Exocrine Pancreatic Insufficiency EPI, And Acute Pancreatitis In Your Dog
Ron Hines DVM PhD
What Occurs When My Dog Has Pancreatitis?
Pancreatitis in dogs occurs in two forms, a sudden attack that can be quite frightening, or a long-term problem called exocrine pancreatic insufficiency or EPI in which portions of your pet’s pancreas no longer function adequately.
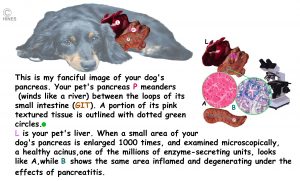
Your dog’s pancreas has the same functions that our pancreas has. It is a pale pink organ with two very different functions and two different areas of inter-dispersed tissue types – each with one of those responsibilities. One of those tissue types in your dog’s pancreas, the acinar portions, produce enzymes to be released into your pet’s intestine to help it digest and absorb the food it eats. Damage to that portion is what is responsible for the sudden (acute) pancreatitis that sometimes occurs. (read here) The other tissue areas of your dog’s pancreas, the islets of Langerhans, produce the hormones that regulate how your dog processes those nutrients once they are absorbed. Those areas secret insulin, glucagon and somatostatin, an inhibitor of the first two. Both portions of the pancreas are critical to your pet’s well-being. You can enlarge my second diagram at the top of this page to see the anatomy of the problem better.
The degree of inflammation in pancreatitis in dogs is unpredictable. It can be very mild, it can be substantial, or it can be severe. All degrees occur. The inflammation can begin suddenly, or it can be a smoldering chronic problem. Pancreatitis can be progressive, or it can remain a minor, manageable issue that you and your pet deal with periodically during its life. When signs are mild and barely noticeable, you might ignore them or, more likely, attribute it to something else. Maybe a snack that didn’t agree with your pet, a tipped over trash can, an upset in its daily routine or a trip to the veterinarian or groomer. Some studies report that perhaps 2 out of 135 dogs will develop a noticeable pancreatic problem sometime in their lives. Probably a lot more with pancreatic issues are never noticed.
The Acute Or Sudden Form Of Pancreatitis
There are two forms of pancreatitis, a smoldering long-term problem and a sudden substantial attack. It is the acute attacks that are the most frightening to dog owners. They are also the most dangerous; so they are the most described online and in scientific publications. Acute pancreatitis attacks appear to be quite painful. They begin with little warning. As I mentioned, the pain they produce is due to the abdominal inflammation generated by leaking pancreatic enzymes.
What Signs Might I See If My Dog Has An Acute Pancreatitis Attack?
You might observe recurrent bouts of cramping, abdominal pain and tenderness. Many dogs in this situation arch their backs uncomfortably and are reluctant to move or play. Usually, they have little or no appetite. Transient depression often accompanies these attacks. However, these signs are not specific or diagnostic for pancreatic issues. All the signs I mentioned accompany a large number of digestive tract health problems that do not involve your dog’s pancreas.
As I mentioned, acute attacks tend to come on suddenly. Some dogs pant and most appear worried. Your dog might vomit. It might develop diarrhea (sometimes with blood). Some run a fever. Vomiting, diarrhea, fever, and a lack of interest in drinking all lead to dehydration and blood electrolyte imbalances. In serous attacks, your dog’s pulse might be rapid and/or weak. Dogs in those situations need immediate hospitalization because they can go into shock (vascular collapse) or even develop a life-threatening condition called DIC.
An inflamed pancreas leaks digestive enzymes that were intended to enter your dog’s upper intestine to digest its food. These nine enzymes, are quite corrosive to living tissue when they are activated in the wrong place. So, when the outlet channel (the common bile duct) from your dog’s pancreas to its intestines is blocked or inflamed, or when pancreatic tissues are disturbed, those corrosive enzymes activate in the wrong place. That causes severe pain and inflammation in the surrounding tissue. If the leakage is severe enough, toxic remnants of the destroyed tissue can enter your pet’s blood stream, causing body-wide alterations and damage. Luckily, cases that severe are infrequent.
The majority of dogs that develop acute pancreatitis are middle-aged to elderly, although the problem may have been brewing since much earlier in their life. When the problem develops in a younger dog, often due to its genetics, it is not unusual for a single dog to have multiple digestive tract issues in addition to pancreatitis. (read here) Dogs that are already suffering from diabetes, Cushing’s diseases or hypothyroidism also have increased chances of developing acute pancreatitis. (read here)
Until recently, when your dog experienced a bout of acute pancreatitis, your veterinarian was limited to providing your pet with supportive care, such as IV fluids, pain medications, anti-vomiting medications, intestinal rest and, perhaps, a very bland, liquid diet if your pet was still capable of receiving it. But in 2022, the FDA gave conditional approved a new pancreatitis medication for dogs, Panoquell®-CA1 (fuzapladib). It is hoped that this medication might lessen the damage caused by acute attacks of pancreatitis. Panoquell-CA1 became a Ceva Pharmaceuticals product in 2023, but the same medication has been available for dogs in Japan since 2018. Panoquell®, is an injectable drug intended to be used by your veterinarian while your dog is hospitalized for treatment of a sudden (acute) bout of pancreatic inflammation. Common factors that might increase the chance of your dog developing acute pancreatitis are eating foods that it does not normally receive – particularly fatty meat scraps. It has also occurred as a side effect of certain medication such as corticosteroids or in combination with diabetes mellitus, Cushing’s disease or obesity. As I mention elsewhere in this article, some miniature schnauzers are affected by a genetic defect, (mutation of the PSTI gene) that makes them susceptible to pancreatic issues. (read here) Possible side effects of Panoquell®/fuzapladib mentioned by the Company are loss of appetite, digestive tract disorders, respiratory tract disorders, liver disease and jaundice.
When Pancreatitis Becomes A Chronic Problem – Exocrine Pancreatic Insufficiency – EPI
I mentioned earlier that although it is possible, repeated attacks of acute pancreatitis are not the most common cause of lasting pancreatic damage in dogs. The most common cause is a genetic propensity of certain dog breeds to lose their ability to produce these digestive enzymes (exocrine pancreatic insufficiency = EPI). Veterinarians believe that in these breeds there is a tendency to develop a type of autoimmune disease directed primarily against portions of their own pancreas. Their immune system mistakes the dog’s own pancreatic tissue for something foreign that needs to be destroyed. This genetic defect occurs most often in German shepherds, chows, cavalier King Charles spaniels and rough-coated collies. (read here) You are unlikely to see signs of this autoimmune disease until a majority of your dog’s digestive enzyme producing ability has already been lost. At that point, weight loss, a dull hair coat, increased gas, soft clay-colored, oily stools and perhaps diarrhea are the symptoms most commonly observed. Although those are the more common signs of EPI, a few dogs do not lose weight – at least not initially, stool appearance is variable and appetite is also quite variable between EPI dogs.
The vast majority of cases of chronic pancreatitis in dogs are thought to be due to autoimmune disease. But repeated bouts of acute pancreatitis can also eventually scar your pet’s pancreas to the point that it can no longer produce sufficient digestive enzymes. Both result in Exocrine pancreatic insufficiency (EPI) – a lack of sufficient pancreatic digestive enzymes. When that occurs, your dog might lose weight. That is because it is no longer able to digest and obtain enough nutrients from the foods it eats (=maldigestion-malabsorption syndrome). (read here) The color and consistence of your dog’s stool usually changes too – often to a lighter color. Lacking sufficient lipase, your dog’s stools tends to be greasy and more fluid. In cases where inflammation persists, the possibility even exists that the insulin-producing islet portions of the pancreas will no longer produce sufficient insulin (=diabetes). However, that outcome is quite rare.
An occasional mistaken is to confuse a dog with a pica problem for one with a pancreatic problem, although many dogs have both. Pica in veterinary medicine is the desire to eat non-food items. That could be leaves, twigs, stones, rotten edibles or the stools of other animals, etc. Pica has a large psychological element in it. Pancreatitis does not. Indigestion, colic, and diarrhea are common in dogs with both problems. (read here) That is why I always have dog owners bring me several stool samples and pass them through a fine sieve looking for debris (e.g., aluminum foil, Col Sanders remnants, wood, plastic, cloth, etc.). Pica can also be exacerbated by digestive tract issues such as inflammatory bowel disease.
Why Did This Happen To My Dog?
In the majority of cases, your veterinarian will never discover why your dog developed acute pancreatitis. It does appear that the pancreas of many pet’s malfunctions when it is exposed to too high a level of circulating lipids (fats=triglycerides). That can be due to a diet too rich in fat, due to obesity, a lifestyle of inactivity, or specific diseases and genetic mistakes that elevate the lipid/fat content of your pet’s blood. (read here)
In some miniature schnauzers, a genetic defect, (mutation of the PSTI gene) appears to be responsible for their high blood lipid content. Subsequent attacks of pancreatitis (familial hyperlipidemia) is a common result. (read here & here) Dachshunds, Yorkshire terriers, Silky terriers and Skye terriers seem to develop more than their fair share of pancreatitis too. No one knows why, but we do know that lapdogs tend to be indulged by their owners. That is particularly true when it comes to their diets. We see cases of pancreatitis more frequently in neutered/spayed dogs than in intact dogs – probably because neutered/spayed dogs tend to become more obese and because of the many negative effects that early age neutering has on their metabolism. (read here)
In some cases, abnormally high (or low) blood calcium levels (also read here), certain antibiotics, diuretics, anti-epileptic medications (read here) or anti-cancer drugs (read here) might have contributed to the onset of pancreatitis. However, it is never clear if it was the medication given that caused the pancreatitis or if it was the disease that the medication was being given for that did.

What Tests Will My Veterinarian Perform?
The most accurate tests to detect acute pancreatitis are thought to be the trypsin-like immunoreactivity test (TLI) and the cPL test. (read here) However, neither test is infallible. (read here) A higher than normal TLI result suggests acute pancreatitis. A lower than normal TLI result suggests chronic pancreatitis (EPI). You can read a very long-winded article that includes diagnostic avenues here. Although presented as the “gold standard consensus statement”, there really is no consensus when it comes to diagnosing and treating chronic pancreatitis in dogs.
If your pet arrives at the animal hospital during an acute pancreatitis attack, many more tests will need to be performed. (read here & here)
What Are My Options If My Dog Has Been Diagnosed With EPI?
An Enzyme Supplement
Because your dog can no longer manufacture sufficient digestive enzymes, you must supply them yourself. Some common brands are Viokase-V™, Epizyme™, Panakare™, Pancrepowder Plus™, PancreVed™, and Parcrezyme™. Powders, granules, capsules, and tablet forms are available. Specialist suppliers also exist that market raw ground beef pancreas. Some believe that coated enzyme products protect the ingredients from stomach acids. Others disagree. Since each EPI dog is unique, it is up to you to judge the value of an assortment of these products for your dog. That is not something your veterinarian can do for you. While on a specific brand, is your dog’s stool more formed? Does the stool appear better digested without identifiable food particles? Is your dog’s weight increasing? Is its hair coat more lustrous and less scurfy? What about its energy level? The dose and frequency that your dog will need these enzyme supplements is also quite variable.
A Diet Change
Many popular dry adult dog food brands are about 28-30% protein, 20% fat and 3% fiber. Dogs with EPI generally do better and have better formed stools on diets that seek meat protein of a higher quality and digestibility than was meets minimum AAFCO standards. In my opinion, that should be restaurant-quality meat. Most dog food suppliers will dance around that question when you ask them. The only way to be certain of what is in your dog’s food is to make it yourself. (read here) That requires quite a bit of dedication and time. So few folks with EPI dogs attempt it. Instead, they rely on major dog food manufacturers of prescription diets or niche marketers.
If preparing your dog’s food at home is not an option, I prefer that you use the products produced by major dog food companies, such as Hills Prescription diet i/d™, Purina EN™ or Royal Canin’s Gastrointestinal™. Too many additional ingredients with no valid reason for being there are always warning signs. It means that the Company’s advertising department, rather than their nutritionists, have had a hand in the formula – things like apple pomace, cranberries, dried kelp, chicory root, alfalfa, etc. Those ingredients probably won’t hurt your pet, but they are unlikely to benefit him/her either. When “grain free” means that legumes have been substituted for ingredients such as corn, wheat, barley or oats, some veterinarians and the FDA have associated those formulas with canine heart issues. (read here)
The smaller the capitalization of the manufacturer, the less likely they are to have trained veterinary nutritionists on staff or to do a thorough analysis of each batch of their ingredients. You can also buy ready-made, freshly prepared canine diets in raw, cooker or frozen form. But you’ll never know if the particular batch that you bought was contaminated or if a formulation error was accidentally made.
Name brand dry commercial diets suggested for dogs with EPI vary from about 22-24% minimum crude protein content, 7-12% minimum crude fat, 3.5-5% crude fiber, 1.8-4% maximum fiber and 10% water. That is a large discrepancy. What that tells you is how little we really know about optimum diets for EPI dogs. It also tells you that gastrointestinal diets need to be tailored to the individual dog. If it works for your dog, it is the right diet. If not, it’s the wrong one. In addition, do not hope for a full cure. Diet can improve your dog’s digestion, but it and enzyme supplements almost never cure the problem entirely.
Unfortunately, the ingredients list on your dog food doesn’t always tell you what type of fiber the diet contains. There are two different types of fiber, soluble and insoluble. Soluble fiber dissolves in the liquids in your dog’s intestine, forming a gel-like substance that beneficial bacteria feed on. That has been found to be helpful in some cases of EPI. However, insoluble fiber, such as the fiber in beans, peas, potatoes, bran and vegetables, remain unchanged as it moves down the dog’s digestive tract. You can see from the 1.8-4% fiber spread that even veterinary nutritionists have no consensus opinion on that. Another effect of higher fiber diets is that they can adsorb and make unavailable portions of the pancreatic enzyme supplement you are providing. Fiber has the potential to do the same thing to any B-complex vitamin products you add. How important that might be remains unknown. So, the best advice I can give you is to try your choice of EPI diets and observe the effects. Hopefully, the same positive signs I mentioned in enzyme supplements, weight gain, a more formed, more normal color and better-digested stool, less flatulence, less steatorrhea, and laboratory test results closer to normal will occur. Some dogs with EPI eat bizarre items, others eat poop. If your pet has that inclination, a decrease in its occurrence is a very positive sign that more important nutrients and vitamins are now available.
As you can see, there is no agreement as to the optimal fat content of diets for EIP dogs either. (read here and here)
A Vitamin Supplement
B-complex vitamins are all water-soluble. When food passes too rapidly through your dog’s intestines, or when the small intestinal lining is disturbed, insufficient amounts of those vitamins might be absorbed. Vitamin B12 (cobalamin) is commonly deficient in dogs with EPI. In those cases, weight loss, wasting, low-energy level and malaise are common signs. Anemia can be a sign of a B12 deficiency as well. Normal blood levels of vitamin B12 in dogs are 251 – 908 ng/L. B-12 interacts with vitamin B9 (folate). In some EPI dogs, blood folate levels are low, in others they are increased above normal level. The Gastrointestinal Laboratory at Texas A&M University can measure your dog’s B12 and folate blood levels. They suggest your dog begin a B12 supplement when its level of that vitamin is <400 ng/L. They recommend that dogs under 22 lbs/10 kg receive 250 µg per day, dogs from 22-100 lbs/10-45 kg, 1000 µg per day.
How and if the absorption of fat soluble vitamins, trace elements and minerals is affected by EPI in dogs is unknown. The absorption of fat soluble vitamins is aided by the fat content of your dog’s diet. However, only a very small amount of fat/lipid is needed to aid absorption. One must be cautious when adding additional vitamin A and D to your dog’s diet. Too much of either vitamin causes health issues. (read here & here)
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.