Kidney Disease In Your Cat
Chronic Renal Failure (CRF, CKD)
Ron Hines DVM PhD
 Update On Kidney Disease In Your Cat & Its Treatment
Update On Kidney Disease In Your Cat & Its Treatment
 The SDMA Kidney Test – What Results Mean
The SDMA Kidney Test – What Results Mean




All of the body’s organs suffer the wear and tear of time. In you and me, it might be our hearts that are our weakest organ. Heart disease is #1, and kidney disease is #10 on the list of causes of human mortality. No one has added up the numbers for cats, but I suspect the two leading issues would be reversed. In cats in the United Kingdom, kidney disease is only surpassed by car accidents and feline heart disease is #8 :

A study by Banfield Pet Hospitals reported that at their clinics, kidney disease was 7 times more common in cats than in dogs. One out of every 12 senior cats presented to them had some evidence of kidney problems. When the diagnosis was made at a point early in kidney disease, cats treated at Banfield lived an average of 2–3 years past that point. When cats were brought in later in their disease (blood creatinine >5.0 mg/dl = >440 µmol/l) they lived fewer than six additional months. Twenty-nine percent of the cats that arrived due to their kidney problems also had tooth and gum disease (periodontal disease). How, or if, one of those two problems contributed to the other remains unclear. The same general relationship exists in people. (read here)
What Is Happening When My Cat’s Kidneys Fail?
First, you need to know something about the critical work that your cat’s kidneys perform. Their primary job is to keep its body free of the wastes that accumulate during the normal, everyday metabolism of cells. Your cat’s kidneys are continually cleansing its blood of excess salts, water, metabolic residues and toxins and depositing them in its urine for elimination.
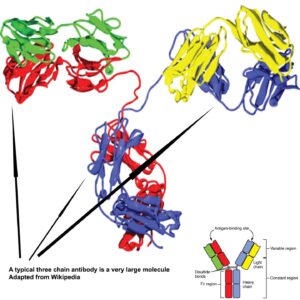
The actual removal of wastes occurs in tiny, multiple structures within your cat’s kidneys called nephrons. There are almost one million of these structures in a single human kidney. How many nephrons there are in a normal cat’s kidney is unknown. Each nephron contains a small sieve-like filtering structure called a glomerulus. These glomeruli (plural form) prevent normal blood proteins, blood cells and critical constituents of the bloodstream from escaping into your cat’s urine, while allowing extra fluid and wastes to pass through, to eventually end up in your pet’s urine. A complicated chemical exchange takes place, as waste materials and water leave the blood and enter the urinary system.
That requires very specialized gatekeeper cells. They are called podocytes. Throughout the animal kingdom, highly specialized cells are never good at repairing themselves or regenerating new ones once they have been injured. Take brain cells, for example. Once a neuron is lost through aging or disease, a new neuron does not take its place.
Your cat’s kidneys also regulate its body’s acidity and, through regulation of body salt/electrolyte content, its kidneys help control your cat’s blood pressure. Cells associated with healthy nephrons produce an important hormone called erythropoietin and an enzyme called renin. Erythropoietin is necessary for your pet’s body to manufacture and maintain red blood cells, while renin activates another hormone (angiotensin) to helps control your cat’s blood pressure. In addition, healthy kidneys are required to convert vitamin D into calcitriol, which preserves calcium reserves in bones and maintains normal calcium balance throughout the body. In chronic kidney disease, these glomeruli have been scarred and lost, or plugged up with proteins and inflammatory cells. Without enough functioning glomeruli, none of the processes I mentioned work normally. You can read about the many regulation processes that occur in the kidney in detail here.
But My Cat Is Still Producing Plenty Of Urine – More Than Before!
Your cat’s body is marvelous in sensing when it has an electrolyte and a waste product buildup problem and attempting to correct it. In its attempt to keep its blood waste-free, the cat’s small number of remaining healthy glomeruli work overtime to remove waste as fast as they can. That accounts for the increased thirst and urination you might be seeing in your cat as its kidney issues progress. For a while, this compensation does keep its body free enough of wastes to function normally. But there will arrive a time when your cat cannot consume enough water to keep those waste levels in its blood under control. That is the time your veterinarian might suggest that fluids be given to your cat by subcutaneous injection. By that time your pet might already be experiencing weight loss, anemia, and abnormal blood work results. When that time arrives, over half of its kidney glomeruli are thought to have been lost. Your pet cannot replace them, and nothing veterinarians have at their disposal today (short of a kidney transplant) can either.
What Might Be Some Of The Signs Of Kidney Disease In My Cat?
Cats with kidney disease tend not to groom themselves as well as they used to. They often have less energy and are less playful. I mentioned that another early sign that often goes unnoticed at first is your cat beginning to drink water and urinate more (polydipsia/ polyuria). It is normal for cat owners to ignore this at first. It might just be that you notice your cat’s litter box is a bit damper and smellier than it used to be. Or that its water bowl has to be filled more frequently. However, kidney disease is not the only cause of increased thirst. Fever, diabetes, severe diarrhea, vomiting, corticosteroid medications or increased salt intake can all produce similar effects. So, you shouldn’t jump to conclusions based on the symptoms I mentioned alone. Laboratory kidney health marker tests need to be performed. Less playfulness and less energy in elderly cats could also be due to arthritis, cognitive decline, or one of the many other afflictions associated with aging. (read here)
As the problem advances, cats with kidney issues tend to become finicky eaters and lose weight. Consequently, their energy levels tend to decrease as well. These cats play less, romp less and sleep more. This is often when cats are first taken by their concerned owners to see their veterinarian. An exception are cats that have both kidney issues and hyperthyroidism. It is common for both health issues to coexist in a single elderly cat. Cats experiencing hyperthyroidism also lose weight, but their high thyroid hormone levels (T4) keeps them overly active. Most veterinarians check a cat’s free T4 level before initiating hyperthyroidism treatment because lowering the cat’s thyroid hormone level to normal can leave a cat’s kidney function worse off than before.
In advanced kidney disease, cats sometimes gag as they would if they were expelling fur balls. They may experience other digestive disturbances such as nausea and diarrhea. At that point, apathy and illness cause their water intake to decrease, so dehydration becomes an issue. Your cat might stand over its water and/or food bowl without attempting to drink or eat. These cats have developed uremia, also called azotemia, an intolerably high level of nitrogen-containing metabolic waste products circulating in their bloodstream.
Why Did My Cat’s Kidneys Fail?
Veterinarians know a lot about the things that will make your cat’s kidneys fail suddenly: an obstructing kidney stone(s), other blockages preventing the passage of urine, something eaten that was toxic such as lilies, ibuprofen, or another NSAID, certain antibiotics, moldy cat food ingredients, or cat food vitamin errors. Perhaps, in some cases, chronic, lower dose exposures to those things were contributing factors. Veterinarians do not know. Genetic defects in inbred cats are another possible cause. But all cats experience some degree of kidney decline as they age, just as we do. Neither veterinarians nor physicians have an explanation as to why that occurs, or why it occurs more frequently in cats than in dogs or in humans. Human nephrologists ponder the same questions. (read here) Many causes of kidney decline have been discussed that seem logical, but none of them have been proven to be true. The most recent theory concerns kidney damage in cats as being a possible long-term result of an infection by a very common feline morbillivirus (FeMV). (read here)
Regardless of the cause(s), all cases of chronic kidney disease develop the same signs and pass through the same stages. Usually, your veterinarian will just tell you after a routine health screen that your cat has early blood indicators of CRF (chronic renal failure). That is because in most cases, there is no way for your veterinarian to determine the original cause. The exception is polycystic kidney disease that I mentioned as a genetic defect.
More On The Wear And Tear Of Time
There was a time, not so long ago, when infectious diseases and dietary deficiencies ended the lives of many cats prematurely. That is still true in the less prosperous areas of the world. But with advances in vaccination, cat nutrition, antibiotics, and, most importantly, indoor living, cats now have the potential to live much longer. Nothing lasts forever, and every organism has its weakest link. I mentioned that the crucial cells of your cat’s kidneys, the podocytes, cannot replace or regenerate themselves as the other crucial cells in its liver, bone, and skin can. Once podocytes, or other tubular cells, are lost and replaced by scar tissue, they are lost forever. When you have a “wellness” checkup on your 15-18 year old cat and are told that laboratory tests (e.g., BUN, creatinine, SDMA) point to kidney disease, you could just as well have been told that you are the owner of an old cat. When Idexx came up with their patented SDMA test, Antech Laboratories felt compelled to come up with some other “marker” of kidney decline of their own:
*************************
*************************
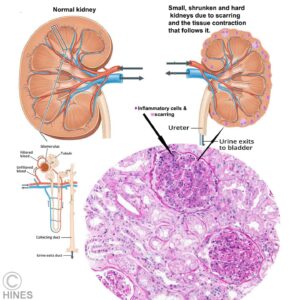
Chronic interstitial Nephritis
Chronic interstitial nephritis is the pathologist’s term for the microscopic damage seen in the most common forms of kidney disease in older cats and older dogs. It is thought to be the end result of many different chronic kidney inflammatory processes – not just one. The tissue that surrounds and supports your cat’s nephron filters is called its interstitial tissue. It is the matrix that suspends the nephrons and gives shape to the kidneys. Pathologists that examine kidney tissue from pets with failing kidneys have noticed that many of these pets have a higher than normal number of inflammatory cells (your cat’s WBCs) invading the interstitial area. This low-grade, chronic inflammation is thought to be the cause of the scaring that eventually destroys most of the pet’s nephrons. What draws these inflammatory cells to the kidneys remains unknown.
Cats suffering from advanced chronic interstitial nephritis, like the fanciful one I drew in the diagram above, have small, shrunken and abnormally firm kidneys due to scar tissue buildup and the shrinkage and contraction that follows it. If your cat is mellow and not too chubby, it would be easy for me (or for you) to palpate and identify these shrunken, firm kidneys during a routine veterinary exam. Some veterinarians once associated chronic interstitial nephritis in dogs with a possible exposure to leptospirosis carrying rodents. Leptospirosis is quite rare in cats. You might think that it would more common, since rodents are their natural prey. So, most veterinarians believe that it is unlikely to account for the type of chronic kidney damage we see in older cats. Others disagree. (read here)
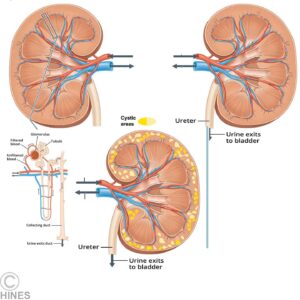
Polycystic Kidney Disease
I mentioned polycystic kidney disease earlier. Cats with polycystic kidney disease inherited a gene that causes fluid-filled sacks (cysts) to form within their kidneys and various other organs. As these cysts gradually grow in size, they crowd out and destroy the functional tissue (nephrons) within the pet’s kidneys. This is rarely, if ever, a disease of rescued kittens sired by the dominant neighborhood tom. The defective gene responsible dwells most frequently in show cats. It was originally reported in those of Persian cat ancestry, but now appearing sporadically in exotic and British and American shorthairs, Himalayans, Main Coon and other less common cat varieties. (read here). Being a dominant defective gene trait, it only takes one bad gene, rather than two, to cause the cat’s kidneys to fail. If an unborn cat embryo inherits a defective gene from both its queen and its tom, it will die before birth. Cat breeders tend to be reticent in revealing skeletons that reside in their closets. One of the many reasons for you to obtain your next cat from your neighborhood rescue. Random bred house cats have a larger and healthier gene pool. (read here)
Chronic Over-stimulation Of Your Pet’s Immune System
Your cat’s kidney glomeruli act as sieves, straining and filtering blood as it passes through them. Very large molecules, such as antibodies, in the blood stream have a tendency to become trapped there. Some of those antibody types may be drawn there due to processes we do not understand. Others may simply become tangled in the glomerular structure. When large numbers of antibodies are present in the kidney’s cortex, they appear to slowly damage its filtering ability. Some of these large molecules are antibodies that are already combined with antigens (=immune complexes). Many chronic infectious and autoimmune diseases produce these immune complexes. They include bartonella, chronic skin infections and chronic intestinal disease.
Among these rare causes of kidney failure in cats is another situation where destructive proteins sometimes accumulate in the kidneys. The material is called amyloid (amyloidosis). In some cats, this is a genetically transmitted disease. But it has also been known to occur after long-term over-stimulation of the immune system. Abyssinians and Siamese cats have a higher than normal incidence of amyloidosis that, in some, leads to kidney failure. (read here) A similar form of kidney damage in pets occurs in autoimmune diseases that are similar to the lupus complex in humans. In this disease, run-away antibodies are produced against the pet’s own body. In some cases, these antibodies are directed at the pet’s kidneys, in others, they may only accumulate there, causing mechanical obstruction and damage.
Hyperthyroidism
An overactive thyroid gland, hyperthyroidism, is a common problem of older cats. Veterinarians are uncertain why it occurs in cats more frequently than it once did. The three most mentioned possible factors are the consumption of ocean fish-containing cat foods (they can be high in iodine), and PBDEs and PCBs, which are also found as contaminants in ocean fish – particularly in the cheap fish residues that end up in cat food. (read here & here) But what we do know with certainty is that hyperthyroidism in cats often occurs concurrently with kidney disease. Hyperthyroidism often masks the signs of kidney failure, making the results of blood tests appear less serious than they actually are. It is only when your veterinarian resolves your cat’s thyroid problem that it becomes apparent that the cat’s kidneys had already lost much of their blood-cleansing ability.
Most veterinarians believe that hyperthyroidism might also cause your cat’s blood pressure to be abnormally high. No studies in cats have ever been conducted, but veterinarians assume it might occur based on studies in hyperthyroid people. (read here) We also know that high blood pressure often leads to kidney failure in humans. Perhaps that is why hyperthyroidism and kidney failure go hand-in-hand in cats. The biggest problem is in getting accurate readings of your cat’s blood pressure during your veterinary hospital visit. Blood pressure readings in cats are notoriously inaccurate. (read here & here) If your cat was diagnosed as having an overactive thyroid gland, its heart and kidney function need to be carefully scrutinized. Of the tests currently available, I rely on the microalbuminuria test of your cat’s urine, considered along with its other urinalysis results, as being the most sensitive for detecting the possibility of early kidney damage related to elevated blood pressure. A cat’s “normal” blood pressure increases slowly as it ages. That is due to loss of elasticity (increased stiffness) of the collagen of its vascular system – the same occurs when we get skin wrinkles.
Lower Urinary Tract Disease
Feline Urological Syndrome (FUS/aka FLUTD) is another urinary tract issue. It became common as more and more of our cats lived their lives indoors, with little interest in exercise or reproduction, and with unlimited access to calories. When a cat develops FUS, a pasty grit (struvite crystals) irritate it bladder lining. This material also has the potential to forms plugs in the urethra of male cats. These plugs in male cats, or more discrete stones in both sexes, can prevent normal urination and increases urine pressure in its bladder, ureters, and kidneys. Abnormally high urine pressure in a cat’s kidneys slowly destroys them. This situation is called hydronephrosis. Obstructing urinary tract stones (aka calculi) and urine flow blocking defects in the cat’s ureters are other possible causes for loss of kidney function. When caught early, the vast majority of cats that suffered from a bout of FUS do not show changes in their kidney function once the blockage has been removed.
How Do Veterinarians Diagnose Kidney Disease In Cats?
The history you give your veterinarian, your cat’s age, and your veterinarian’s physical examination often lead your vet to suspect a chronic kidney problem. As I mentioned, as glomeruli are replaced by scar tissue, its kidneys become smaller, harder and lumpy (pitted). In lean cats, these kidneys have a characteristic feel and shape when felt (palpated) through the cat’s abdominal wall or when observed using renal ultrasound or x-rays. A standard blood chemistry and urinalysis panel usually confirms these initial suspicions. Bringing your cat in for its examination on an empty stomach also makes successful kidney palpation considerably easier. Fearful or aggressive cats might need calming medications.
Your Cat’s Urine’s Specific Gravity SpGr
Veterinarians often request that you to bring them a urine specimen from your cat, so that its specific gravity and its constituents can be determined. (read here) Placing some Saran wrap™ over your cat’s litter might make urine collection easier. Purchasing non-absorbing plastic beads that replace the litter is considerably more successful. For certain other analysis, it is better if your veterinarian collects the sample by expressing your cat’s bladder or through a urinary catheter. Specific gravity measurement tells your veterinarian how concentrated the urine sample is. Cats that have weakened kidneys can no longer produce concentrated urine. So, its urine specific gravity, a measure of concentration, is low. Cats with normal kidneys produce urine with a specific gravity of about 1.015 to 1.060. When your cat’s kidney nephrons have suffered substantial damage, the urine your cat produces is essentially the same as its blood plasma’s specific gravity, minus the blood’s protein content. (= isosthenuric urine = <1.015 SpGr) The lower your cat’s first-of-the-morning specific gravity is, the more serious its kidney problem is likely to be. Later in the day, water your cat may or may not have consumed clouds the meaning of the results. Some veterinarians insist on withdrawing urine from your cat’s bladder with a needle and syringe by penetrating its abdominal wall (cystocentesis). Unless they plan to submit that urine for bacterial antibiotic sensitivity testing or when your cat’s urethra is blocked, there is really no indication or need for that. Would your urologist do that to you? Urine samples obtained that way often report the false presence of blood in the urine.
Your Cat’s Urine Protein Content And Microscopic Urine Examination
Failing kidneys leak blood proteins into your cat’s urine. Most of that protein is albumin. Although a urinary tract infection or sudden trauma can also cause high urine protein content, excess urine protein is often an early warning sign of long-term kidney damage in older cats. The presence or absence of white and red blood cells and debris in the urine specimen help your veterinarian tell the difference between sudden (acute) urinary tract damage and chronic (long-term) kidney disease. Of the many tests available to detect protein in the urine, the urine microalbuminuria test appears to be the earliest test to give accurate warning of a pending kidney issue.
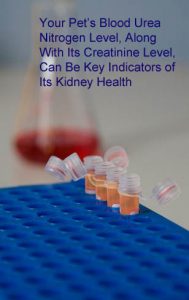
Your Cat’s Blood Urea Nitrogen (BUN) Level
Blood urea nitrogen (BUN) is a waste product generated by all cell level metabolism as proteins are assembled and disassembled. Your cat’s liver creates the BUN from ammonia-containing residues as the safest method to convey those residues through its bloodstream, and to its kidneys for elimination in your cat’s urine. The urea ammonia in BUN is what gives the pee in your cat’s litter box its distinctive odor. BUN levels stay within a relatively narrow range in the blood of healthy cats – although it fluctuates during the day, depending on your cat’s ingestion of high-protein meals and hydration status. BUN level in the blood of kidney-problem cats begins to rise when not enough healthy kidney tissue remains to excrete it into the cat’s urine. The higher its persistent level remains in your cat’s blood – the more serious its kidney problem is likely to be. The blood urea nitrogen and creatinine results in your cat’s blood profile are also the prime ways veterinarians decide if their treatment of kidney disease in your cat is working. You will have many of those tests run on your pet during therapy.
Your veterinarian knows that lack of hydration, over-hydration, impending heart or liver failure, urinary tract obstruction, high-protein diets, fasting and vigorous exercise also influence your cat’s BUN (and SDMA) levels. Your cat’s other blood panel results as well as your veterinarian’s physical examination of your cat and the history you provide will help him/her rule those other causes out one-by-one.
Your Cat’s Blood Creatinine Level
I mentioned that your cat’s BUN level can have substantial daily fluctuations. In a veterinary research setting, your cat could have many repeated BUN blood tests run throughout the day, and they could be averaged. But that would be asking a lot from your cat. It’s impractical, it’s expensive, your cat would be quite upset, it probably would not drink or eat, so the results would be meaningless. However, non-specific, throughout-the-day, fluctuation are much smaller when it comes to creatinine. Like BUN, creatinine is also a waste byproduct of cellular protein metabolism (primarily muscle metabolism). However, creatinine diffuses through your cat’s body slower than BUN. So, its level throughout the day is more stable than BUN (less subject to hourly fluctuations). However, once your cat’s weight begins to drop, its blood creatinine level may actually underestimate the extent of its kidney damage. That is because loss of lean muscle mass causes lower creatinine production. (read here) Sometimes diagnostic laboratories additionally report BUN and creatinine as a ratio, the BUN:Creatinine ratio. That might get around the problem in lean cats. As cats age, many loose muscle mass and consequently, their blood creatinine level is naturally a bit lower. So, as I mentioned, in cats with advanced kidney disease and wasting, the reported creatinine level may not sufficiently indicate the seriousness of your cat’s situation. Some claim that the highly marketed SDMA test avoids this problem. However, your cat’s SDMA level is affected by so many non-kidney issues (read here) that I believe that creatinine is still the best marker of kidney health that veterinarians and cat owners currently have. When it comes to your kidneys, human physicians agree. When last I corresponded with the American Kidney Foundation’s physician team, I was told that they just didn’t feel that the SDMA test was worth performing.
Your Cat’s Blood Phosphorus & Calcium Levels
Bones are primarily composed of a combination of calcium and phosphorus, hydroxyapatite. But much smaller amounts of both calcium and phosphorus are also essential mineral constituents of blood that perform multiple functions. (read here) The foods your cat prefers (meat and fish) are naturally high in phosphorus. A cat with failing kidneys has difficulty preventing unintended leakage of blood calcium or disposing of excess phosphorus into its urine. Healthy kidney tubules reabsorb almost all the calcium that escapes through your cat’s kidney’s filtering units. Calcitriol, a form of vitamin D manufactured within healthy kidneys, is also necessary for the proper absorption of calcium from your cat’s diet and for the release of calcium stored in its bones. So, an elevated blood phosphorus level in your cat, often another worrisome sign of failing kidneys. Phosphorus and calcium exist in tandem in you and your cat’s body. As one goes up, the other goes down. So as the ratio of phosphorus to calcium in its blood becomes abnormally high, your cat’s bones will weaken as they are leached of calcium. That is why cats in kidney failure need to be fed diets that are lower in phosphorus or given oral phosphate binders, or both. Your cat’s parathyroid glands are its natural regulators of its blood calcium and phosphorus. Sensing an imbalance, they increase their production of PTH. In cats with healthy kidneys, PTH corrects calcium:phosphorus imbalances by regulating kidney calcium and phosphorus excretion. But in cats with failing kidneys, this system breaks down.
Your Cat’s Blood Potassium Level
Proper internal levels of potassium are very important for your cat’s well-being. When a cat’s kidneys fail, its body potassium level tends to drop. The primary sign of this problem, called hypokalemia, is muscle weakness. These cats are often slow to rise and wobbly in their gait when they do. Holding their head properly erect becomes an effort. Picky eating, depression, constipation, a lack of interest in grooming and scruffy hair coat are also common. But it is hard to know if those issues are due to low blood potassium or another of the many imbalances and toxicities that accompany kidney failure. A few cats reach a point where they no longer produces sufficient urine. In those situations, its blood potassium level can actually rise too high (hyperkalemia).
It is very important that your cat eat enough to maintain a healthy body weight. If it doesn’t like the taste of the food your animal hospital provides – make the diet yourself (best accomplished with the aid of a veterinary nutritionist). In kidney disease in cats and people, body weight maintenance and longevity go hand in hand. The most important characteristics of a good kidney diet are that your cat finds it tasty, that it fulfill your cat’s vitamin/mineral needs, that it be as low in phosphorus as possible and that it not furnish protein in excess of what your cat requires to maintain good muscle mass. You might also experiment with Elura®, although many cats dislike its taste.
Your Cat’s Packed Cell Volume (= hematocrit, Hct, PCV)
Your cat’s packed cell volume (PCV) is a measure of the volume % of its red blood cells in its whole blood. Cats in kidney failure commonly have a PCV that is abnormally low. That it is usually because it is no longer manufacturing sufficient red blood cells in its bone marrow. One of the hormones involved in red blood cell formation is produced in its kidneys. It is called erythropoetin. When your cat’s kidneys deteriorate, not enough of that hormone is produced. The buildup of circulating toxins when kidneys fail (uremia) also decreases your cat’s ability to produce new red blood cells in its bone marrow. Cat’s that are not consuming sufficient water become dehydrated. Dehydration that often occurs in advanced kidney failure falsely increases PCV as the cat’s blood “thickens”. But in those cases, blood sodium content should be above normal as well.
Your Cat’s Blood Pressure
Your veterinarian will probably also measure your cat’s systolic blood pressure. Your cat’s systolic blood pressure is the first (highest) number – the second number (its diastolic pressure) is difficult to accurately obtain in cats with the in-office technology that veterinarians currently have. Abnormally high blood pressure (hypertension) is thought by many to be common in cats with chronic kidney disease. We know that occurs in humans, it is less well documented in cats. It is also unknown if high blood pressure is one of the causes of your cat’s kidney damage, or if it is the result of its kidney damage (secondary hypertension).
What limits your veterinarian’s usefulness of the results he/she obtains is your cat’s trip to the animal hospital. BP readings at animal hospitals – even when performed several times and averaged – are highly untrustworthy and may have little to do with your cat’s blood pressure at home in a more relaxed situation. The White Coat Syndrome. is considerably more profound (intense) in cats than in people. Read more about this problem here. That is why I suggest that you have your veterinarian check your cat’s blood pressure regularly during its lifetime and keep notes so that your vet, and you, have a historical record to compare it to. It is also normal for blood pressure to creep upward as a part of the normal aging process. (read here)
What Treatment Options Are Available For My Cat?
In the future, we might be able to regenerate failing organs. But for now, there is no known way to mend damaged kidneys. What veterinarians can attempt to do is to slow the rate at which your cat’s kidney tissue is lost, and deal to with the side effects of that loss. Kidney failure is a progressive disease. That means that with time it will become worse. The key to gaining time for your cat is to use its remaining functional kidney tissue as efficiently as possible. We try to do this through diet, medications and, when necessary, fluid injections (diuresis).
A Specially Formulated Diet
Commercial diets, designed for kidney failure in cats, are a bit lower in protein than ordinary cat food. Dogs can tolerate lower protein diets better than cats can. These “renal” feline diets also have added omega-3 fatty acids and compounds such as potassium citrate to counteract body “over-acidity “. Most importantly, they are considerably lower in phosphorus. Some are marketed as “early stage” renal diets, with a different, even lower protein content recipe for “end stage” kidney failure. That any of these diets extend the lives of cats is difficult to prove. Studies that would confirm or refute their value would require animal experimentation on cats that is no longer permitted in the developed world. We have some positive data coming from the manufacturers. But the cats they followed were on a variety of medications and led differing lifestyles as well, making it quite difficult to decide what, if anything, was yielding increased lifespan. What I do believe is that these diets cause no harm. They all meet the AAFCO’s trade group’s nutritional guidelines for cats.
Although there is no scientific data that pertains to cats, these commercial-prepared feline kidney diets usually follow current trends in human diets and limit the amount of sodium-rich ingredients. As I mentioned, they also add omega-3 fatty acids, usually obtained from fish oil. Some combine that with flax seed omega sources. Extra vitamin E (tocopherols), as antioxidants, are another common addition. Again, no hard data exists, but some believe that these particular fatty acids reduce inflammation throughout the body – perhaps including any inflammation that might be occurring in your cat’s kidneys.
Cats with kidney problems often have poor appetites. They might suffer digestive disturbances as well. Both could limit their absorption of vitamins. So B-vitamins are often given as an appetite stimulant and to ward off any B vitamin deficiencies they might have. I mentioned earlier that for your cat to convert sufficient vitamin D into its active form, calcitriol, it needed sufficient healthy kidney tissue. Unfortunately, the doses of calcitriol supplement suggested for cats by various sources and suppliers differs enormously. Too much vitamin D is toxic. (read here) You are always safe to go with the dietary suggestions for cats in renal failure of Dr. Chew at Ohio State University. (read here)
On any of these diets, your cat’s body weight and kidney test parameters need to be frequently monitored. It is particularly important that your cat’s blood albumin protein level not drop too low and that your cat’s body weight remains stable. Cats are creatures of habit and often resent diet changes. When you do that, and your pet’s BUN and creatinine levels drop or remain stable, not providing unnecessary protein is a positive step. There are periods in a cat’s ongoing struggle with renal disease when restricting its protein consumption is not a wise thing to do. (For example, when 7/8th of its kidney’s filtering apparatus was removed) (read here & ask me for Madison2010)
Always make your cat’s dietary changes gradually. As I mentioned, cats are creatures of habit. Several veterinary schools have nutritionists on staff that will, for a fee, design a homemade lower phosphorus, lower protein diet from ingredients that your cat already enjoys.
You already know that I am not a fan of industrially manufactured cat food – particularly dry kibble. I believe that the most important thing you can do in modifying your cat’s existing diet or preparing a better homemade diet is to slowly increase the amount of added water, up to the limit that your cat will accept. That needs to be done slowly enough that your cat does not catch on. Keep track of its body weight; we do not want body weight to drop in a cat that is thin already. The more water, broths, and fluids your pet consumes (within reason), the more toxic waste products it will be able to flush from its body with the few healthy kidney filtering units (nephrons) that remain. Others find that leaving faucets dripping sometimes encourages drinking, as do multiple water bowls of various designs. You might also explore offering your cat Hydra Care™.
ACE Inhibitor Medications
An ancient organ, as critical to life as the kidney, does not vary much at the cellular level between mammals. Today, experiments in the treatment of kidneys disease are most acceptable to animal welfare advocates when they are performed on rats. The cells that medical research scientists zero in on when kidney function is declining are called podocytes. I mentioned them before. They are highly specialized cells in the kidney’s filtering apparatus that underlie its blood-cleansing abilities. Once podocytes loss begins, like a tree bent to a severe angle by a storm, it will continue to slowly fall even after the winds cease. The kidney’s only remaining option is for its remaining kidney filters, “super nephrons” to enlarge (=hypertrophy) and work harder. There is considerable evidence that, in rats at least, medications called ACE inhibitors slow that podocyte loss. (read here) They do so by easing the passage of blood and lower blood pressure throughout the body – including within the nephrons. The ones most often chosen by veterinarians for cats are benazepril and enalapril.
If your cat is taking an ACE inhibitor, it is wise to be sure that its blood creatinine level does not suddenly spike. In later stage kidney failure, when the remaining kidney filters (glomeruli) are filtering way above their normal capacity, ACE inhibitors occasionally drop a cat’s internal kidney pressure so low that the pet’s uremia actually worsens. The best monitoring test in those situations is a 24-hour creatinine clearance test or another test that estimates your pet’s GFR. But those tests are beyond all but the most sophisticated veterinary college teaching hospitals. Over the years, I have not seen that the outcomes at those advanced veterinary institutions outperform those of your local veterinary practices that specialize in feline medicine.
The most common side effects of ACE inhibitors in cats are said to be stomach/intestinal upsets, constipation and weakness due to too low a blood pressure. I qualify that because these cats are often taking more than one medication, and they are in failing general health. So, it can be hard or impossible to sort out which one or ones of the medications are responsible for side effects. In those cases, the individual medication doses need to be reduced – preferably one by one. Sometimes side effects can be lessened if you begin these medications at a low dose and gradually increase them to the desired dose.
Phosphorus binders
Certain oral products, phosphate binders, block the absorption of phosphorus from food while it is still in the cat’s intestine. At one time, aluminum hydroxide – containing products were commonly suggested. But they are rarely given today because they contain aluminum. Instead, products like Epakitin® and Pronefra® which contain, in addition to calcium carbonate, crab and/or shrimp shells (chitin & chitosan) are commonly given to cats experiencing kidney failure. Some common phosphate binders marketed for humans, but occasionally suggested for cats, are calcium acetate (PhosLo™) and sevelamer (Renagel®). Both can produce various digestive tract side effects – so begin gradually. Others are known to interfere with the absorption of fat soluble vitamins (A, D-3/calcitriol & E). Whichever product you use, be sure its use does not keep your pet from meeting its nutritional needs (no turning up its nose at its food).
A Potassium Supplement When Required
Potassium supplements (Tumil K®, etc.) can help if your cat’s blood potassium level drops too low. Your veterinarian might suspect low potassium (hypokalemia) when your cat does not eat adequately to maintain its former body weight and appears listless and weak. As I mentioned earlier, in very advanced kidney disease, your cat’s potassium levels can actually become too high. You need to let your veterinarian make those decisions.
Experimental Treatments
Erythropoetin To Combat Anemia
Synthetic Erythropoetin, (Epogen®, Betapoietin®, Eporel®) products encourage bone marrow to produce more red blood cells. However, because these hormone products were molecularly engineered to match human erythropoietin, cats eventually cease responding to them. But they often do raise your cat’s PCV for a time. There is a moderate concern when giving these products. When a cat’s immune system decides to attack human erythropoetin because it is a foreign protein, it not only destroys the human-engineered erythropoetin that was given – it can also destroy the cat’s natural erythropoetin. So, it is possible that it might make its anemia even worse. I would only suggest these products as a last ditch effort. Some believe that these potential side effects might be less when darbepoetin is used. (read here)
Varenzin®
In May of 2023, the FDA gave conditional approval for Elanco Pharmaceuticals to market, molidustat to combat the anemia associated with advanced kidney disease in cats. Previously, this compound had been used to treat anemia in humans suffering from kidney failure (read here), and by athletes to gain a competitive edge. (read here) Elanco’s trade name for molidustat is Varenzin®. Bayer markets or marketed the human product in various parts of the world as Musredo®, Larvol® and Larvol Delta®, others perhaps as Enaroy®. But I believe that in the USA, they are applying to the FDA for approval for a similar drug, daprodustat. Varenzin™ is an oral suspension. It gained conditional approval from the FDA in 2023. That means that it appears to be safe, and they will observe its effectiveness and safety before granting unconditional approval. In their FDA evidence submission, they gave their product to 14 cats ranging in age from 4 to 17 years old. All were anemic due to their kidney disease. Cats received Varenzin for 28 days. Fifty percent of the cat’s anemia declined by 25% or more, about a 4% increase, whereas only one out of the six control cats with anemia improved by 16.7% during the same time period. At the end of that time, 8 of these cat owners elected to continue giving their cats Varenzin® for an additional 8 weeks. On day 56, six of them were still showing benefit. By day 84, five of them were. The most common side effect was vomiting. A few also showed elevated blood pressure. Whether that was due to common anxiety to which cats handled by strangers are subject to (read here) or the influence of the drug is unknown. One cat was suspected of developing a stroke (a thromboembolism). If that had to do with the drug is unknown, but I recall seeing the same stroke warning on the human molidustat label. One cat with a prior history of seizures developed a seizure. Again, it is unknown if that had anything to do with Varenzin. For reasons unclear to me and not included in the FDA data I have access to, Elanco suggests that cats get a 7-day breather from the drug after each 28-day treatment cycle. You need to shake the bottle well before using it because it is a suspension. Elanco’s suggested dose is 2.3 mg/lb (5 mg/kg) body weight, or was at the time I wrote this. Product labels change, particularly on products new to the market. So read the instructions and dose suggestions on what you purchased. Please don’t rely on what you see on websites like mine. A measuring syringe comes in the box. Be sure to weigh your cat frequently to be sure the dose is correct. Your vet will determine your cats’ degree of anemia through and Hct or PCV before starting and monitor that weekly beginning about the 14th day of each 28-day cycle. It is quite dangerous if your cat produces more than a normal number of red blood. After that, it is wise to have your cat’s Hct/PCV checked every week, every two weeks or monthly depending on its degree of anemia. Whenever it becomes anemic again, Elanco currently suggests you begin a new Varenzin® treatment cycle – as long as 7 days have passed. If three weeks on this medication has not improved your cat’s anemia, Elanco suggests that your cat be checked for an iron deficiency, some other inflammatory disease or internal bleeding.
Fermentable Fiber
Fermentable or soluble fiber, when added to your cat’s diet, is thought to help remove toxins from its body. Because of this ability, it is often an ingredient in diets sold to manage kidney failure in cats. In those diets, the source is usually sugar beet pulp. Too much fermentable fiber in your cat’s diet might cause diarrhea and flatulence. That type of diarrhea is a mess – but not a hazard to your cat’s health.
Subcutaneous Fluid Administration
When encouraging your cat to drink more is no longer sufficient, sterile fluids needs to be given periodically by injection under your cat’s skin. Most cat owners, with their veterinarian’s guidance, are capable of learning to do that at home. The effect of those fluids is called diuresis. As body fluid content increases, the cat’s kidneys work harder to remove it in the form of urine and, in the process, flush out more toxins from your cat’s body. The effects can be dramatic – similar to a human visit to a dialysis center. This procedure causes the cat very little pain or discomfort if the fluid is administered at body temperature, slowly and in multiple locations. In most cases, there is no benefit in giving these fluids intravenously. However, cats with failing kidneys often do need emergency intravenous fluids when they are presented severely dehydrated to veterinarians. The hesitancy to inflict pain on a loved pet can be more than some cat owners can overcome. In those cases, find a mobile veterinarian who is willing to visit your home or a veterinarian willing to dispatch one of his/her technicians to your home periodically. Observe the procedure. With time, you will most likely overcome your hesitancy. In your search, independent veterinarians have more decision-making flexibility than those working for large conglomerates like VCA, Blue Pearl or Banfield. Corporations discouraged their employees from working off-script.
How Much Longer Will My Cat Live?
Pets with fasting blood creatinine levels below ~2 mg/dl usually do well for years. Pets with blood creatinine levels of up to ~4 mg/dl have also survived happily for many years – with appropriate treatment. But when your cat’s creatinine levels exceed ~5 mg/dl, it is severely azotemic and will probably survive only a mater of months. Those in the 6-8 mg/dl range can sometimes survive for short periods. But their quality of life is very poor. Although it is sometimes possible to keep those pets alive for a while with heroic measures (feeding tubes, etc.) — I question the kindness of doing so. Your cat loves you very much. But it is a two-way street – it is relying on you to end its life peacefully and humanely when the time comes. Your veterinarian is, at the most, likely to hint when that time comes. If he/she does, I would take it as your vet’s heart-felt advice. Hesitancy to suggest euthanasia among veterinarians comes with their experience that pet owners often expect more from us than is humanly possible. When your cat has lost its will to eat, and appetite stimulants like mirtazapine/Mirataz® and Elura® are no longer effective, offer it what was once its favorite lifetime treat. If it turns its head away at that or sniffs and licks at it halfheartedly, it is trying to tell you something that in your heart you already know. Cats live in the here and now, they do not fear death the way we humans do.
A Kidney Transplant For My Cat?
Kidney transplants are an option for cats – if you are fortunate enough to be able to afford the procedure, and if your cat is young enough and healthy enough for the results to likely be successful. Remember, it is not only kidney function that declines in the elderly. Kidney transplants are more successful in cats than in dogs, but not nearly as successful as in humans. Currently, a little more than half of the cats that have kidney transplants are thought to survive an additional six months. Veterinary centers that specialize in these procedures are likely to offer you a more rosy outlook than disinterested parties. The Center’s success rate is also much higher if they only accept candidate cats who are the most likely to benefit. As I mentioned, those are generally younger cats without multiple health issues. Of those centers that do this procedure, some cats have lived an additional three years. Success rates for transplant surgery generally go up as a specific surgeon and his/her assistants accumulate more experience with this very delicate procedure. None of the university-based centers are very transparent about providing usable success rate statistics.
Is Hemodialysis An Option?
Hemodialysis, as it is performed on humans with failing kidneys, is not frequently performed in cats. The Subcutaneous fluids I mentioned offer similar, but less effective benefits. A similar blood-cleansing effect for your cat in a uremic crisis situation can sometimes be obtained through peritoneal dialysis, in which fluids are injected, and then removed from your pet’s abdomen. That procedure is usually reserved for cats whose kidneys have shut down acutely (suddenly) due to exposure to toxic products or infection. Performing hemodialysis, as done in humans, is much harder for veterinarians to perform due to your cat’s smaller size. The procedure is too traumatic and risky for cats to be subjected to it frequently.
What About New Experimental Drugs, Homeopathic Remedies And Other Unproven Treatments I Hear And Read About On The Internet?
Despite the many things today’s marketers will tell you, nothing they offer is likely to benefit your cat. You might even see some of those products that the Googlebot chose to show at the bottom of this webpage.
We veterinarians are unlikely to be able to offer your cat more than we already do until substantial progress has been made in regenerative medicine. If you do take this road before that happens, my suggestion would be one of the experimental options in stem cell therapy. (read here) Various techniques in platelet rich plasma and harvested stem cell therapy. If you do, please let me know the results.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.