Leptospirosis In Your Dog
How Dogs Catch It, How Vets Treat It, How You Can Prevent It
Ron Hines DVM PhD
 Do All Dogs Need The Same Amount Of Leptospirosis Vaccine?
Do All Dogs Need The Same Amount Of Leptospirosis Vaccine?
 Feedback From Dog Owners About Leptospirosis Vaccinations
Feedback From Dog Owners About Leptospirosis Vaccinations
 The Most Likely Places For Your Dog To Be Exposed
The Most Likely Places For Your Dog To Be Exposed
What Causes Leptospirosis?
Leptospirosis is a disease found in temperate climates throughout the world. It is caused by a bacteria – a peculiar, very thin, corkscrew-shaped organism with a hooked “tail” (they really have no front or rear). This family of bacteria are called spirochaetes. The majority of spirochaetes live their lives free in the environment causing no one harm. But a few have evolved to cause particularly nasty diseases. Those undesirable ones include the eight varieties of leptospira that cause leptospirosis, as well as their cousins, the spirochaetes responsible for Lyme disease, relapsing fever and syphilis. (read here) None of them, other than syphilis, are particularly choosy about whom they infect.
Traditionally, the threat of leptospirosis was associated with heavy rainfall, high humidity, hot climate, flooding, a lack of basic sanitation and rats. (read here) Apparently-healthy rats can carry leptospirosis in their kidneys and spread it through their urine. Rats are still a threat, but dense populations of urban raccoons are an even greater threat today. (read here, here & here)
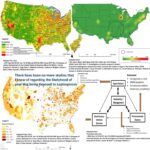
If you expand the map at the top of this page you will see where most cases occur in dogs in the United States. Late summer and fall see the most cases. The leptospirosis organism usually enters the body from contaminated water or soil through the pet’s mouth, nose, eyes or even broken skin. Hawaii at one time led the Nation in reported cases. It is also the state with the highest average rainfall. The CDC reports that ~50% of the leptospirosis cases in people now occur in Puerto Rico, with Hawaii and Florida next in line.
You Mentioned Varieties. Is There More Than One Type Of Leptospirosis Organism?
Yes.
There are many strains. They are called serotypes or serovars. Serovars differ in the structure of certain of their surface compounds (lipopolysaccharides). Since these compounds are the ones that your dog’s immune system must recognize and respond to by producing “exact fit” antibodies, immunity to one serovar may not provide strong immunity to other serovars. There have been over 300 different leptospirosis serovars reported. (read here) The ones that most commonly infect dogs are Leptospira interrogans icterohaemorrhagiae, L. canicola and L. kirschneri/grippotyphosa. Other serovars are occasionally responsible for infections in dogs. The prevalence of all of them as well as their accepted names vary from place to place and time to time.
Both Zoetis’ Vanguard® L4 and Boehringer Ingelheim’s Recombitek® 4, leptospirosis-containing vaccines contain killed portions of the L. canicola, L. grippotyphosa, L. icterohaemorrhagiae and L. pomona organisms. Those are the serovars that they feel your dog is most likely to be exposed to. But if your dog becomes infected, our current diagnostic test, the MAT test, has limited ability to accurately determine which of the leptospira serovar(s) is causing your dog’s infection. ELISA tests can also be used. But test results can be confusing and hard to interpret. (read here)
How long After Exposure Might My Dog Become ill?
Most of the infected wild animals, dogs and domestic livestock that spread leptospirosis don’t appear ill. They are carrier animals in which the leptospira have taken up residence in locations that are sheltered from the animal’s immune system. Usually, the kidneys. Residing there for long periods, they are intermittently present in the animal’s urine. Once infected, dogs take about 2 weeks before the leptospira organisms begin to appear in their urine. Most often, dogs only shed those leptospira for a few days. But in some cases they have persisted in their urine for more than two years. (read here) I suppose that no one could be certain that the dogs in question with long-time persistent shedding were not just reinfected with a different serovar. Veterinarians do not know what percentage of dogs that are infected with leptospira actually become ill. The CDC still believes that in exposed people, most leptospirosis infections are asymptomatic.
The incubation period for leptospirosis (the time from exposure to illness) can be only a few days or as long as two weeks. In experimental studies, the average time was about a week. (read here) But as I previously mentioned, many dogs that become infected or exposed never become visibly ill. (read here & here)
Today most dogs in the prosperous parts of the world catch leptospirosis from exposure to wildlife reservoirs, not from other infected dogs. The species of animals most responsible for spreading the disease vary from place to place, time to time and even season of the year. In areas of poverty where rats are prevalent, rodents are thought to be the prime transmitter. In prosperous areas where urban wildlife like raccoons are abundant, suspicion falls on them. (read here & here) It is not that the cute and endearing raccoons are any better carriers of leptospirosis than a number of other critters. It is just that they are the most clever and fearless about invading human and dog-occupied space in their search for food. People obligingly feed them – sometimes inadvertently, sometimes intentionally. 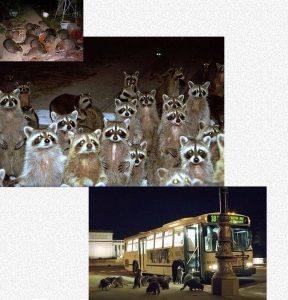
Nothing interested your dog more than sniffing the scent of exotic urine. By the time your dog sniffs a urine-contaminated location, the raccoon or other leptospirosis vector is long gone (has departed), but the leptospira can survive in water and soil for weeks to months. (read here) Leaving food out for stray cats presents the same underappreciated threat. (read here, here & here) The second way leptospirosis travels is when animal urine is washed by rainfall into bogs, streams and impoundments that your dog frequents. Drainage pipes and culverts are a choice location for raccoon latrines.
Dogs and cats that spend their days indoors or hiking with you in areas remote from standing water and vermin-attracting garbage are considerably less likely to encounter leptospirosis than those that spend time off-leash where the organisms thrive.
What Are Some Signs I Might See If My Dog Became ill With Leptospirosis?
I mentioned earlier that many dogs show very few or no signs of illness when infected with leptospirosis and succeed in ridding their bodies of these organisms on their own. There is really no advantage for a disease organism to kill its host or make it seriously ill. But there is really no way of knowing which dog will react violently to a leptospira infection and which one will not. Perhaps it is the damaging ability (virulence) of the particular leptospirosis serovar that your dog was exposed to. Perhaps the genetic abilities of your dog’s immune system factors in. Perhaps the size of the dose of leptospira organisms it encountered is another factor. Perhaps all three. Veterinarians really do not know.
It is the fever, muscle pain, depressed mood and lack of appetite associated with leptospirosis that motivate dog owners to bring their pet to their veterinarian. In those cases, vomiting and diarrhea ares also common. Your pet’s midsection (abdomen) might be tender to the touch. As the disease progresses, some of these dogs show a yellowish hue to their gums and the whites of their eyes – evidence of jaundice. Your dog’s liver is a common target of leptospira. Some of the dogs whose livers are affected are left with chronic hepatic problems. (read here) Elevated blood liver tests confirm liver involvement. But on rarer occasion, the jaundice is the result of a slowdown in your dog’s blood clotting process or destruction of its red blood cells by the leptospira toxins. (read here) Occasionally lungs are a primary target of leptospira. That can be due to blood clots and to the bleeding tendency I just mentioned. Those dog have shortness of breath (dyspnea). They might cough up blood or have nose bleeds. An increased tendency to bruising or the presence of blood in their stools or urine is also possible. (read here) Leptospira move freely through the bloodstream. When a dog’s kidneys are a prime site of damage, their kidneys sometimes fail. (read here)
What Diagnostic Tests Will My Veterinarian Use?
Like many infectious diseases, your veterinarian encounters, initial blood work tests rarely indicate a specific disease organism. Your dog’s total white blood cell count (WBC) will often be elevated, particularly its neutrophil count. It is common for your dog’s thrombocyte count, (the cells involved in blood clotting) to be low as well. Because of the bleeding often associated with leptospirosis, your dog might also be anemic. Since your pet’s kidneys are often a destination for leptospira, tests might detect decreased kidney function (i.e. elevated BUN and creatinine). Liver tests (ALT, GGT & bilirubin) are commonly elevated as well. Alkaline phosphatase (AP), an enzyme released by many injured tissues, is often also elevated. Your pet’s urine analysis (urinalysis) often confirms a kidney infection as well (e.g. pus cells, casts and protein).
The symptoms that I mentioned earlier, along with a history of your dog being exposed to places where leptospirosis lurks, and these blood results might lead your veterinarian to suspect that your dog had contracted leptospirosis. If that is the case, your vet might order one or more of the three specific leptospirosis tests I mentioned earlier: the MAP test, a PCR test, or a leptospirosis IgM ELISA test. All of these tests have their limitations – but they are the best we veterinarians currently have to offer. (read here)
Idexx Laboratories (SNAP® Lepto) and Zoetis (WITNESS® Lepto), do market in-office leptospirosis tests that veterinarians can perform on the spot (point-of-care tests). Both tests rely on detecting an early antibody type (IgM) that a dog’s immune system produces on its first encounter with the leptospirosis organism. Later on, and in vaccinated dogs, the antibodies present are mostly IgG). The development of these tests has been a great help in getting leptospirosis-infected pets into therapy quickly – before the results from central laboratory MAT and PCR tests have had time to arrive.
Is There A Danger I Can Catch Leptospirosis From My Dog?
It is theoretically possible – but quite unlikely. Using common sense, sanitation products and practicing good hygiene is usually all that is required. (read here) Here are some things that minimize the transfer of infectious diseases of all kinds: Have only one healthy, family member care for the ill dog. It should not be a child or a person with a weakened immune system. Confine your pet to an easily sanitized area of your home. Prevent exposure of your other pets. Wear protective gloves when cleaning up after your dog. Take your dog out on a leash frequently to urinate and defecate on a hard surface. One such as concrete or tile that can be easily sanitized with bleach. When you are potentially exposed to any secretions or waste from your pet, disinfect your hands well with a common disinfectant. I use 70% isopropyl alcohol. On nonporous surfaces bleach and Lysol as well as povone iodine kill leptospira rapidly. So does heat, sunshine and drying. Should you feel ill, always inform your physician about your pet’s illness. If you are a worrier and want to be more certain your dog does not remain a leptospirosis carrier, have a leptospirosis PCR test or two performed on its urine several weeks after it recovers.
How Will My Veterinarian Treat Leptospirosis?
Every veterinarian who diagnoses or is suspicious of a case of leptospirosis will place that dog on antibiotics. Not all commonly dispensed antibiotics are equally effective in destroying the leptospira organisms. The best ones are penicillin derivatives (ampicillin, amoxicillin, etc.), a cephalosporin, or doxycycline. When vomiting and/or diarrhea are symptoms, oral doxycycline might not be the best choice. When nausea, or stomach and intestinal inflammation are present, the antibiotics are best given by injection, not orally. No studies I know of have reported that antibiotics are effective in preventing the development of carrier dogs; but I would probably keep the patient on antibiotics for a considerable period after recovery.
Very sick dogs require intense supportive care to get them through the early stages of leptospirosis. Dogs that vomit or show intestinal involvement generally receive medications to calm their stomachs (e.g. metoclopramide, maropitant/Cerenia®) and medications to decrease stomach acidity (e.g. ranitidine/Zantac® or omeprazole/Prilosec®). Diarrhea needs attending to as well because it causes so much fluid loss. So many canines also need liberal amounts of intravenous fluids. If their abdomen is sensitive, or they show other evidence of pain, dogs might benefit from the judicious use of pain-control medications such as buprenorphine. Those with respiratory distress benefit from oxygen and some from theophylline. Dogs that are not willing to eat need to receive their essential nutrients in other ways.
How Can I Prevent My Dog From Catching Leptospirosis?
Some diseases come to you. But in the case of leptospirosis, you go to it. So limit your dog’s exposure to standing water, the urine of infected wildlife, rats, stray cats and roaming dogs. In those areas, your dog needs to be on a leash and under your close supervision. The prime attractor of leptospirosis carriers is easily available food. That could be food intentionally placed there for them by well-meaning people, food left outside your house for your pets or food-related garbage carelessly discarded. Without those food sources, there would not be an urban reservoir of leptospirosis and other similar diseases. When we intentionally or unintendedly upset the balance of Nature, we do not do animals of any kind a long-term service.
Leptospira organisms generally enter your dog’s body through its mouth or nose. Some have associated leptospirosis exposure with feeding raw meat. That is highly unlikely to happen when it is meat sold for human consumption. At least not in the developed world. (read here) Leptospira are very dependent on water, mud or damp clay soils to survive. That is because they do not possess a waterproof membrane, cysts or spores to protect them from drying. They quickly die on dry surfaces – even if those surfaces were contaminated with the urine of an infected animal. Temperatures at or above 131 F (42 C) kill leptospira almost immediately. All common household disinfectants (bleach, alcohol-based products, vinegar, lemon juice etc.) kill leptospira. Porous items need to be completely submersed in those solutions. Standing water can be disinfected using swimming pool chlorine tablets. However, those products are toxic to all aquatic life. Common sewage treatment processes are so effective against leptospira that smelly polluted effluent water is not nearly as much of a leptospirosis threat to your dog as are destination park ponds and slow-moving streams where water appears pristine. (read here) Tropical and semi-tropical humid climates with high rainfall favor leptospira survival. The United States Army once experimented with giving their soldiers in Panama doxycycline in an attempt to prevent them from contracting leptospirosis. (read here)
Should I Vaccinate My Dog Against Leptospirosis?
The American Animal Hospital Association (AAHA) considers leptospirosis vaccine a “non-core” vaccine for dogs. That is, they do not recommend that dogs receive the vaccine unless there is a good chance they will be exposed to leptospirosis. The primary reason for that is that veterinarians see more vaccination reactions following the administration of vaccines that contain leptospirosis ingredients than any other vaccine that they administer. These reactions range from the minor inconvenience of post-injection pain at the injection site, to facial swelling and hives, to fatal anaphylactic reactions. Which dog will experience any of them cannot be predicted. I believe that the “one-size-dose-fits-all” philosophy of vaccine manufacturers, the FDA and the AVMA community account for most of the leptospirosis reactions that veterinarians see. Read about that here.
Only you can decide if your pet’s risk of catching leptospirosis justifies the risks of yearly leptospirosis antigen-containing vaccines. In making that decision you need to ask yourself if your dog frequents areas that are likely to harbor lepto. Ask your public health department how many confirmed cases of leptospirosis occurred in your community in the last few years. You should also consider your dog’s size in relation to the dose size and if your dog or its siblings, or its parents experienced vaccination reactions to any vaccine in the past.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.


