Why Is My Dog Or Cat Itching & Scratching? — Allergies In Your Pet
Ron Hines DVM PhD
 Some other causes to consider:
Some other causes to consider:

Next To Fleas, Allergies Are The Most Common Cause Of Itching and Scratching In Your Dog Or Cat
Also common, are two forms of mange, sarcoptic and demodectic which can also be responsible for hair loss and scratching. Fleas are dealt with in another article in this series, you can read here. Sarcoptic and demodectic mange are covered through their links.
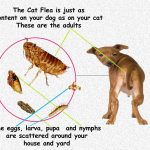
I included a diagram of the flea life cycle here because over half the cases of allergic skin diseases have fleas – seen or unseen – as the underlying cause. Once you are certain that no fleas or mites are present, it is likely that allergies are the cause of your pet’s scratching. In human beings, allergies are often expressed through the respiratory system. If you yourself have allergies, you are likely to have a stuffy nose, sneezing and watery eyes. This is because the histamines that humans produce are released primarily in the membranes of the respiratory system and eyes. In dogs, histamines are released primarily in the skin. Veterinarians have found that dogs with a tendency to canine atopy tend to have lower than normal levels of IgA. That is a genetic problem that some dogs are born with. In some breeds at least, the location of the defective gene responsible for that has been located. (read here & here)
How Do These Allergies Occur?
All chronic allergies are based on the body recognizing protein substances as foreign and trying to rid itself of them. Mold, dander, bacteria, pollen, flea saliva along with a host of other substances are allergens made up of proteins foreign to the body.
Veterinarians will discuss pollen allergies, for an example because they are so common. In this case, pollen is called an allergen – something the body recognizes as foreign. When a pet’s immune system is exposed to pollen for the first time, some pollen attaches to the linings of the nose and lungs. The body’s immune system recognizes that pollen is not supposed to be there and, in response, produces antibodies against the pollen called immunoglobulins of the E class (IgE) and G class (allergen-specific IgE). This process is called sensitization. The IgE attaches to cells in the body called mast cells. These cells then leak (degranulate) and release inflammatory substances (histamines, bradykinins, and proteolytic enzymes) which cause the symptoms of allergy in your pet. In people, large numbers of mast cells are located in the respiratory system. That is why our allergies usually have respiratory system symptoms. In dogs and cats, more mast cells are more prevalent in the skin. That is why dog and cat allergies usually cause signs associated with the skin and ears, such as itching, hives and inflammation. This allergic disease is called atopy or atopic skin disease. Only about 15% of pollen allergies in dogs and cats cause respiratory system signs, such as nasal stuffiness and sneezing.
Canine Inhalant Atopy
This is the type of allergy for which we used pollen as an example. It is the most common form of allergy in dogs and cats, making up over ninety percent of the cases I see. About nine percent of the canine population has this disease. Certain breeds are more susceptible to than others. Among the most susceptible are bulldogs, Labrador retrievers, miniature schnauzers, poodles, west highland white terriers and German shepherds and their crosses. Pretty much in that order. But dogs and cats of any breed share allergic problems as well. Dogs usually show their first signs of itching between 10 months and 4 years. If a dog does not have this condition by the time it is four years of age, it is unlikely that it will ever have atopic skin disease. The disease often begins as a seasonal problem, but after a number of years (or moving to a southern climate) the itching occurs year round. Some common allergens are flea saliva, tree, grass and shrub pollens, house dust, mold, dust mites, and feathers. In 2023, allergic skin disease treatments are the #1 most common claim submitted to the Nationwide Pet Insurance company. That is followed by ear infections (which are commonly are due to allergic dermatitis), diarrhea and vomiting in that order. In cats, allergic skin disease is not in the top four claims group. When it comes to ear infections, the most common cause in dogs, after floppy ears, is an underlying flea allergy.
Flea saliva allergy is a special form of Atopy. Fleas survive by sucking blood from your pets. To get this blood, they drill their mouth parts into the dog or cat’s skin and inject special anticoagulant saliva into the site to keep blood flowing while they engorge. This saliva is highly irritating to some dogs and cats. These pets do not only itch at the site of the flea bites, they itch all over. The pads of their feet are often itchy, puffy and inflamed. Areas between the toe pads as well as the ears often become infected with bacteria due to the pet’s constant licking and chewing. Because of the availability of excellent flea-control products such as Advantage and Frontline, many vets see less flea allergy than they once did. Recent studies indicate that fleas do not have to bite the dog to initiate itching – their presence is enough.
Food Allergies:
Food allergy cases are less than fifteen percent as common as canine atopy but occur with about the same frequency as atopy in cats. The itching food allergies produce is constant throughout the year. Cocker Spaniels, West Highland White Terriers and Labrador Retrievers are particularly susceptible to food allergies. However, the majority of these breeds that have itching problems do not have food allergies. Dogs and cats can be any age older than a few months when signs first begin. Some common food allergies in dogs are to beef and pork, fish, dairy, eggs, corn, soy, wheat, and preservatives and dyes in food and treats. But almost any diet ingredient can be involved. The most common allergens in cats are to fish, beef and chicken. Many believe that when dogs (or cats) become allergic to food ingredients, it is not because their immune system is defective. It is because large, potentially allergenic proteins are not being disassembled in the pet’s intestines into smaller, much less antigenic amino acids before they enter the body’s circulation. That is called leaky gut syndrome. (read here) Wikipedia is quite dismissive that leaky gut syndrome actually exits. But there are just too many Pubmed entries regarding it for it to be entirely imaginary.
What Signs Would I See In My Dog Or Cat?
Canine Atopy and food allergies are not visually distinguishable because the signs of both diseases are the same. The most common sign of the conditions is constant itching, scratching and licking. Dogs will often rub on objects. The degree of discomfort the pet undergoes is partly dependent on its temperament. High-strung breeds and very active pets do severe damage to their skin. The face, lumbar area at the base of the tail (particularly if fleas are the cause) ears and paws show the most damage. In severe cases, the skin of the whole body is inflamed and covered in crusts, while the hair coat is thin and broken. In mild cases, the pets only lick these areas, discoloring light hair coats with salivary stain. When fleas are the problem, small pepper-like granules are present over the neck or in the dorsolumbar (“lower back”) area. These specks of digested blood or flea dirt will “bleed” a rust-colored trail if moved to white tissue paper and whetted with water.
As your dog or cat scratches, it destroys the outer waxy layer of the skin. This allows bacteria and mold to enter the skin and causes a musty, oily skin condition called seborrhea. Because the ears are covered with skin, ear canal redness, odor, and inflammation are common in canine atopy. Sometimes ear problems are the only sign present. When this is the case, we treat the ears with specific antibiotic, antifungal, corticosteroid preparations but must treat the whole dog with medications as well. Veterinarians rarely attempt to identify which bacteria are present in your pet’s ears or which antibiotics these bacteria are sensitive to, unless standard treatments fail. A problem with antibiotic sensitivity tests is that bacteria or yeast that have developed resistance to specific antibiotics when given at their usual safe doses orally or by injection, may still work fine in clearing up your pet’s ear infections because the antibiotic’s concentration, when applied in the ear is many times greater that it would be if given orally or by injection.
Cats develop a condition called miliary dermatitis, in which the surface of the back and scruff of the neck are covered with bumps and scabs. Allergic cats sometimes develop another condition called eosinophilic granuloma complex in which ulcers form on the lips, tongue, and surface of the body. After months and years of scratching, the skin of the inner thighs and flank often becomes thickened and blackish. This condition is called acanthosis nigricans.
Damaged skin due to the pet’s scratching often leads to superficial staphylococcus bacterial infections (pyoderma) and infection with the yeast, Malassezia. Mild bacterial conjunctivitis or eye infections with greenish matter at the inner corner of the eye are common. It is important to realize that although a bacterial or fungus condition is present and may need treatment, the root of the problem is allergic dermatitis. In very severe cases of skin allergy, the superficial lymph nodes of the body enlarge due to secondary skin infections.
How Will My Veterinarian Diagnose This Problem?
The clinical diagnosis of allergic dermatitis is one of exclusion of other causes of skin disease. Veterinarians usually do skin scrapings when pets with this condition are presented to them for the first time or when they do not respond to treatment as expected. Through skin scrapings, they attempt to rule out sarcoptic mange as a cause of the pet’s problems and locate secondary bacteria and fungi that may be making the skin problem worse. If one cannot rule out mange, if the dog’s history suggests it might be mange, or other members of the household are itching, veterinarians may put the pet on a test dose of a safe anti-mange medicine called ivermectin. (certain breeds cannot tolerate ivermectin) They also try to rule out fleas as the source of the problem. Some dogs and cats are so good at grooming that no fleas remain on them when they are examined. Even when I cannot locate fleas on a pet, I can often locate flea dirt. In some of these pets, the presence of tapeworms is the only indication of fleas or one may find fleas on another household pet, which does not have skin problems.
There are other signs that the problem may be allergic. Typically, atopy occurs in dogs and cats between one and three years of age. This makes the diagnosis of allergies in puppies and older dogs less likely. The first two or three years that the condition exists, it is often seasonal, occurring only in the spring and summer months. Flea-related allergies tend to subside after the first few freezes of the winter. Golden retrievers and arctic breeds with thick oily hair are susceptible to a special form of dermatitis called hot spots or acute pyotraumatic dermatitis (pyo=pus & infection due to scratching) dermatitis. In these cases, the dogs suddenly become extremely itchy over a small area. They are so troubled that they pull out the fur of this area and infect it through chewing in a matter of hours. The itching sensation departs rapidly thereafter – with or without treatment. It is not known if they represent a true form of allergy. Another form of the disease is called acral lick dermatitis. In these cases, a small area of skin itches over an extended period. Licking leads to a well-defined small area of raw skin, scarring and bacterial infection.
I try to learn if the parents of the dog or cat or its brothers and sisters also have itchy skin disease. Canine atopy, as well as food allergies often, often run in families.
In diagnosing food allergies, vets look for uniform involvement of the skin over the entire body. I rarely find that diarrhea accompanies food allergies. Often, the best way to rule out food allergies is to put the pet on a 60-90 day trial eating a hypoallergenic diet exclusively. Many hypoallergenic diets are available. Until recently, these diets relied on novel protein sources such as lamb, venison duck or fish. The problem is that with time, allergy-prone pets eventually become allergic to these diets too. Hypoallergenic diets are available that use heat and hydrolysis to break their food proteins into a size theoretically too small to cause allergies (less than 10,000 Daltons). (read here) The biggest problem with these diets is that some pets won’t eat them. When food allergies are truly present, the most common culprits are beef, dairy, chicken, wheat, egg, soy, lamb and pork, in that order. If you begin your pet on a low-antigen diet, either one containing ingredients your pet has never eaten before (such as alligator) or a hypoallergenic one that has been heated enough to break up its large, antigenic protein molecules, give it 4–6 weeks to see a modest reduction in itching. But it might take double that time to see maximum improvement. Since novel meat diets are produced in the same company facility and on the same machines used to produce ordinary pet food. (read here) Studies have found that many of these diets contain residual amounts of protein from animal species not mentioned on their labels. So, you might find that hydrolyzed, diets (e.g., Hill’s z/d, Purina HA, Royal Canin Hydrolyzed, etc.) the best initial option. Those diets don’t have to be forever. If one of these brands causes improvement, you can then add dietary ingredients one by one to find what specific proteins your pet is sensitive too. Vets call that an elimination test – although it is, in fact, an addition test. As I mention in many of my articles, blood or hair-based allergy testing is close to worthless. At a veterinary symposium last week, a well-known veterinary dermatologist mentioned that these tests are about 58% accurate – just a bit more accurate than a head’s toss with a penny. He mentioned that another dermatologist submitted a hair sample from a stuffed teddy bear. They reported back that the teddy bear was allergic to beef. Another point he brought up was that dog and cat flavor tabs are often flavored with beef. So, if itching increases just after your pet’s monthly heartworm or flea/tick flavor tab, you might consider changing to a topical product that accomplished the same protection.
Veterinarians will usually examine pets with skin disease in a darkened room with an ultraviolet lamp. Hairs that glow are diagnostic for ringworm. Ringworm is almost never itchy, and glowing hairs are not found in cases of allergic skin disease.
Veterinarians often encounter Malassezia yeast in skin scrapings of dogs with itchy skin. This fungus is a normal inhabitant of the skin of dogs. It only becomes a problem when the pet has an underlying problem, such as allergic skin disease. Some of the antifungal shampoos I mention elsewhere in this article are quite helpful in controlling it.
Are There Any Other Health Issues That Might Be Confused With Canine Skin Allergies?
One does concern me. Veterinarians now know that not all dogs exposed to sarcoptic mange mites develop the typical hair loss symptoms of mange. An unknown number of dogs continue to harbor a few mites in their skin for long periods. How individual dogs respond to exposure to sarcoptic mange mites depends on their individual genetics. (ask me for DeCandia2020.pdf) Some of those dogs might itch and some might not. Idexx Laboratories offers a Sarcoptes Antibody ELISA test to help identify those dogs with low sarcoptic mange mite numbers. Alternatively, you could administer a monthly isoxazoline drug such as Simparica® for a few months. Simparica® (sarolaner) has been verified to rid dogs of sarcoptic mange mite infections. (read here)
Allergy Testing
Rast Testing (a laboratory test, performed on your pet’s blood)
I am not a fan of this test, it gives too many false positive and occasionally false negative results. But many veterinarians suggest it. There are Two forms of allergy testing available, this one and the skin test procedure that follows. Only veterinary dermatologists are qualified to interpret the results of the more complicated, more time-consuming, more accurate and more expensive intradermal skin tests. The easiest and most commonly performed test in animal hospitals is called the RAST test. This test, which is performed on a blood sample from your pet, stands for radioallergosorbent test. In the test, the presence of IgE antibodies to specific antigens is determined by a central laboratory. Pets must not have had corticosteroids or antihistamines administered for thirty days prior to testing. As I mentioned, the problem with this test is its high number of false positives. If the test determines that a pet is not allergic to an antigen – that is probably correct. But positive reactions often turn out to be wrong. If the RAST test is used, a central laboratory will prepare an antigen extract, which can be injected into your pet’s skin periodically to hopefully decrease the effects of allergies. Oral antigen extracts serve the same purpose. As I mentioned, most research indicates that the blood-based test is extremely inaccurate in pets and humans. (read here) I suggest intradermal skin tests if at all possible – although those, too, produce a substantial number of errors. To read more about the benefits and limitations of both these tests, go here.
Skin Testing
A more reliable test is an intradermal skin test. Before the test is administered, the pet is taken off all corticosteroid, tranquilizing or antihistamine medications for 30–60 days. In this test, small amounts of various allergens are injected into the skin. The entire side of the pet must be shaven to perform this test. Then the injection sites are monitored over an hour’s period to judge the degree of redness and swelling at each site. A list of offending antigens is used to prepare an allergen extract, which is injected periodically into the pet. With time and success, these injections lessen the pet’s allergies to these allergens. Because a high degree of skill is necessary in giving and interpreting the results of this test, veterinary dermatologists usually perform it. (Even when skillfully performed, this test can also give false results. The most common findings in positive skin testing is an allergy to flea saliva. Probably the next most common allergy is to dust mites. Studies have consistently found that dust mites and storage mites (the mites that inhabit grain-based products such as dog and cat kibble) are very similar and probably cross-react in mite-sensitive pets. The only solution I know of is to store your kibble in the freezer.
The Strange And Unusual
A perplexing cause of itching in dogs is the development of autoantibodies (aka autoallergies). These are pets, primarily dogs, that show no allergies to any of the common antigens veterinary dermatologists test them for. They have no flea exposure, their tests for mange and skin fungi are all negative, but they still stop itching when they are given a corticosteroid orally, topically, or by injection. Many of these dogs are believed to have become allergic to one or more of their own body proteins. One could also describe this as a form of autoimmune disease. In other cases, it may take a combination of these antibodies and certain foods to trigger a more severe itching episode. (read here) The culprit most discussed is the tomato. So, for some dogs and cats, it might be unwise to give them your leftover pizza, spaghetti, etc., no matter how much they would undoubtedly enjoy it. (read here)
Skin Biopsies
Occasionally, when veterinarians are uncertain if the problem is a routine case of allergy, they will take a biopsy specimen of the skin involved and send it to a pathologist for evaluation and diagnosis. This can rule out the presence of other disease, such as lupus (autoimmune disease). Blood tests might also detect elevated levels of eosinophils, which occasionally also occurs in allergic skin disease. Biopsies can also identify the rare cases of calcinosis cutis.
What Treatment Options Are Available For Allergic Skin Disease?
It is next to impossible to avoid all the environmental allergens that plague allergy-prone dogs and cats. The exceptions are pets that are chiefly bothered by fleas. So enforce strict flea control – even if you are uncertain that fleas are present. So many dogs and cats are cured by this simple task alone.
Approximately one in twenty of my clients elected to undergo skin testing and desensitization of their pets. This figure differs from practice to practice. The desensitization procedure can take a bit over a year to show good results. Dermatologists argue for the procedure pointing out, correctly so, that even if desensitization does not cure the pets, it may lower the dose of corticosteroids they require later in the disease. Skin testing also identifies the allergens and perhaps some of them can be avoided or eliminated from your pet’s environment. The procedure is quite costly, and requires a life-long commitment to frequent injections. (Most owners learn to give these injections themselves.)
Apoquel®
Zoetis introduced Apoquel® (oclacitinib) as an oral treatment for allergic dermatitis in dogs in 2014. At the time, it was the first new treatment option for canine skin allergies to appear since Novartis’ introduction of Neoral®/Atopica (cyclosporin) in 1996. Unfortunately, long-term use of Apoquel® has been associated with a higher than desired frequency of side effects. Read all about Apoquel® here
Cytopoint®
The FDA approved another Zoetis product, Cytopoint® (lokivetmab), for use in dogs in 2016. The EMA approved the drug one year later. Cytopoint® has revolutionized the treatment of canine allergies. The Cytopoint molecule is engineered specifically for use in dogs. It is ineffective in cats. Read all about Cytopoint® here.
Medicated Shampoos
Medicated shampoos are quite soothing to inflamed skin and lessen itching. Some veterinarians begin by dispensing clear tar preparations, such as lye tar shampoos. When these are inadequate, they may dispense selenium sulfide or benzyl peroxide shampoos. Benzyl peroxide is quite effective in eliminating secondary bacterial infections when they are part of the problem. Some pets are helped by oatmeal and antihistamine shampoos. With all these products, I usually suggest that the skin be first be cleansed with soapless soaps and then the medicated product massaged in and allowed a long contact period with the skin – the longer, the better. Weekly shampooing along with flea control is often sufficient for a number of years or forever – even when the pet has a confirmed allergy. There are pets that cannot tolerate weekly bathing as it dries out their skin too much. Use of a skin conditioning rinse often helps in those cases. Use temperate, not hot water, when you bath your pets. Medicated shampoos containing miconazole, ketoconazole, and/or selenium sulfide (e.g., Selson Blue™) are effective against yeast overgrowth – a common situation in allergic dogs. Follow directions. Pets will ingest more of these products while grooming themselves than us humans are likely to.
Antihistamines And Tranquilizers
Antihistamines help block the release of histamines from your pet’s mast cells. Antihistamines can be quite helpful for some itchy pets but appear to have no effect on others. Cyproheptadine, chlorpheniramine, and diphenhydramine (Benadryl®) are effective in lessening symptoms in some dogs and cats. But my opinion is that no antihistamines are as effective in doing so as they are in humans. All of these over-the-counter products can cause serious illness when given in too large a dose. Some antihistamines have a calming effect on dogs. That can be very helpful because dermatitis and itch are self-perpetuating. One that some owners find helpful for their pets is clemastine.
Some cat owners discontinue antihistamine use because they did not like personality changes they saw in their cats while on these medications. Some antihistamines can be applied in shampoo form. Some dogs damage their skin less when given mild tranquilizers such as acepromazine. If that medication actually lessens the itch or just sedated the dog is unknown.
Corticosteroids
Medicines of the cortisone class are effective and dramatic in controlling the symptoms of allergic skin disease in your pet. The problem is that this group of drugs has substantial and serious side effects when given in high doses over extended periods of time. Your veterinarian’s challenge is to treat your pets as long as they can without the use of these steroids. To do so, they use medications that are effective – but less dramatically so. I know you want dramatic, fast relief for your itching pet – but that may not be in its long – term best interest. Given only during flare-ups in an appropriate dose schedule, they are much less likely to cause serious side effects.
Many pet owners are worried when veterinarians suggest that their pets receive measured doses of corticosteroids to treat stubborn allergy cases. They should not be. These drugs have nearly miraculous powers in both human and animal medicine. They just should not be overused. Some of the drugs of the cortisone class are prednisolone, prednisone, triamcinolone, dexamethasone, beclometasone, and betamethasone. Corticosteroid sprays (containing betamethasone or triamcinolone, some with added antibiotic) are less absorbed into the body and therefore safer. When I dispense corticosteroids in their oral forms, I try to use so low a dose and as infrequent administration as possible (skip days) that a bit of itching persists in your pet – but at a tolerable level. A comfortable muzzle at night and when you are away is often the only additional thing that is needed. I give the lowest possible dose only two or three times a week. At a low dose, noticeable side effects tend to be minimal. Combining topical medications, antihistamines, cortisones and occasionally desensitization, allow us to keep the cortisone dose as low as possible for as long as possible. The most common side effect is increased appetite and consequent weight gain. There are ways you can avoid that. Read about that here. Being the owner of a 14-year-old allergic Labrador retriever, I know that the use of these drugs has greatly improved the quality of many pets’ lives. Just don’t overuse them.
Don’t allow your vet to administer the injectable, long-acting forms (melthylprednisolone acetate = “Depo” = “the itch shot” = ‘itch jab” etc.). Politely ask your vet if he/she would dispense an oral corticosteroid instead (and give it only intermittently during flare-ups and at as low a dose as possible).
You might notice that your pet drinks more and urinates more on corticosteroid medications. If they are over-used, a disease called Cushing’s Disease (hyperadrenocorticism) can be the result. The form caused by steroid administration (the iatrogenic or human-caused form) usually slowly subsides when the medication is discontinued.
As I mentioned, when you have decided that corticosteroids must be used, the safest way is to apply them is topically in sprays or lotions. Corticosteroids, applied to the skin, usually cause less side effects than those given orally or by injection. (read here) But in every case, your dog, or cat needs to be monitored closely for sensitivity to the product, increased thirst and urination or weight gain because traumatized skin can allow a considerable amount of topically applied steroid to enter the blood stream. (read here) Do your best to prevent the pet from licking the products off by massaging them well into the skin. The previous two links explain those side effects in detail.
Atopica® (Cyclosporin)
Another drug, Atopica® (cyclosporin) that I mentioned in passing earlier will also halt your dog or cat’s itching. But it does so with the potential of major health risks. Read all about Atopica® here. It is up to you to decide if the potential benefits of giving this drug to your dog or cat outweigh the discomfort and debility of chronic itching.
Antibiotics
Many pets that are presented to veterinarians with severe bacterial skin infections subsequent to the self-trauma (scratching) of allergies, need a two-week course of antibiotics to clear up the infection. If yeast overgrowth is an important component of your pet’s problem, fungus-specific medications such as ketoconazole, chlorhexidine or itraconazole might be indicated as well. (read here)
Food Supplements
There are a large number of “nutraceutical” products marketed for allergic skin disease. None of them have been adequately tested for effectiveness. The best that can be said for these products is that they probably do no harm. When I recommend them, I usually suggest ones that combine omega-3 and omega-6 fatty acids. Some of these products also contain zinc. Some pet owners do report them as being beneficial.
Distractions
No matter what the underlying cause of itching is in your pet, boredom, inactivity and unoccupied time will make it worse. It is not unusual for the underlying cause of itching to be eliminated by your veterinarian, only to have the pet continue to scratch and lick itself from force of habit. To minimize this, give your pets plenty of distractions. Hidden food morsels (my favorites are well-stuffed Kong toys), other interactive toys and chew toys, walks, play time, other pets, and view through a porch, kennel, or window all take your pet’s mind off of its skin. Try these distractions, and any others you might think of, before you resort to tranquilizers, powerful drugs and/or mood-altering medications.
Omega Fatty Acid Supplements And Ceramide-Containing Topical Products
Oral fatty acid supplements have been marketed for itchy dogs for many years. They usually contain a mixture of omega-6 and omega-3 fatty acids – compounds your dog’s body cannot synthesize on its own. These lipid supplements are occasionally helpful in decreasing itching when a dog’s diet does not provide them. Increasing the fat (lipid) content of the pet’s diet is occasionally helpful as well, when abnormalities of its digestive tract do not allow enough fats to be absorbed.
Ceramides are a special class of lipids or fats. They are found throughout the body. Those ceramides present in the skin appear to be depleted in itchy dogs. Recently, a group of topical ceramide-containing sprays and drops have become available for itchy pets. They seem to help decrease itching considerably better than the oral lipid products did. You can read about those compounds here and here. Add them to your pet’s treatment plan if they appear helpful – but be cautious about exaggerated claims for the products. One brand is Spot-on®.
Your Pet’s Future
Allergic dermatitis is a lifelong condition. Unless the problem is solely fleas, there are no cures. Luckily, it is not a life-threatening or a life shortening condition, and it can be managed with a minimum of inconvenience. Often, there will be periods of a year or more when the disease is not as severe and needs less or no medications. When a family moves, the disease is often left behind. Unfortunately, not too much time passes at their new location before the pet becomes allergic to new allergens. Because this is an inherited trait, pets with this disease should never be bred. The fact that so many pets suffer from allergic skin disease shows that many breeders disregard that advice.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.