When Your Cat Can’t Pee – Feline Urological Syndrome
aka FUS /Feline Lower Urinary Tract Disease (FLUTD)
Ron Hines DVM PhD
The problem that brought you to this page has many long names. These urinary tract problems are said to be responsible for 2-13 % of cat veterinary hospital visits. Many believe that the chances of your cat developing FUS is greater when it is being feed primarily a diet of dry cat food, rather than a canned, refrigerated or home prepared diet that keeps your cat’s urine more dilute. However, as you might expect, a Hill’s cat food-sponsored report published in 2020 still disputes that that dry diets are more likely to cause feline urinary tract disease than canned diets. Others have noticed that an indoor, versus an outdoor, lifestyle predisposes cats to this problem. That might be due to a lack of exercise and/or obesity. (read here, here & here) Many cat owners arrive at their veterinarian’s office believing that their cat just has an etiquette problem – either too much time spent in its litter box, urinating outside of its litter box or spraying furniture and other objects in the home. (read here) Other cat owners arrive, certain that their cat is straining because it is constipated. Occasionally, cat owners arrive because they believe that their cat is straining because it has worms. (perhaps they saw tapeworm segments on its stool). However, intestinal parasites are never the cause. When your cat can no longer pass its urine (already blocked) the signs quickly become considerably more severe than straining. Although both male and female cats suffer from FUS/ FLUTD ; it is only a life-threatening disease when your cat is a male. Female anatomy makes complete blockage of your cat’s urine passageway (urethra) considerably less likely to occur. The female urethra is shorter and wider. Litter box accidents and spraying occur in cats for reasons other than urinary tract blockages or irritation. (read here) But once a cat has one episode of lower urinary tract issues, it is likely to experience them again. (read here) When there is incontinence (dribbling) but no straining to urinate, spinal cord issues are the most common cause. (read here)
Feline urological syndrome, FUS, is a perplexing disease. Veterinarians and nutritionists still do not understand why one cat in the household develops urinary tract problems while other cats in the same household do not. Many suspect that in multi-cat households it has to do with cat hierarchy. When FUS/ FLUTD occurs, it’s the most common cause because sharp crystals have fallen out of solution in your cat’s urine while the urine is still in your cat’s bladder. Those crystals irritate the lining of your cat’s bladder as well as its urethra. Those crystals, mixed with cellular debris sloughed from your cat’s bladder lining, can then form plugs that prevent male cats from passing their urine. In female cats, the irritation those crystals produce cause her urination behavior to change. She has more urges to urinate. However, the wider diameter of her shorter urethra rarely allows for complete blockages. Irritation and inflammation in both sexes can progress to the point where blood or clots are also present in the cat’s urine. (read here) In a second form of FUS, bladder lining inflammation occurs without the formation of struvite or oxalate crystals. That form of FUS is called feline idiopathic cystitis. (read here) This problem can be controlled in some cats by feeding a diet high in quality meat, with the goal of keeping your pet’s urine pH between 6.0 and 6.4. (read here) On a semi-dry basis (=moisture ~10%), increasing high-quality meat protein content to 38-42%, fat content between 15-20%, and keeping magnesium content below 0.1% Cheap and not-so-cheap big box cat foods, dry and canned, are lower in protein. But more importantly, the protein they do contain is of the lowest quality. Consequently, they are also much higher in unwanted ash minerals such as excessive calcium, phosphorus, and magnesium that can form urinary tract sediment. The %s I supplied approximates Dr. Randy Wysong’s recipe for cats with urinary tract issues. These diets taste good. So, your cat will be tempted to eat more of it. You need to periodically weigh your cat to be sure it is not gaining unhealthy weight like the cat just below. Just eyeing your cat is not sufficient. Obesity is also a risk factor in FUS.

What Kind Of Cats Are Most Likely To Develop FUS?
Cats of any age can develop lower urinary tract problems. But the average age at which cat owners are likely to report the issue in their cat is about 4 years. It is quite uncommon for FUS to occur in a cat less than 1.5 years of age. Older cats also develop FUS/ FLUTD. But when they do, they usually have other underlying health or chronic stress issue. That stress might be a new feline arrival, a move to a new residence, the development of arthritis, or even a new feral cat taking up residence in the backyard near your cat’s favorite window. Some veterinarians claim to see FUS more frequently in Persian cats; others believe that Siamese cats have the problem less frequently than other breeds. But no one has confirmed that this is more than a coincidence. Until the early 1990s, the irritating urine crystals (“sand”) that veterinarians encountered in cats were usually composed of the mineral, struvite (ammonium-magnesium-phosphate). But through the 1993-2004 period, the number of urine crystals composed of calcium oxalate gradually increased to compose ~50% of the cases. After 2004-2008, the number of stones composed of calcium oxalate began to decrease and the number of struvite crystal cases to increase (today about 55% struvite). That might be due to changes in the ingredients of the commonly used prescription urinary health diets that vets sell. But as in humans, a multitude of other factors influence how often one or the other type occur. (read here & here) When discrete calculi (aka “stones”) can be visualized in your cat using x-ray or ultrasound, those detected in the cat’s kidneys or ureters, rather than in its bladder or urethra tend to be composed of oxalate. I think of this as the “Garfield Syndrome” because it appears to be a disease of easy living. It is most often a pampered indoor cat that develops this disease.
If My Cat Develops FUS, What Signs Might I See?
I mentioned that the first thing many cat owners notice is that their cat is spending too much time in its litter box and/or urinating outside of its litter box or spraying. You can read an article specifically about that problem here. I also mentioned that it can be hard to decide if your cat is straining to urinate or to poop. But it is usually obvious that there is a problem with one or the other when your cat squats too long or more frequently than it once did. If the consistency and color of its stool has not changed, its anal sacs are not impacted, and I palpate no hard stools in its colon, I suspect a urinary tract problem. Occasional cats will meow and show their discomfort while making their attempts in the litter box. Between attempts, they often lick their genital area. Your cat’s tongue is rough, so it isn’t long before the penis of male cats becomes red and inflamed. There may be blood in its urine. The penis of males may no longer withdrawn entirely into its sheath and might be an inflamed bluish red at its tip. There may be a white, cheese-like material surrounding its penis and sheath. Those cats are particularly prone to complete obstruct (urethra plug up) if they haven’t already done so. In that condition, they tend to find sinks, tubs, open drawers and closets particularly attractive as new elimination areas.

What’s Going On Inside?
I also mentioned that when FUS/ FLUTD occurs as small sharp crystals in your pet’s urine, those crystals irritate its delicate bladder and urethral linings. Less commonly, actual gravel-to-egg-size stones, rather than a fine sand form. In cases where those larger stones/calculi form, secondary bacterial infections are common. It is unclear if the bacteria change urine in ways that give rise to the stones, or if these porous stones give bacteria convenient locations to hide from your cat’s immune system and antibiotics. (read here) But most cats with an FUS/ FLUTD problem have very few dangerous, bacteria or virus in their urinary tracts. And when those bacteria are experimentally transferred to healthy cats, they cause no disease. When bacteria are found in your cat’s voided urine, they are often no more than normal contaminants or symbionts of your pet’s penis or vagina. (read here & here) But when certain bacteria are present in high numbers in urine obtained sterilely from your cat’s bladder through a needle (cystocentesis) they might need to be eliminated. Unfortunately, urinary tract protective bacteria will often be harmed as well. An antibiotic sensitivity test might avoid that risk. The presence of white blood cells in your cat’s urine is a common indication of a need to eliminate urinary tract infections.
Another theory is that lethargic, indoor cats on dry kibble diets do not consume enough water. Cats rarely do. In the wild, your cat’s ancestors subsisted on small rodents that were 70-80% water, so they rarely needed to drink. We know that struvite and oxalate crystals form more rapidly in concentrated (supersaturated) urine. However, just as veterinary scientists could not produce FUS with high ash diets, they couldn’t produce it with dehydration that produced concentrated urine either. (read here & here)
Struvite crystals form when the pH (acidity) of your cat’s urine is greater than 7 and possibly also when dietary magnesium levels are high. 6.7-6.8 might be a good goal, but veterinarians really do not know. When animal nutritionists realized this, they reformulated prescription cat foods to produce more acidic urine (as low as 6.3). This reformulation did lower the incidence of struvite crystals in house cats successfully. However, it apparently increased the number of cats that formed calcium oxalate crystals instead. So today, FUS / FLUTD diets have been reformulated primarily to keep your pet’s urine dilute and low in both struvite and oxalate components with a pH slightly below 7. There is no scientific evidence that other additions to those diets protect cats from either form of urinary tract stones. (ask me for Abigail’s PhD thesis)
Why Is This Problem So Much Worse In Male Cats?
Male cats have a narrower and longer urethra (the tube leading from their bladder to the outside) than female cats. If this passageway gets blocked by fine grit and swelling, your cat cannot urinate and will rapidly becomes quite ill, as toxins (the end products of normal metabolism) build up in its body. The diameter of this tube is particularly narrow when it reaches the distal end of your cat’s penis. The generalized illness produced has similarities to uremia. You can read about that problem here. In addition to a buildup of the toxic products of metabolism, the abnormally high urine pressure in a blocked cat’s bladder rapidly starves its bladder tissue of oxygen. Tissues starved of oxygen rapidly deteriorate, liberating even more undesirable compounds. Kidneys are very sensitive to urine back pressure caused by blockages farther down the tract. It does not take very long for irreversible kidney damage to occur.
Female cats with the same lower urinary tract problem are in distress due to the pain of an inflamed urethra. But because their urethra is shorter and wider, I have never seen one that lost its ability to urinate. In the few cats that develop actual bladder or kidney stones (calculi) that block urine flow, their sex is irrelevant – they can both obstruct.
Is This A Medical Emergency?
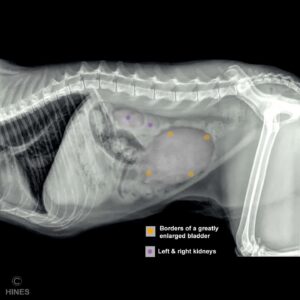
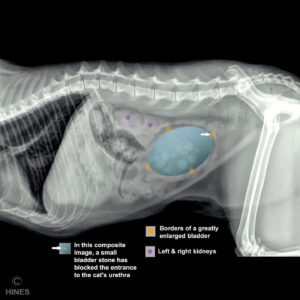
Urination is how your cat’s body cleanses itself of toxic waste. Urination is also critical for your cat to keep the proper balance of minerals and water in its body. It doesn’t take long (~24 hrs) for cats that cannot urinate to become depressed and for many systems in their body to begin to fail. If you can feel an enlarged orange to grapefruit sized bladder where I placed them in the diagrams above, yes, it is an emergency. If your cat’s rear abdominal area is painful, yes, it is an emergency. If your cat is weak, depressed, or apathetic, yes it is an emergency. If it has been attempting to pass urine for over 4 hours but has been unsuccessful, yes, it is an emergency. If your regular veterinarian is open for business, call, explain the situation and let him or her decide. If a trusted friend can suggest another full-service veterinarian, call there. FUS is a long-term problem that emergency animal hospitals are poorly equipped to handle. However, they are often the only option you have when emergencies occur after hours. That is why all cat’s that spend too much time at their litter boxes or pass blood in their urine need a veterinary exam before it becomes an emergency. You can experiment with cat litter that has color indicators, or even purchase medical urine dipsticks without a prescription that detect the presence of blood and bacteria. (read here) NEVER SQUEEZE ITS TUMMY FIRMLY. Obstructed bladders tear easily.
When urine backs up into your cat’s kidneys due to a blocked urethra, the pressure within both kidneys goes up. That can cause irreversible damage to their fragile kidney filters if the pressure is not relieved promptly. Three days with a blocked urethra is often fatal. When a blockage is present in one ureter, only the kidney upstream from that ureter is affected.
Experienced veterinarians learn to identify the male cats with FLUTD that are at the highest risk for future blockage. When the bladders of those cats are manually expressed, the stream of urine is quite narrow. Part of the reason could be anatomical, but often it is due to chronic swelling and inflammation of its urethra that is already present. Those are often cats that suffer from chronic urethral and bladder inflammation (idiopathic cystitis/urethritis) that leads to a swollen, narrowed passage for urine. Because of that, the urethras of those cats are more likely to be blocked or obstructed with debris. (read here & here)
How Will My Veterinarian Restore My Cat’s Ability To Urinate?
Veterinarians try to eliminate your cat’s urethral blockage in the least traumatic way possible. Catheterization, particularly with rigid catheters, carries the risk of traumatizing its fragile urethra. That can cause swelling that decreases the urethra tube’s diameter. If that should occur, the likelihood of your cat soon blocking again becomes much greater. I believe that an attempt should always be made (except for the most critically ill cats) to relieve urethral obstructions without catheterization. One author believes that over half of all obstructed cats can be unblocked without resorting to full catheterization. (read here) When a catheter is required, I have had better success using the much softer 22 G catheters designed for intravenous use in humans than those sold as “tom cat” catheters.
The common plugs that block male cats are composed of mineral crystals and cellular debris. That material has the consistency of cottage cheese. In many male cats, this plugging material is only compacted near the tip of their penis. In those cats, sedation, gentle massage of the penis and mild pressure on the abdomen often breaks down the plug and allows your cat to void its bladder with only a little hand assistance. Within a matter of hours, most cats regain bladder muscle tone that allows them to urinate on their own. This is the first method that I try. When successful, I follow that with generous amounts of subcutaneous injected fluids to maximize urination that helps flush out the remaining crystals. That extra subcutaneous hydration might need to be continued for several days to clear the urinary tract of debris.
When gentle pressure on the bladder and massage of the penis is not sufficient, many veterinarians, including myself, use a small, soft catheter to “jet” a stream of saline around the plugs to expand the urethra at that point, which encourages the debris to flush out. This is called retropropulsion. It is similar to veterinary “hydropropulsion” that is often effective in removing very small urinary tract stones that have blocked the urethra. (read here) If that is still unsuccessful, your veterinarian will probably have to catheterize your cat. In that method, one uses the retropropulsion technique to expand the urethra’s diameter as much as is safely possible. Then, a very small diameter, catheter is slowly advanced into your cat’s bladder. Sometimes the bladder has been over-distended so long that the urine it contains must be removed through the catheter with a syringe. The color, odor, and consistency of the urine is a good indication as to how long your cat has been blocked and how much tissue damage has already occurred.
These pets need to be heavily sedated or anesthetized when these techniques are attempted. Because many of these cats are already “toxic” with blood electrolyte imbalances, they are at a considerably higher anesthetic risk. Your vet is aware of this, and will adjust drug doses and monitoring accordingly. Once the blockage has been removed, your cat will probably be given intravenous fluids and buffers to correct those earlier imbalances, flush out its kidneys and encourage urination. Once successful, it is always wise to have your cat’s kidney function (BUN & creatinine) tested, a few days later to be sure that no lasting kidney damage occurred. Most cats requiring a catheter will pull it out if not wearing a sunflower-like (Elizabethan) collar. Your pet need to stay at your local animal hospital until the staff there is pretty confident your pet will not plug again. Depending on what is seen microscopically on urinalysis, your cat might also require antibiotics. Injectable medications to relieve pain and help relax your cat’s urethra are most often administered as well. When, for one reason or another, a cat has to be sent home before I am confident the problem is behind it, I suggest that the cat’s owner(s) bring the cat in twice a day to be certain its bladder is emptying and that it is doing as well as expected.

What Are My Cat’s Chances Of Full Recovery?
One of the most important factors is how long your cat was unable to urinate before the problem was discovered. The longer a cat remains unable to urinate, the sicker it becomes. The more time your cat’s bladder remains over distended, the more bladder tissue damage is likely to occur. The longer the urine pressure in your cat’s kidneys remains above normal, the more kidney nephron damage is likely to occur. A telltale sign that a cat might be prone to urinary tract obstruction is the presence of sandy material in the sheath and on the penis of a male cat’s penis. That is why every veterinary health exam should include an inspection of that area. That, plus a microscopic and chemical examination of your cat’s urine, might nip a potential urinary tract issue in the bud. Thankfully, most cat owners realize their cat has a problem early enough for your veterinarian to set things right. That includes removing the blockage(s), insuring proper hydration, and making lifestyle and dietary changes to, hopefully, prevent a reoccurrence.
However, for various reasons, a cat’s owner might not notice that their cat has a urinary tract obstruction. When that is the case, toxic products and blood constituent disturbances mount. I already mentioned rises in your cat’s blood BUN and creatine levels in those situations. They are just two convenient markers that veterinarians use to monitor a host of other undesirable products that the kidneys of normal cats dispose of through urination. Depending on how long your cat has been obstructed, BUN (aka SUN) can be greater than 80 mg/dL and creatinine greater than 6 mg/dL. Your cat’s blood potassium level can also increase to dangerous levels (> 8 mmol/L). Blood pH might also decrease to a dangerous level (< 7.1). You can view all the normal test blood values of cats here. Cats with subnormal body temperature (less than 96 F / 35.6 C) and a heart rate of less than 120 beats per minute are also at extreme risk. (read here)
What Medications Will My Cat Need?
Pain Control
As you can imagine, urinary track blockage or inflammation are very painful conditions. Pain control medications, butorphanol (Torbutrol®) and buprenorphine (Simbadol®) can help with that. Some veterinarians utilize medetomidine (Domitor®), another pain-relieving medication. Others combine more than one agent.
Other veterinarians find Non-steroidal anti-inflammatory agents such as meloxicam (Metacam®) sufficient. Metacam® is FDA-approved for cats as a single dose to control postoperative and other forms of pain. In cats, more than one dose has been associated with kidney damage. Perhaps I am overly cautious, but I never administer this product to cats. (read here & here)
Antispasmodics
One of the effects of antispasmodics is relaxation of your cat’s urethra and bladder muscles. When those areas are inflamed, they constrict in spasms, causing much pain and making a second urinary tract obstruction more likely. So, your veterinarian might administer one or more drugs to your cat in the hope that they might be helpful. However, most veterinarians now feel that they did more harm than good. Medetomidine, that I mentioned earlier for pain relief, also has some muscle relaxing, antispasmodic properties. Other veterinarians were administering oral medications primarily marketed for benign prostatic enlargement in men. They hoped those medications would relax your cat’s urethra and allow residual gritty sand-like material to pass. A common one given to cats was prazosin. However, a 2022 article indicated that that product did more harm than good. (read here)
Antibiotics
In most cases, they are probably unnecessary. (read here) But antibiotics are still commonly dispensed to cats that have had a FLUTD episode involving obstruction or near obstruction. The most common antibiotic dispensed is probably Augmentin®/Clavamox®. Clever bacteria use indwelling urinary catheters (a catheter left in place) as “ladders” to move up into your cat’s bladder and kidneys. (read here) So protecting your cat in that situation with antibiotics might be a wise thing to do. Also, cats with significant bladder damage due to over-stretching (bladder over-distention) have probably lost their natural resistance to bladder infections. In those cats, antibiotic “cover” (prophylaxis) might be a wise choice as well.
Stress Control
Obstructed cats need to be housed in a dimly lit, secluded room by themselves. They need to concentrate on urinating – not on the sounds and odors of distracting other cats, dogs or people. Tranquilizing them with medications such as acepromazine, at appropriate doses, can be quite helpful when required. Acepromazine combats dysphoria, it is not believed to lessen pain sensation.
Prazosin, a drug sometimes used to lower high blood pressure in people, or to allow aging men to pass their urine more freely, also has a calming effect. Some veterinarians dispensed it to cats in the hopes that it would both relieve their anxiety and, perhaps, aid blocked cats in eliminating urethral obstructions. But more recent studies in cats have not confirmed that. (read here, here & here)
Once your cat is back home, some cat owners rely on products like Feliway™ or catnip to minimize stress in their cat’s life. Others try to think back as to when urinary problems began and what life changes occurred for your cat at about the same time. That might have been a move to a new location, the introduction of another cat, or perhaps a diet change. If possible, try to return the situation to what it was before the urinary problems began. If you can’t do that, be sure your cat has some private space to itself. Cats have personalities as different as people do. Some cats just don’t like the company of other cats. Do what you can to give each of your cats its own separate space, food, water bowels, litter boxes and love.
In the future, do not neuter or spay your cats too young. If you are reading this article, you are a responsible cat owner. You are not going to let your cat indiscriminately breed. Let male kittens, mature for 7–9 months before having them neutered, so their urinary tract can fully form as Nature intended it to. Then neuter them. The beginning of the urge to spray is the right time. Female cats mature a bit earlier than males, but there are many long-term health benefits of delaying their spay surgery as well. Indoor cats do not contribute to the pet overpopulation problem.
Increased Water Consumption – A Longer-Term Benefit For Many Cats
The more water your cat consumes, the more dilute its urine will be and the less likely it will be that crystals and sediments will form. So encouraging your cat to drink is very important in our attempts to prevent future relapses. Pet food companies don’t want you to think about that because selling dry cat kibble is a very lucrative business. Increased urine production also helps flush crystals and debris out of your cat’s urinary tract before clogs can occur. Cats are not by nature big drinkers. They were designed by Nature to obtain all the water they needed from the rodent prey that they ate (rodents are 70-80% water). Changing your cat’s diet to a home-prepared or (less desirable) commercial canned cat food will supply it with more water. (read here & here) Cats can be very grumpy about accepting diet changes. They get set in their ways. So, alternatively, you can very gradually add a meat broth to the dry food that your cat currently eats to supply it with more water. Be sure that several water bowls remain full throughout the day. Try putting them in novel containers, fountains, and locations to increase your pet’s interest in them. Some veterinarians suggest distilled water. There is no harm in offering distilled water – but ordinary, tap water that meets EPA standards is just fine. You might also experiment with Hydra Care®. If you do, please let me know the results and I will post them on my Hydra Care webpage.
Urinary Acidifiers As A Treatment For Struvite Crystals
Struvite crystals dissolve when your cat’s urine is acidic. So, for a time, veterinarians dispensed a lot of urinary acidifying agents such as ammonium chloride or dl-methionine tablets and powders for cats with a history of struvite crystal or stone problems. Oxalate crystals and stones form in urine that is acidic, nothing we know of will dissolve them; but after surgery or mechanical removal of oxalate crystals or stones, veterinarians dispensed potassium citrate supplements in hopes of decreasing the chances of oxalate crystals forming again. However, the effects of all these products on urine pH is short-lived, and many cats find these products’ tastes objectionable. You are better off feeding a cat with urinary tract stones or sediment issues commercially produced canned cat foods that are low in ash, have higher quality protein content and have added electrolytes to encourage your cat to drink more water. Oral acidifiers need to be used with caution in cats that are already consuming a diet formulated to acidify your cat’s urine. If your cat is in the middle of an FLUTD crisis, feed a diet furnished to by your veterinarian, or hire a veterinary nutritionist service to guide you in preparing one yourself. Dr. Wysong’s recipe for cats with urinary tract issues is another good option – if you confirm that your cat is hydrating itself adequately.
If discrete stones are present that are too large to pass through your cat’s ureters or urethra, your veterinarian will have to remove them from your cat through traditional surgically or with the aid of sophisticated “basket & YAG (Ho:YAG) or TFL laser apparatus” available at a few large veterinary centers such as the AMC the RVC and the UQ. (read here)
Would Surgery Help My Cat?
I mentioned that traditional surgery or sophisticated laser apparatuses, passed up your cat’s urinary tract, are the only two ways to remove urinary blockages that are composed of oxalate – and some that are composed of masses of struvite. Those are the few cats with struvite-based FUS / FLUTD that actually have larger granules or struvite stones plugging their urethra or displacing urine volume in their bladders, rather than those with fine-grained “sand”. The only ones that can be dissolved by specialized diets are those that are composed of struvite which has not yet completely blocking the passage of your cat’s urine. Oxalate-based urinary tracts stone reoccurrence might be prevented by these special diets. Their makers claim that is true. But they do not dissolve stones that are already present. They admit that too.
When your veterinarian must be surgically open your cat’s bladder, the procedure is called a cystotomy. However, in the majority of cats, thankfully, this material is fine-grained and pasty. When male cats with this more common form relapse despite everything your veterinarian can do, the best solution may be a surgical procedure called a perineal urethrostomy. This surgery works best in male cats that block because they have an abnormally narrow portion of their urethra nearest the tip of their penis. But in which the remaining upper portion of the cat’s urethra is adequately wide. In those cases, plastic surgery, performed by your veterinarian, restructures (i.e., widens) that narrow portion to lessen the chances that debris and crystals will block that portion of the urethral channel again. The surgery does not prevent future crystals or debris from forming. Only a diet change, greater fluid intake, exercise, and weight loss for obese cats, will do that. When the surgery is complete, your cat’s privates will look allot like a female cat. This surgery can be the only option to save the life of a cat when diet, medication, and lifestyle changes do not prevent FUS / FLUTD reoccurrence. However, this surgery is not always successful. Occasional cats I have performed this procedure on appear more susceptible to subsequent urethral and bladder infections. So, they need to be monitored throughout their lives for urinary tract infections and treated appropriately. If discovered, those infections can be controlled or eliminated with periodic antibiotics. If cranberry extracts have any place in the treatment of FUS / FLUTD in cats when bacteria play a part in their illness remains unknown. (read here) Again, maintaining high water intake is critical to long-term success. A second possible complication is chronic irritation of the surgically remodeled area that causes obstructive granulation tissue to form. Only the natural lining of your cat’s urethra is resistant to the chronic dampness and constituents contained in its urine.
What Causes Feline Urological Syndrome?
The short answer is that veterinarians don’t know. On rare occasion, perhaps an underlying anatomical or metabolic cause might be detected. But in the vast majority of cats, no underlying anatomic or metabolic cause can be found. When veterinary school scholars don’t know the cause of something, they are prone to calling it “multifactorial” – vetspeak for we don’t know. We do know that overweight cats, cats consuming dry cat food, lazy cats, cats that do not drink adequate water or consume sufficient water from their food and cats in multi-cat households seem to be more at risk. But veterinarians see FUS / FLUTD is cats that do not fit into those groups. In those cats, some veterinarians believe that perhaps genetics, and even the age at which your cat was neutered might be contributing factors. Burmese and Himalayan cats are said by some to have more than their share of oxalate problems. On the average, oxalate problems are said to develop in cats at a somewhat older age than struvite-based problems. But that is when the symptoms were first noticed, not necessarily when they began. In some cases, cats with oxalate problems were found to have blood calcium levels that were elevated. (read here) In cases where struvite crystal formation is the problem, anything that causes your cat’s urine to be less acidic or more concentrated is thought to make the problem more likely to occur. (ask me for Abigails PhD thesis) Despite fancy cat food ingredient lists and deceptive cat food company media commercials, your cat’s nutritional needs are not the same as yours. (read here) Suspicion might also fall on cats receiving inappropriate diets for what is basically a carnivorous animal, or diets high in ash. (read here)
What Can I Do To Prevent A Relapse?
Your veterinarian has no way to predict the future for an individual cat such as yours. Some cats have only one incident of FUS / FLUTD in their live. Others have repeated episodes despite all that you and your veterinarian do to prevent them. Until we understand the causes better, I can only give you some general suggestions. It’s been said by some that the reoccurrence rate of FUS / FLUTD is about 35% – although that would be very hard to accurately document.
Here Are Some Of The Things That Might Help:
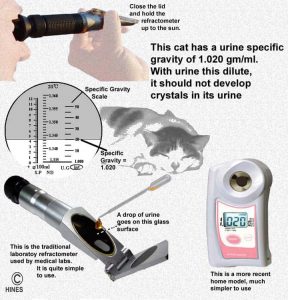
 Monitor the amount and characteristics of your cat’s urine at home for its specific gravity with a refractometer and for acidity and the presence of unseen blood, WBCs. or evidence of infection (nitrite+) with paper dipsticks similar to the ones in the second photograph above. Some 10-Parameters Urine Test Strips also report specific gravity, but they are not nearly as accurate as a refractometer.
Monitor the amount and characteristics of your cat’s urine at home for its specific gravity with a refractometer and for acidity and the presence of unseen blood, WBCs. or evidence of infection (nitrite+) with paper dipsticks similar to the ones in the second photograph above. Some 10-Parameters Urine Test Strips also report specific gravity, but they are not nearly as accurate as a refractometer.
 Do what you can to encourage your cat to drink more. The more dilute (the lower the specific gravity) of your cat’s urine, the less likely mineral sediments are to form. (read here & here) Give Hydra Care™ a try. Let me know how it affects the specific gravity of your cat’s urine.
Do what you can to encourage your cat to drink more. The more dilute (the lower the specific gravity) of your cat’s urine, the less likely mineral sediments are to form. (read here & here) Give Hydra Care™ a try. Let me know how it affects the specific gravity of your cat’s urine.
 Keep your cat’s litter box clean and place it in a low-traffic area. If you have more than one cat, have proportionally more litter boxes. Experiment with different brands of cat litter. (read here)
Keep your cat’s litter box clean and place it in a low-traffic area. If you have more than one cat, have proportionally more litter boxes. Experiment with different brands of cat litter. (read here)
 Feed a prescription or home prepared diet that is formulated to prevent struvite or oxalate formation. If you prepare it at home, you will need a board certified veterinary nutritionist at one of the Veterinary Colleges to furnish a recipe. (read here)There are many commercial brands on the market. None are scientifically known to be better than others. I much prefer that you feed the canned types over the dry kibbles. Dry chows are convenient, but cats that consume them tend not to drink proportionately more to meet their hydration needs.
Feed a prescription or home prepared diet that is formulated to prevent struvite or oxalate formation. If you prepare it at home, you will need a board certified veterinary nutritionist at one of the Veterinary Colleges to furnish a recipe. (read here)There are many commercial brands on the market. None are scientifically known to be better than others. I much prefer that you feed the canned types over the dry kibbles. Dry chows are convenient, but cats that consume them tend not to drink proportionately more to meet their hydration needs.
 Minimize stressful changes in your cat’s routine and environment as best you can. Some cats, like some people, are incompatible and do best when re-homed.
Minimize stressful changes in your cat’s routine and environment as best you can. Some cats, like some people, are incompatible and do best when re-homed.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.