All About Rabies
Ron Hines DVM PhD

Rabies is one of the oldest recognized diseases of man and animals – everyone knows a bit about it. Rabies is also the most feared of all diseases that humans can catch from animals. The ancients called it hydrophobia because of a mistaken belief that humans suffering from rabies were afraid of water.
The rabies organism is a bullet-shaped RNA virus, of the genus Lyssavirus in the Rhabdoviridae family. That family of virus most commonly affects plants and insects. (read here) Lyssavirus, like rabies and those that affect bats, are outliers in that family. Rabies has a mystique that rests upon its finality and the striking psychological disturbances the disease produces. That is why the ancient Greeks named the virus after their goddess of madness, Lyssa. The commonly pictured foaming mad dog is actually not the most common form of the rabies that veterinarians encounter. The only 3 cases I have seen all had the “dumb” or obtuse spacey form.
Eighty years ago, people in the United States usually contracted rabies from a pet dog and infected dogs were thought to be the largest reservoir of the virus in the United States. That was because back then, dogs were much more common pets than cats. Back then, it was also quite uncommon for dogs or barn cats to receive periodic preventive rabies vaccinations and dogs were considerably more free to roam. With today’s easy access to effective pet rabies vaccines and public compliance with vaccination laws, the epidemiology (dynamics) of the disease has changed. Now more than 90% of the reported cases of rabies occur in wildlife – chiefly carnivores and bats. And rabies passes from one wild animal to another most frequently without your pet or you entering the picture. All warm-blooded animals have the potential to catch rabies. It is the animal’s lifestyle and vaccination history that determines the likelihood.
The CDC is sluggish in maintaining their website rabies page. Figures still rely on their 2021 data, when 4,951 cases of animal rabies and 5 human fatalities occurred in the United States. That was an increase of 11.2% in total reported cases over the year before. All had been exposed to bats. None of these people had received post-exposure prophylaxis (PEP) rabies shots (read here) that usually prevent you from developing rabies – if one receives them before symptoms start. Since then, approximately 5,000 animal cases have been reported to the CDC each year. Ninety percent were in wild animals, not dogs or cats. Rabies is much more common in areas of the world where people of moderate means live in high density and where vaccination of dogs and cats is less practiced. For example, in the Philippines, there have already been 55 cases of human rabies through March of 2023.
As I mentioned, over 90% of the animal cases occur in wildlife rather than pets. In recent years, raccoons have constituted ~ 35% of the cases, bats ~ 24% of the cases, skunks ~ 24%, foxes ~ 7.5%, domestic cats ~ 4.5%, dogs ~ 1.25% and cows ~ 1.1%.
Raccoons are the most common carriers of rabies on the Eastern Seaboard of the United States – from the Atlantic Coast through the Appalachian Mountains. They are also the wild animal most likely to mingle with your dog or cat – particularly if you or your neighbors leave food for your pets outside. An added, and much more likely, threat than rabies that is due to an over-abundance of urban raccoons searching for food is that raccoons are a common carrier of leptospirosis and assorted gruesome parasites. In the rest of America, skunks are the most common carriers. In isolated pockets of Texas, Arizona and Alaska, rabid foxes are more commonly reported than in the majority of the United States.
In Canada in 2021 there were 101 reported cases of rabies reported in animals. Of those 1 was in an arctic fox, 74 in bats, 2 in cows, one in a house cat, 3 in dogs, 4 in raccoons, 1 in a red fox, and 15 in skunks. One human case occurred in 2007 in Alberta and another in 2003 in British Columbia. Wolves have been known to transmit rabies in Canada, in addition to the same common carrier animals found in the US. In 2022, there were 17 cases reported in Arctic fox, 56 in bats, one in a cow, 10 in dogs, 2 in horses, 7 in raccoons, 15 in red fox, 29 in skunks, for a total of 136 cases. There was one fatal human case of rabies in British Columbia in 2019.
When bats become rabid, it is almost always the large cave and grotto colony variety that are more likely to harbor the disease (Free-tailed bats =Tadarida) – not the solitary varieties of bat that you commonly see fluttering around lamp posts. Some of these bat colonies number into the 20 millions and in those colonies up to 2% show evidence of rabies exposure. (read here)
In 2009, human cases of rabies occurred in Texas, Indiana, Virginia, and Michigan. In the Texas case, the 17-year-old girl involved was the first known case of an unvaccinated human making a complete recovery after symptoms had already begun. This particular child went on a Texas camping trip two months prior to her illness, during which time several bats collided with her while she explored a cave near the campground. She is not the only person to recover from what most consider a fatal disease. (read here)
Through 2021, Hawaii is the only state that has never reported a case of rabies. And because Hawaii is rabies free, resident pets are not required to be vaccinated against rabies. However, entering pets must be quarantined upon arrival in Hawaii with three different options available ranging in cost in 2021 from $185 to $1,080 per pet.
The rabies virus attacks the brain causing encephalitis (brain inflammation), which destroys brain cells and ultimately causes death. The early signs of rabies in animals and man are variable and not specific. They can consist of fever, and a general malaise (discomfort, feeling unwell). In humans, a bad headache is often the first sign of the disease. As rabies progresses, neurological (brain-related) signs begin which can include confusion, aimless motion, agitation, blindness, paralysis, salivation, difficulty swallowing and seizures. Patients usually die within the following two weeks.
Although only a few human deaths occur in the United States each year, in southern Asia, many thousands of people die from the disease. Australia, England, and Antarctica are the only large geographical areas that are thought to be entirely free of rabies. In Europe, the primary carrier of rabies is the fox. In Africa, it is the jackal and in Asia as well as Puerto Rico, dogs and mongoose. (read here) In South America, vampire bats also spread the disease after feeding on rabies-infected cows. (read here)
My Family Or I Were Bitten By a Rabbit, Squirrel, Or Our Pet Rodent – Are We In Danger?
The US Center For Disease Control in Atlanta has not recorded a single case of human rabies derived from the bite of a squirrel or other rodent. Although it is scientifically conceivable for any warm-blooded animal to contract rabies, it is extremely unlikely. There have been cases of rabid rodents in the United States. Those were usually groundhogs that had fought with rabid raccoons or shared their burrows with skunks or foxes. (read here) I know of no public health official or expert on rabies that would suggest a series of rabies shots after a domestic rodent bite, but those decisions are made on a case-by-case basis at the city or county level.
What Are Some Factors That Would Put Me More At Risk of Rabies Exposure?
People most likely to handle or be exposed to injured and sick wildlife or stray pets are at the most risk for contracting rabies. An effective vaccine is marketed to immunize these high-risk individuals and I have had many of these shots during my career. The vaccine currently used in the United States to immunize humans is Sanofi-Pasteur’s Imovax® HDCV vaccine. Many years ago, rabies vaccines caused great pain, requiring the injections to be given in the stomach or abdomen. That is no longer the case. Dogs and cats that come into frequent contact with wildlife are also at a higher risk for the disease. Vaccines to protect these pets and their owners are highly effective.
How Is Rabies Transmitted?
Rabies (with rare exception) is only transmitted through the saliva of infected animals. Being licked by a possibly rabid animal is not dangerous unless the lick is across raw, broken skin. Kissing an animal will not put you at risk of rabies. The only very rare exceptions are through airborne transmission to people or animals that frequent caves with large populations of colony bats. In those bat caves, the virus can become airborne in dust and secretions. In that form, the virus can then be inhaled by passing humans and animals or passed through a bite from a bat. (read here & here)
After what is normally a few days of incubation, the rabies virus is present in large numbers in the saliva of infected animals. However, not every animal or person bitten by a rabid animal develops the rabies. Actually, less than two in ten untreated people bitten by rabid animals are thought to develop rabies.
What Are The Symptoms Of Rabies In Animals?
When a wild animal such as a raccoon or skunk is bitten, the rabies virus leaves the site of the bite and travels slowly through the animal’s nervous system. The virus enter the nerve endings nearest the site of the bite, and follows those nerves to the spinal cord and eventually reaches the brain – often 3–8 weeks later. But an exceptional case might take twelve months to make that journey. Most infected animals then go through one or more classical stages before they die from the disease. The incubation period in skunks appears to be longer than say foxes, leading to the misconception that skunks can become lifelong healthy carriers of the rabies virus. (read here)
Rabies is a quite variable disease. Classical or “typical” cases of rabies do not always occur. So just because a wild animal, dog or cat does not show one or more of the common symptoms of rabies is no guarantee that the pet does not have the disease. In wildlife, beware of normally nocturnal (nighttime) animals that are visible and out in the daytime. Beware of those that have lost their normal fear of humans. Beware of those that behave in ways that they usually would not. In ruminant animals like cattle, the most frequent symptoms are paralysis and vocalization. Some become aggressive. The incubation period before symptoms begin in cattle is also quite variable. Many believe that the farther the bite was from the brain, the longer it takes for symptoms to begin. In cattle, 1–2 months commonly pass before the animal appears abnormal.
The Prodromal Phase:
Following infection, the virus enters an eclipse during which its effects on the body are negligible. At the site of the bite, the rabies virus enters directly into the peripheral nerves or replicates in tissue at the bite site, entering the nerves later. In dogs, this phase of the disease typically lasts for two or three days. During the next period, the animal often becomes nervous and anxious. It may withdraw from contact. It may run a fever. Personality changes are common. Friendly dogs may become fearful or aggressive. Normally, fearful or aggressive dogs may become overly friendly. Some observers claim that the site of the bite itches or stings them because they frequently lick and worry the area. Some believe that cats go through these phases more rapidly than dogs.
The “Furious” Phase:
Once the virus has entered the peripheral nerves, it is transported via sensory and motor nerve fibers to the brain. The virus also spreads from the brain to other highly innervated (highly supplied with nerves) sites, including the salivary glands. This is the time that the virus becomes present in the animal’s saliva when a bite from the animal can infect others.
After passing through the prodromal phase, dogs and cats often pass through a stage characterized by irritability to stimuli of sight, sound, or touch. This stage might last from one to seven days. These animals might become restless, aggressive, or viscous. I have seen a dog in this phase chew the metal bars of its cage until it injured its mouth severely. Unconfined dogs, cats, and wildlife in this stage of the disease often roam and wander great distances in an aimless fashion. Eventually, these animals become ataxic (wobbly) and may develop seizures and die. The canine distemper virus can affect an animal’s brain in a similar manner. Cases of rabies and canine distemper can appear quite similar.
The “Dumb” Phase
Some call this the paralytic phase. Some animals develop this stage after a prodromal or furious period, others never experience a period of agitation. The “dumb” stage is the time when the nerves of the head and throat might become paralyzed. Animals in this state drool and walk about with their mouths agape (open). They are unable to swallow. Owners often think their pet in this condition has some object lodged in its throat. During a period of about a week, these animals become more and more paralyzed and finally die. More dogs pass directly into this stage from the prodromal stage never developing the furious stage of rabies. Cows in this phase often bellow and extend their necks as if their throat was obstructed. Occasionally, a farmer (or veterinarian) might attempt to remove a suspected apple or corncob from these animals’ throat, and in so doing become exposed to rabies.
How Is Rabies Diagnosed?
The traditional method of rabies diagnosis requires submitting the suspect animal’s brain to a laboratory for microscopic examination. The pathology of rabies infection includes cellular changes that denote encephalitis (brain inflammation) and myelitis (spinal cord inflammation). Blood vessels within the brain become surrounded with white blood cells (perivascular cuffing). Often, reddish globular inclusion bodies form within the nerve cells (Pyramidal and Purkinje cells) of two portions of the brain, the cerebellum and hippocampus. These inclusions are called Negri bodies. They are diagnostic for rabies. Today, fluorescent antibody tests and immunoenzymatic tests are supplanting the older microscopic search for negri bodies. (read here)
Is There A Successful Treatment For Rabies?
Traditionally, veterinarians and physicians said that there was no treatment for rabies.They thought that once the virus was present, death was inevitable. Other than the few cases I mentioned earlier, there are very few documented reports of survival from rabies in the literature. However, studies in tropical areas where vampire bats are common have found that a percentage of non-vaccinated forest-dwelling people carry antibodies against rabies. That most likely stems from successful recovery after a bite from a vampire bat that carried the virus. (read here, here & here)
If an unvaccinated dog or cat is bitten by a known rabid animal, public health officials in America generally recommend that the pet be destroyed immediately. If the owners are unwilling to agree to that and their county, local and state laws allow, animals have been vaccinated against rabies and placed in strict isolation for 6 months. In those situations, it is vaccinated again against rabies one month before release. In other localities, when the pet is current on its rabies vaccination, it is permissible for it to be revaccinated again against rabies and closely observed for 45 days. In my experience, decisions tend to be made on a case-by-case basis and decisions vary depending on the personal inclinations of the official making them.
When a human is suspected of having been bitten by a rabid animals, a combination of the human anti-rabies vaccine produced by Sanofi-Pasteur that I previously mentioned, with or without the addition of rabies immune globulin (RabIg), is given.
Rabies immune globulin contains antibodies that neutralize the rabies virus on contact. Whereas rabies vaccines require time to stimulate the body’s own immune response to generate similar antibodies. So RabIg is often given when time is of the essence or the bite was located on the face or hands (closer to the brain).
Veterinarians have always known that only a small portion of non-immunized animals and people who were bitten by a proven rabid animal develop rabies. I was taught that that was because the virus is not always present in the saliva or because teeth were probably wiped clean of saliva and virus by the clothing victims were wearing.
Preventing Rabies Infection
It is always a good procedure to vigorously scrub and disinfect all animal bites. However, the only certain way to prevent infection is prior vaccination or vaccination subsequent to being bitten. Laws throughout the United States and most other countries require periodic rabies vaccination of your dog and cat. Both modified (attenuated, weakened) live virus and killed virus vaccines are available. Some brands are approved for use in ferrets, horses, cattle and sheep as well as dogs and cats. These vaccines are quite effective and almost never fail. The problem is that less than half of the dogs and only one-in-ten cats in the United States receive their rabies vaccinations when they ought to. Vaccine manufacturers suggest that cats and dogs receive their first rabies inoculation at twelve weeks of age and then again when they are one year old. From then on, some vaccines require yearly booster vaccinations while others protect for three years. I always use three-year vaccines. But even though my vaccines are federally licensed and tested for a three-year duration of immunity, many States require that they be given annually. Excellent pre-exposure rabies vaccines also exist for people at high risk of animal bites. Over the years, I have had at least ten of them.
Oral rabies vaccination of wildlife with Raboral V-RG® has been used in the United States since 1990. (read here) When I first wrote this article in 2016, there were 15 states distributing this oral vaccine to raccoons. In 2022, there were ten: Maine, New York, Pennsylvania, Ohio, West Virginia, Massachusetts, Alabama, Virginia, Georgia, and Tennessee were using the same oral vaccine administered in baits to control rabies in their wild raccoon populations. That is done in the hope that reducing the incidence of rabies in wildlife will reduce the risk of your dog, cat or you being exposed to the rabies virus. Texas also distributed rabies vaccine baits for their wild gray fox and coyote populations. The vaccine is a recombinant vaccine made from a living canary pox virus that had been modified to carry the rabies antigen (protein) on its surface. This vaccine cannot cause rabies because it contains only the non-infective surface proteins of the rabies virus, not the rabies virus’ nuclear material which is necessary for the virus to reproduce. Only government entities have access to this oral vaccine.
Are There Alternatives To Frequent Vaccination For My Pet?
In the United States, how often your pet is required to receive a rabies vaccination booster is regulated by the laws of your individual state. Those laws are often slow to keep up with scientific developments or are just inclined to err on the side of caution when it comes to guarding public health. We now have federally approved and certified vaccines that are known to protect dogs and cats against rabies for at least three years. Yet, many states in America still require yearly rabies vaccine boosters for dogs and cats. Blood tests exist that can determine if your pet is – or is not still immune to rabies (the RFFIT test). But it will be up to your state or local public health department to decide if they will accept those test results in lieu of vaccination. Many municipalities do not.
What Have We Learned About Rabies in Ferrets?
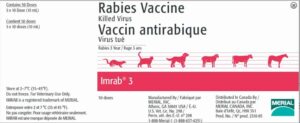
Until rather recently, American health authorities lumped domestic ferrets in with wild animals when it came to public health. This only began to change as the number of pet ferrets in the United States grew. Merial pharmaceutical company (now a part of Boehringer Ingelheim) saw an opportunity in testing and marketing their Imrab-3 rabies vaccine line for these pet ferrets as well as for the other species it had been tested on up to then. USDA approval of the vaccine’s use in ferrets was obtained in the 1990s. Although Imrab-3 is approved for three-year-protection in dogs, cats and sheep after the first and second year’s dose, it is only licensed for every-year use in ferrets, cattle, and horses. Studies were not conducted long enough to know how long beyond a year that immunity lasted. Imrab-3 vaccine is used “off label” in zoos around the world to protect a variety of animals from rabies. (read here)
The procedures for managing a pet ferret that has bitten a human are determined individually by each state or municipality in America. Although state and municipal laws regarding post-bite quarantine tend to be quite similar. But it is always wise for you to read your state and municipal quarantine statutes yourself, rather than rely on the advice or direction of an animal warden investigating a bite incident or complaint. The information that public officials convey to you is not always correct.
What Happens In The USA When Humans Are Bitten?
Whenever a domestic animal bites a human it should be quarantined for a 10-14 day observation period. Alternatively, it can be humanely destroyed, and its brain sent to a laboratory equipped to do rabies diagnostic tests. This is the only accepted option for non-domestic animals. State, county and municipal laws also determine the conditions of quarantine. Conditions may differ for vaccinated and non-vaccinated animals. If the biting animal cannot be located for quarantine or if it should prove to have been rabid, a series of five inoculations of human immune globulin are generally given. Individuals at high risk of bites usually receive a three shot series of human diploid cell line vaccine to ensure that they do not develop rabies. After that 3-shot series, some get yearly re-vaccinations; others just check their blood anti-rabies antibody titer to be sure it is still protective (greater than or equal to 0.5 IU/ml serum).
What Happens When I Get Bitten?
Subsequent to an animal bite, the type of post-exposure treatment your physician decides upon depends on what part of the world you live in and the type and circumstances of the exposure. Whether you have previously been vaccinated against rabies is also a consideration. Unvaccinated people often receive five, 1-ml doses of human rabies vaccine plus one initial dose of human rabies immune globulin. If the individual was previously vaccinated for rabies, they often receive two, 1-ml doses of rabies vaccine and no immune globulin. (read here)
Rabies is a frightening disease. Laws and procedures frequently change, and they differ from area to area, state to state and country to country. If you or your pet have potentially been exposed to rabies, do not rely on my advice to be the most current or to be applicable to your particular situation or locality. Speak to your physician, your local veterinarian and an animal control supervisor to determine what needs to be done.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.