Vaccination of Zoo Animals, Wild Animals and Exotic Pets
Who Gets What And When
Ron Hines DVM PhD
 All Of Dr. Hines’ Wildlife Rehab Articles
All Of Dr. Hines’ Wildlife Rehab Articles
Where does this information come from?
None of the uses of the vaccines that I discuss here – other than a few, used in domesticated ferrets, mink and a few non-domestic hoof stock – are governmentally approved for the uses I mention anywhere in the world. They are all off-label uses given at your or your veterinarian’s discretion. Because one or the other was safe or worked well for me or for others is no guarantee that it will work well for you. There has been immense consolidation and name change in the veterinary pharmaceutical industry. Some products I mention have been discontinued due to low demand; others have been re-christened with new names.
Few animal collections have identical vaccination programs – even when a specific disease risk appears quite similar due to collection size, husbandry and geographical location. On the whole, zoos and private collections in the United States and Canada vaccinate their animals considerably more frequently than those in Europe, Asia, or Southern Africa. (ref) As to be expected, animal collections in economically developed areas are more likely to have vaccination programs than collections housed in the less developed World. However, it is not clear that vaccinated collections have less overall mortality than well managed facilities that do not.
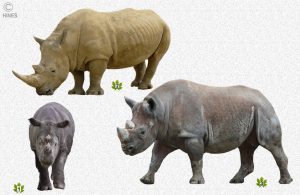
Dog-like Animals (canids and hyenas )
I included hyenas and aardwolves in this photo-group – But, genetically-speaking, they appear to be more similar to cats.
Canine Distemper
The most important vaccination that dog-like animals receive is against canine distemper. Because of uncertainties as to the safety of live virus vaccines in non-domestic canines, many zoos relied on Merial/Boehringer Ingelheim ‘s PUREVAX® ferret canine distemper vaccine (a “subunit” vaccine) given subcutaneously at ~ 12 weeks of age and repeated three and six weeks later. In exceptional or very high-risk situations, one might add an earlier vaccination. Many zoos give a canine distemper booster annually, although immunity probably persists much longer. That vaccine was not always available in 2013 and is unavailable as of this writing in 9/2014. Merial/Boehringer Ingelheim cites the complicated manufacturing process as the reason. Although it is only approved for domestic dogs, many zoological facilities that once relied on PUREVAX® are now using Nobivac® Puppy DPV , a product marketed by Merck Animal Health.
Healthy wolves and coyotes have no problems receiving any of the US or European–licensed canine distemper products for dogs (without leptospirosis). But other canids, particularly grey and fennec fox, maned wolves, cape hunting dogs and bush dogs have become ill subsequent to receiving dog combination-vaccine products. Which portion of the vaccine (if any) that caused the problem is unknown and unverified.
In the absence of Merial/Boehringer Ingelheim ‘s PUREVAX® FERRET , one of the safest product for those species is probably the Duramune Max 5 product (w/out lepto) sold by Boehringer Ingelheim and used extensively without problems in the US and Canadian 15,000-animal fox industry or NOBIVAC® PUPPY-DPV used extensively “off-label” in ferrets in the Netherlands, UK and the USA.
RECOMBITEK® C3 Sold By Merial, which contains an incomplete (non-infectious) distemper virus, should also be a safe alternative (ref) ; although I know of no zoos or breeders using it in what might be the more sensitive canid species.
In some areas of the World, Merial’s PUREVAX® FERRET was never available. The Johannesburg and Pretoria zoos in South Africa have their own inactivated canine distemper vaccine produced by a local laboratory ( Design Biologix,Pretoria,SA )
UC Davis veterinary school vaccinated California Island Fox, a subspecies of Gray Fox, using Merial/Boehringer Ingelheim ‘s PUREVAX® FERRET Distemper vaccine. It took two vaccinations to produce measurable antibodies against canine distemper. However, after a few months, those antibodies could no longer be detected. Whether the fox were still protected remains unknown (adequate protection can still be present against virus even when blood antibody levels have dropped or are undetectable [ref1 ref2] ). They also administered IMRAB®3 rabies vaccine to Island Fox with no observable ill effects.
(gray and fennec fox in captivity experience considerably more mortality (deaths) than red or arctic fox. Some believe they experience more vaccine-related reactions as well.)
Canine Parvovirus
If you used one of the combination distemper/parvo vaccines I spoke of, the canid is already protected. If not, the safest procedure for a valuable wild canid whose ability to tolerate a modified live virus canine parvovirus vaccine is unknown is to use a killed feline parvovirus (panleukopenia) vaccine (such as Merck’s Panagen) for the initial vaccination. Once it develop even a low titer (≥1:40), you have the option of giving a modified live virus parvo vaccine from then on for the longer-lasting immunity those vaccines generally provide. Titers that develop using cat panleukopenia vaccines are not always as high as we might wish. More about canine parvovirus here.
As with some canine distemper vaccines, modified live virus vaccines against parvovirus have occasionally been suspected or accused of causing the disease in captive wild canids (bush dogs). However none were adequately document to prove that it was the vaccine that initiated the subsequent problem. In red wolves, at least, obtaining protective parvovirus titers ,even with MLV parvovirus vaccines, appeared more difficult than protecting the animals against canine distemper with the vaccines available at the time.(ref)
If A Vaccine Worked Safely In One Member of This Group Does That Mean It Will Be Safe In All Members Of This Group?
Not necessarily so.
The majority of captive, non-domestic animals reside with breeders or are maintained in zoos. Zoos often display the rarer eye-catching species. Commonly, the number of animals that formed the initial breeding stock of that species was quite small. Although there may be many of the species now, they often share the problem of consanguinity or inbreeding. They do not have the larger and safer gene pool of their wild ancestors.
In other species, such as cheetahs, ancient genetic bottlenecks in their history reduced their number during catastrophes unknown to us today. Those catastrophes are thought to account for the cheetah’s increased health risks among wild large cats. (ref) In others, such as red pandas, (ref) and black-food ferrets (ref), fragmentation of their habitat probably accounts for their small gene pool and fragile health in captivity. In still others, like the California Island grey fox, isolated on small coastal islands, sea level rise ended their intertraficing with the mainland and kept their genetic diversity low. In expansive ranges in the wild, inbred animals are naturally weeded out. (ref1 ref2 ref3) With a lack of genetic diversity the immune system is sometimes compromised. (ref) Us humans are not immune from that effect either. (ref)
Astute veterinarians have noticed that adverse vaccine reactions seem to be more common in certain “rare breeds” and inbred lines of dogs. (ref) This phenomenon probably occurs throughout the animal kingdom.
Some warning signs of a low genetic diversity animal population are breeding failures, small litter size and high infant mortality. But that is not a hard and fast rule.
Rabies
In some jurisdictions, it is illegal to administer rabies vaccine to non-domestic animals. When given, jurisdictions may refuse to differentiate between vaccinated and unvaccinated animals that have bitten humans. Never-the-less, many facilities vaccinate all canids in their care against rabies. My personal preference in all species is Merial/Boehringer Ingelheim’s IMRAB® – sold outside of North America as RABISIN®. (ref) But the wildlife veterinarians associated with Pretoria’s Onderstepoort , vaccinate their wild canids with Merck’s Nobivac beginning at 3 month of age and then yearly. More about rabies here. Do not assume that every single rabies-vaccinated animal will be protected. ( read here )
Most localities have strict laws regarding rabies vaccination of animals and the disposition of animals that have bitten humans. Those regulations are not always based on science – but they are best followed.
Some Rabies Vaccination Protocols Used Around The World In Caninds
The Jerusalem Zoological Gardens, Jerusalem, IL, vaccinates all their wolves against rabies with RABISIN® once every three years and against other dog diseases with Zoetis’ Vanguard Plus 5.
The National Zoo, Washington, DC vaccinates all canids every three years against rabies with Merial/Boehringer Ingelheim ‘s IMRAB®3. Canine distemper vaccine boosters are given annually. Their red wolves receive a standard, multivalent MLV DA2LPP vaccine booster yearly but their fox and maned wolves only Merial’s canary pox vectored ferret CDV vaccine.The SanWild Sanctuary, SA, vaccinates injured and immature wild South African jackals against rabies before they are returned to the wild. No other vaccines are given.
As late as 2014, approximately 15,000 fox were raised commercially in the United States to supply the fur industry. Their vaccine of choice is Duramune Max 5®. (Ft. Dodge Company structure has changed multiple time: Wyeth, Pfizer, Boehringer Ingelheim, Zoetis) In the many years that it has been administered to foxes, none, to the knowledge of their national organization, is known to have developed canine distemper. The vaccination schedule used for puppies and dogs is followed, but booster vaccinations are generally not given. Their umbrella organization, The Fox-Shippers Council, suggests avoiding the Duramune Max 5 + Lepto. Severe reaction to leptospirosis vaccinations commonly occur. (ref) Other US fox breeders that I know of use Pro Lab’s Univac 7 or Zoetis’s Vanguard Plus 5®. Most of the fox breeding industry has now moved to China and persists, for now, in Scandinavia.
Most US fox breeders bred Red or Arctic Fox. Those breeding Fennec and grey fox seem more reluctant to vaccinate with vaccines designed for dogs. Similar reluctance to vaccinate with living products (MLV vaccines) occur and are known have occurred in cape hunting dogs, South American bush dogs and maned wolves. ( ref1 ref2)
Leptospirosis
The mixed high-density wildlife populations of zoos, their urban settings among dogs and their tendency to attract vermin (rats and raccoons) make leptospirosis vaccination of dog-like animals a plausible option as well. Leptospirosis vaccines are all killed, inactivated products that protect against all 4 common leptospirosis serovars. As with dogs, the dose of vaccine given really needs to be adjusted to the animal’s body weight. ( rptref ) When the potential for exposure is high, leptospirosis vaccines need to be given yearly. Very few collections administer this vaccine. More about leptospirosis here.
When exotic canids were born of vaccinated parents and raised by their parents, there is no need to begin vaccinations for canine distemper and canine parvovirus before 12 weeks of age. As is domestic dogs, parental (colostral) immunity can interfere with the effectiveness of vaccines given before that age. A booster vaccination at 16 week (or older) is also important to insure an adequate immune response in case the first dose was not fully protective. After that, yearly antibody titer tests are the most reliable way to determine when and if booster vaccinations are required. Lacking that, follow the recommendations on revaccination frequency given on the product insert.
Canine Adenovirus
Most combination products I mentioned for immunizing against canine distemper also immunize against CAV-1. Canine adenovirus 1 (CAV-1) is responsible for canine infectious hepatitis in dogs and encephalitis in fox. Canine adenovirus 2 (CAdV-2) is one of the many causes of kennel cough of dogs. Vaccine immunity to either adenovirus protects against the other. Since CAV-2 is less likely to cause eye complications (blue eye) it is the one that is generally incorporated in dog vaccines in a living but weakened (attenuated) form. A few suggest canine parainfluenza-containing vaccine as well (even though I know of no recorded cases of the disease in wild or zoo canids). You can read about another case where the vaccine was thought to be responsible for the disease in a maned wolf here. More about canine adenovirus here.
Feline Panleukopenia
The parvoviruses that cause parvovirus disease in dogs and panleukopenia in cats are quite similar and appear to commonly mutate and recombine with one another. Although vaccination for one is thought to induce immunity to the other, that is not yet entirely certain. An interesting recent article documents the feline panleukopenia virus’s ability to infect foxes and multiple other carnivore species in southern Europe. You can read that article here. Merck’s Panagen® non-adjuvanted, killed panleukopenia vaccine should be protective. Read more about feline panleukopenia here.
Hyenas And Aardwolves
Hyenas and Aardwolves look like dogs. But genetically, they are a closer relative to the felines in the second image on this page and the civet-like viverrids in the fifth. Their unique genetics make them susceptible to feline as well as canine distemper. Feline distemper is also called feline panleukopenia. Killed virus vaccines designed to protect house cats from that disease work well in hyenas and aardwolves. The Fel-O-Vax line of cat panleukopenia vaccines are often given. Although they contain other killed virus ingredients, they apparently cause no ill effects. In addition, hyenas and aardwolves need protection against dog distemper and rabies with the same vaccines suggested for wild canines. Vaccination frequency is generally yearly or based on antibody titer. Not all authorities agree that hyenas and aardwolves are even susceptible to canine distemper. ( ref1 ref2 )
When vaccinating hyenas for canine distemper, zoo veterinarians prefer killed canine distemper products or the Merial PUREVAX® FERRET recombinant canine distemper vaccines, which has been so difficult to obtain recently – although there is some thought that even that canary pox- vectored vaccine might have the potential to cause illness in hyenas on occasion. (ref)
Vaccines For Cats Of All Sizes
The great size of some of the wild cats does nothing to change the outcome when they are infected with the common disease of domestic cats. Exposure is generally through feral small animals attracted by the availability of food. The current surge in the establishment of urban feral cat colonies make this ever more likely where that practice is tolerated. (ref)
Feline Panleukopenia (FPV)
The most important vaccination for non-domestic cats is probably one that includes protect against panleukopenia (feline parvovirus). Fortunately, killed panleukopenia-containing vaccines are readily available and quite effective. When properly administered, all provide immunity that generally lasts for many years. Vaccines marketed for panleukopenia usually also contain, at a minimum, feline herpes virus and feline calicivirus. Read more about feline panleukopenia here .
The most common brand used in wild felines housed in zoological, breeding and display situations around the world is Zoetis’ Fel-O-Vax IV+ – a formulation of killed (inactivated) panleukopenia, rhinotracheitis/Herpes1, calicivirus and Chlamydia psittaci. As in house cats, the vaccine will not prevent calicivirus or feline herpes-1 virus infection – but it usually keeps the infection mild or unapparent until the cat’s antibodies can eliminate the virus or cause it to go dormant. Some use Fel-O-Vax IV, but since calicivirus has been documented in exotic cats, IV+ is probably the better choice. One mL has traditionally been given to cubs and kittens every 2 weeks from 8 weeks to 16 weeks of age and then a booster at 6 and 12 months.
I generally vaccinated at 12 and 16 weeks of age and again at 12 months with a booster every 3 years thereafter. It can take several weeks for initial protective antibodies to form. Vaccine administered to stress animals or those in less than excellent health are less likely to be as effective. Based on recent recommendations for domestic cats many institutions do blood titer determinations after 12 months and only revaccinate those animals whose titer is low. Over-vaccination is thought to lead to an increased risk of fibrosarcomas and various other immune system-related problems. The interpretation of a low or no titer animal’s need for booster inoculations can be difficult because vaccinated animals have other important defenses beside antibody (immunological memory). Cornell University staff are known for their particular interest in these titers in non-domestic species. (ref)
Although an unproven procedure, I also give twice the dose suggested for house cats to the large panthera cats in hope of delivering an antigen mass appropriate for their high body weight – although most veterinarians still give only the label’s suggested dose for house cats. Generally, vaccines contain considerably more antigen than what is minimally required for protection.
Most veterinarians specializing in zoological species in the USA do not administer modified live virus vaccines, such as Zoetis Felocell® or Merial/Boehringer Ingelheim ‘s PUREVAX® feline line to exotic felines. But I know of a Florida veterinarian who has administered Merial’s PUREVAX® FELINE 4 (MLV feline rhinotracheitis, calici, and panleukopenia Chlamydia psittaci) ; as well as Purevax Feline Rabies 3 year recombinant canary pox vaccine to a number of display tigers and cougars with no apparent ill effects. Some European zoo trials used MLV feline vaccines (Feligen CRP) in lions and tigers as well. (ref) Doing so with the MLV cat vaccines available in the US does not necessarily mean the cat will become ill. I also knew of two young unimmunized Florida circus tigers that were given the Zoetis/Pfizer’s Felocell-R3, MLV live product, by accident. Neither developed any visible illness during the following year I observed them.
Zoetis’ Fel-O-Vax IV+ contains inactivated calicivirus. Since feline calicivirus replicates in large non-domestic cats (lions, tigers) as well as smaller species and is capable of causing illness in them, it would be my current vaccine of choice in non-domestic felines. (ref1 ref2)
Herpes Virus 1 (FHV-1)
This most stubborn respiratory and ocular virus was once called the feline rhinotracheitis virus. It rarely kills, but sometimes debilitates. Once infected, all felines carry the virus for life. Vaccines are not particularly effective in halting its spread. (ref) Read more about herpes virus 1 here.
Among non-domestic felines, cheetahs suffer the most from FHV-1, where it is usually passed from a carrier mother to its offspring. That is why many zoos begin vaccinating cheetah cubs at 6 weeks of age. Some vaccinate pregnant females with killed FHV1-containing vaccine in an attempt to boost protection in their offspring. In cheetahs, the signs of a herpes-1 virus infection can be quite different from its appearance in house cats and often involve skin and facial ulcerations as well as eye and respiratory symptoms. (ref1, ref2, ref3)
It is not only cheetahs that are at increased risk of FHV-1, pallas and black-footed cats in US zoological collections have also suffered debilitating outbreaks of FHV-1 (in some cases, use of a live virus containing vaccine was thought the possible cause).
High antibody titer does not necessarily protect felines against infection with FHV-1, but it tends to lessen the severity of any symptoms that may develop after an exposure.
Fel-O-Vax IV is the vaccine most commonly used to impart FHV-1 protection in non-domestic felines the world over (worldwide).
Rabies
Most zoos and private collections rely on protections against entry of rabies virus into their facilities rather than on vaccination of their exotic cats. Many vaccinate their staff against rabies rather than their animals.
However, some jurisdictions (such as France) require rabies vaccination before an animal can enter their borders. Others vaccinate specific demonstration, mascot or show animals that get in close proximity to the public where bites will be more likely. Protective titers across species are considered to be >0.5 IU/mL (21 days after inoculation). although lesser titers sometimes also protect. Read more about rabies here.
When the decision is made to immunize exotic cats against rabies, Merial’s IMRAB®3 (given at 3 month of age and again annually and then annually or every 3 years according to local regulations) has caused me no problems. It is often given at yearly intervals in the USA in keeping with state laws that specify yearly rabies vaccination regardless of label claims. Other institutions have found that Rabvac3 and PUREVAX® feline rabies vaccines are equally as safe. I give larger species twice the dose intended for house cats. I believe the Houston Zoo does (or did) as well. An alternative is a second standard injection 2-3 weeks after the first.
Canine Distemper (CDV)
Canine distemper is a true and present danger to free-roaming large African cats and tigers on Indian (India) reserves that have close association with unvaccinated village dogs. It is a considerably lesser threat in most zoological setting – greatest in drive-through parks, animal “sanctuaries” or where raccoons have easy access to the facilities. In those situations, vaccination is quite prudent ; in others, it is the staff veterinarian or director ’s call. Some US zoos, like Rolling Hills Zoo, KS, Louisville Zoo and Henry Doorly Zoo, NE administer it, others, like the National Zoo do not. Read more about canine distemper here.
Most cases have occurred in panthera genus, but cases have also been reported in lynx and bobcats. (ref)
When veterinarians elected to protect exotic cats against canine distemper, they used Merial/Boehringer Ingelheim ‘s PUREVAX® FERRET recombinant canine distemper vaccine marketed for ferrets. The standard 1ml dose size given intramuscularly at yearly intervals is said to be sufficient. I know of no side effect having occurred and I know of no vaccine failures under well-supervised conditions. But one Tufts Veterinarian questioned the effectiveness of that vaccine when, five of six lions and tigers that died in a Texas refuge outbreak had received prior vaccinations with the Merial product. It is hard to verify what actually occurred. I know of no other reports of vaccine failure with that product in the many other exotic species in which it is used.
With PUREVAX® FERRET recombinant ferret distemper vaccine currently unavailable in 2014, my choice vaccine for canine distemper protection in large felines would be Merial/Boehringer Ingelheim ‘s Recombitek C3 canine vaccine (rDACPP). It combines the same canary pox-vectored distemper virus that was in PUREVAX® FERRET with weakened (MLV) canine Adenovirus Type 2 and canine parvovirus. However, the virus mass in that vaccine is only one third the amount that was present in PUREVAX® FERRET. Should Merial’s PUREVAX® FERRET return to the market or another safe alternative become available (such as a CDV-ISCOM subunit inactivated virus vaccine (ref1, ref2), I would consider them first because of they are monovalent with recombinant and inactivated safety. (In early 2015, Merial’s canary pox-vectored, univalent, canine distemper vaccine came back on the market with a dog and puppy label and somewhat lower titer. It should be just as safe in felines as PUREVAX® FERRET.)
In 1994-1995 four orphan adult lions were given Novibac distemper vaccine at the Masai Mara wildlife reserve in Kenya. All developed good titers without noticeable adverse clinical effects. (ref) But 4 lions does not a study make – even the virulent “wild” canine distemper virus only kills one out of three free-ranging lions. (ref)
Feline Leukemia (FeLV)
Non-domestic feline occasionally experience mortality due to the feline leukemia virus both in zoos and in fragmented natural environment that increase their contact with feral cats. In situations where the likelihood of exposure to stray cats is high, vaccination of captive non-domestic felines with Zoetis’ Fel-O-Vax LV-K is prudent. That is also the recommendation of the Siberian tiger advisory committee (SSP). A two-dose primary series at 8 and 12 weeks of age, and a booster 12 months later. Some facilities continue with yearly booster, but there is evidence that vaccines can protect up to 2 years in domestic cats. (ref) Read more about feline leukemia here.
However, the flagship book on zoological medicine recommends against routine vaccinating non-domestic felines against feline leukemia and feline Immunodeficiency virus (FIV). (ref) Others in the zoo community have express similar views : “no exposure- no risk” But for private breeders of the smaller wild feline, mixed domestic-non-domestic collections, highly inbreed feline species, crowded or high-stress situations or zoos increasingly unable to halt the intrusion of feral domestic cats due to local public sentiments – vaccination against feline leukemia is probably wise.
Feline immunodeficiency virus (FIV)
The same factors I mentioned for FLV pertain to the risk of exposure to FIV. However, I know of no facilities using the currently available vaccine (Zoetis’ Fel-O-Vax FIV). Because this current FIV vaccine appear to be of limited value in protecting house cats and because its use can confuse diagnosis in ill animals, few if any veterinarians suggest vaccinating domestic cats with the product either. The FIV virus does occur in many wild felines. Whether it commonly causes disease in them remains to be determined although it has been diagnosed as a cause of disease in snow leopards, lions, pallas cats etc. (ref) Read more about FIV here.
Feline Infectious Peritonitis (FIP)
FIP is caused by a mutant feline coronavirus. It has been an occasional problem in captive cheetahs. (ref) Because this vaccine has been of limited or no value in house cats, most zoos do not administer it. But Primucell intranasal FIP vaccines has been given intranasally to Servals and cheetahs with no side effects that I am aware of. Read more about FIP here. Read more about FIP here.
Parvovirus of Dogs (CPV)
Non-domestic felines have the potential to be infected with dog strains of parvovirus, cat strains and probably raccoon and mink-adapted strains as well. These virus are all thought to have originated in domestic cats and later moved to other species. (ref) Because of their close similarity, vaccination against the feline form (panleukopenia) is thought to provide a measure of protection against canine strains – but a mild or unapparent infection might still occur. (ref1, ref2, ref3) Read more about parvovirus here.
Tetanus And Leptospirosis
Non-domestic cats, like all mammals, are susceptible to tetanus and leptospirosis. I do not know of either being a specific problem in exotic cats, but some 1997 AAZA guidelines suggest vaccination for tetanus (ref) and leptospirosis be considered on an annual basis “where the diseases are “endemic” and more recent publications suggest they be considered “high-risk collections”. Both are rarely – if ever – given. Read more about tetanus here and leptospirosis here
Some Vaccination Protocols Used Around The World In Felines
The National Zoo, Washington, DC, vaccinates their non-domestic felines annually against panleukopenia and calicivirus using Fel-O-Vax®3. IMRAB®3 rabies vaccinations are administered every three years.
There are many breeders and collections of smaller exotic felines in the United States (bobcats, Servals, caracals, lynx, Geoffoy’s cat, leopard cat, etc. ). The many with whom I have had contact, all administer Boehringer Ingelheim’s Fel-O-Vax brand. Some only vaccinate them as kittens with a two injection protocol – more often at 8, 12 and 16 weeks. Fel-O-Vax IV is most often used. Adult felines rarely receive annual boosters after their first year. Minnesota breeders I have spoken to tell me they dod not recall a single case of feline distemper (panleukopenia) in 1000+ ranched bobcat and lynx that had received only their initial 3-shot juvenile vaccination. A few vaccinate their felines against rabies with Zoetis/Ft. Dodge’ Rabvac (1or3) every 1-3 years. Most do not.
The Helsinki Zoo, Finland has a geographic location, minimal local intensive animal production (compared to central European countries) and strict legislation concerning animal diseases that keep their risk of contagious diseases very low. Never the less, they vaccinate all their exotic cats with Fel-O-Vax IV because feral house cats are a perceived threat.
The Jerusalem Zoological Gardens vaccinate all their exotic felines (tigers, lions, leopards, servals and cheetahs) with Fel-O-Vax IV + Calici. Display animals likely to come in close contact with the public also receive yearly rabies vaccination. Those less likely to be in close proximity to the public, every three years. They have no choice as to rabies vaccine brands because a solicitation of bids for the entire country is placed by the Agriculture Ministry and they must accept the lowest international bidder.
The Kristiansand Zoo, Norway, vaccinates its panthera and smaller non-domestic cats with Fel-O-Vax IV. Rabies vaccination is only given when animals are being shipped to zoos in countries that require it (eg France).
The SanWild Wildlife Sanctuary, Letsitele, South Africa vaccinates their caracals (desert lynx) against rabies before returning them to the wild. No other vaccinations are given.
Veterinarians associated with Pretoria’s Onderstepoort veterinary school, who service the
National Zoological Gardens vaccinate all captive wild feline with Fel-O-Vax IV at three month of age, again 3-4 weeks later, and then yearly. They suggest these cats receive Merck’s Nobivac or Merial’s Rabisin® rabies vaccine annually as well. They are fortunate in that a locally produced, killed canine distemper vaccine is available to them as well. (Design Biologix CC).
Orana Wildlife Park, Christchurch, is New Zealand’s only open-range zoo.
The only carnivorous animals they vaccinate are their cheetahs, lions and tigers, using Zoetis’ Fe-O-Vax3®.
The Leopard Cat Foundation of Bonnieville, KY administered Fel-O-Vac IV® and Rabvac3® to its collection of leopard cats. Fel-O-Vac IV® was administered at 4, 7, 10, 13, 16 weeks, 1 year of age and every three years thereafter. Rabvac®- was given at 16 weeks, 1 year and every 3 years thereafter. Vaccine reactions were never encountered.
You can read other 2015 non-domestic feline vaccination suggestions here
Raccoons And Raccoon-like Animals (procyonids)
Canine Distemper (CDV)
Most, and most probably all, of this group of animals are susceptible to canine distemper. Once clinical signs appear, animals rarely if ever recover fully. Read more about canine distemper here.
So almost all facilities in the United States, did, until recently, vaccinate procyonids with Merial’s recombinant PUREVAX® FERRET vaccine (if they vaccinated them at all). If you read my preceding discussion on cat-like animals, you know that as of the fall of 2014, this vaccine is not available and it is uncertain when, or if, it will return to the market. (check link at top of page for possible options) Zoological veterinarians are in the process of pleading with Merial to resume production – even though the profits this vaccine generates for them probably does not justify its production. When PUREVAX® FERRET was available, many facilities gave yearly booster inoculations after a two-shot initial series at 8 and 12 weeks . An alternative to booster vaccinations was to do periodic blood antibody titer determinations. Any titre (≥1:16) is probably protective. (ref)
Killed distemper vaccines are no longer available in the United States or Europe. They do not reliably produce the antibody titer that living, attenuated (weakened=MLV=modified live virus) distemper vaccines do. We loved PUREVAX® FERRET Distemper vaccine because only a portion of the dog distemper virus was linked to a living canary pox virus that was harmless to mammals. With that currently unavailable, we only have less tested alternatives that lack the USDA stamp of approval. That doesn’t mean they are less safe. It just means that no scientific test on their use have been performed in procyonids.
My choice in raccoons would be Merial’s Recombitek C3 canine vaccine (rDACPP). It combines the same canary pox-vectored distemper virus that was in PUREVAX® FERRET with weakened (MLV) canine Adenovirus Type 2 and canine parvovirus. I feel most at ease with this vaccine because the same vaccine, (with additional MLV coronavirus and parainfluenza virus that procyonids are not known to need ) were extensively studies for their safety and effectiveness in raccoons by the staff of the Kentucky Wildlife Center. (ref)
Merck’s Nobivac Puppy-DPv, which has been an effective and safe distemper vaccine in ferrets with a multi-year track record in European ferrets, appears to be effective and safe in raccoons and skunks as well. Several rehabilitation centers in North Carolina use it in conjunction with Boehringer Ingelheim’s Fel-O-Vax PCT . But I am not aware that trials as extensive as the ones performed on Recombitek C3-4 have been run. Like Recombitek C3, Nobivac Puppy contains a modified live canine distemper virus but it is the whole virus, not just a portion as in the Merial/Boehringer Ingelheim ‘s ferret vaccine.
No vaccine will protect an animal that already has the wild distemper virus in its system. Vaccines given to immature, stressed, ill or injured animals are less likely to protect. Two vaccinations at 2-3 week intervals give more assurance than one.
As for other procyonids, if anyone has used those products, or others currently available, I am unaware of it. Please let me know if you do. ![]()
Parvovirus Disease (aka panleukopenia, canine parvo virus disease, raccoon parvo virus, mink enteritis virus)
Animal parvovirus are highly adaptable and capable from jumping from species to species. A raccoon variant is now common in the United States and Canada. Scientists believe that in recent times, the initial carnivore parvovirus was the one affecting cats (aka panleukopenia). (ref) By 1947, It had become a problem in ranched mink (MEV). By 1978 it had jumped to dogs (ref) [some disagree with this narrative (ref)]. Around 1980, it became a noticeable problem in raccoons (ref) Generally, it is human actions that allow these new viral threats to emerge. With suburban sprawl, urban and suburban raccoon numbers exploded as the clever animals became scavengers of pet food and human garbage. Intermingling of dogs cats and the growing number of raccoons made conditions ripe for a new parvo virus host to emerge (ref) [a perfect storm for serial viral passage and ramping up the virus’s pathogenicity/severity in a new host] (ref)
The parvo virus jumps back and forth between species – forever recombining and forming new variations. (ref) All it seems to require to mutate is a large group of susceptible carnivores housed near a carrier animal of another species or housed in facilities that previously housed one. The only blessing is that vaccines that protect against one carnivore parvo strain seem to be moderately effective in protecting against the others. (ref1 ref2 ref3 ref4) Vaccines produced against a parvo virus isolated from the same species can be somewhat more effective in stimulating immunity in that species. But in the case of procyonids, we do not have such a vaccine. Multiple vaccinations at 2 wk intervals often over ride that problem.
There is no evidence that raccoons are more protected against the raccoon parvo strain when they receive a cat parvovirus vaccine than a dog parvovirus vaccine. Perhaps procyonids receiving both the cat strain of parvovirus present in Zoetis’ Fel-O-Vax PCT or Merial’s PUREVAX® FELINE 4 and the dog strain present in Merial’s RECOMBITEK® C3 or Merck’s Nobivac Puppy-DPv have increases protection; perhaps it is just that a second vaccination of either boosts their immunity. In Florida and North Carolina, Merial’s RECOMBITEK® C3 and Nobivac Puppy-DPV (both containing the dog variant of parvovirus) have been given to Coatimundis as well as raccoons without noticeable side effects.
If you choose to administer a cat panleukopenia vaccine to procyonids, I would still go with Zoetis’Fel-O-Vax 3 because it is a killed (inactivated) product with a long, comfortable history of safe use in exotic species. However, killed vaccines of that type often produce shorter lived immunity than live (MLV) products. So, alternatively, if you are comfortable using MLV vaccines off-label, I would go with Merial/Boeringer Ingelheim’s PUREVAX® FELINE 4 , based on its successful use in raccoons at the Kentucky Wildlife Center and in pet coatimundis in Florida.
I would not administer dog and cat vaccines at the same time and I would not be confident that animals vaccinated at under 16 weeks of age would necessarily be protected. I would give the first vaccination at 12 weeks, second at 14 weeks and a third at 16 weeks – beginning earlier during an outbreak or if the animals were in an environment with a high likely of exposed to the virus.
Vaccination procedures are scientifically studied in dogs and cats and well funded. They are approved by the US Department of Agriculture, and printed on the label. Veterinarians using those products off–label in other species are relying on word of mouth reports – a case here and there – and an occasional a small public report. Even modified live vaccines sometimes fail. (ref) , particularly when the animals vaccinated are less than 16-18 weeks old or under stress.
Yearly revaccination is probably unnecessary when a juvenile parvo/distemper -containing vaccine series has been administered or a two-shot series has been given to adults, but yearly revaccination is often the practiced in captive animals. I generally suggest that animals be boosted one year from their initial series just to be cautious – vaccines given to juveniles can fail due to residual parental antibodies, inadequate vaccine storage or administration, illness or stress when given, etc. But post-vaccination immunity to those virus last at least 4 years in dogs and probably much longer. ( read here & here) Post-vaccination immunity to parvovirus in cats last at least 4 years (ref), 7yrs in another study (ref) and is probably lifelong. Periodic blood titer determinations can be reassuring, but low-titer and no-titer animals may still be adequately protected against clinical disease. (ref) because much of the animal’s immunity is based on long-lived memory defense cells, not antibody. (ref)
Over 95% of the procyonids vaccinated against parvovirus are orphan and injured raccoons in small rehabilitation facilities scattered across America.
Do not assume too quickly that an MLV (=attenuated or modified live virus) vaccine caused your raccoon(s) to develop parvo. There are many non-parvo causes of severe diarrhea in raccoons. Your orphaned raccoons could also have been incubating parvovirus before they receive their vaccinations, too young when vaccinated (ref) or were exposed to the virus before vaccinations had time enough to protect. The parvoviruses are one of the most resistant virus know. Their tough shell or capsid makes them very stable in the environment. (ref) In those cases, or when the animals are severely stressed, vaccines sometimes fail to protect.
Rabies
Many procyonid animals are kept as pets or as interactive display animals at institutions. The most common are raccoons, coatis and kinkajous. Very few kinkajous in private hands receive vaccinations of any kind.
Most zoos vaccinate their animal handlers against rabies, not their animals. But in display situations where the public is at risk of being bitten, the rabies vaccines of choice is Merial’s IMRAB®3 or 1 (aka RABISIN® in Europe) or Boehringer Ingelheim’s Rabvac-3. Given annually. This is not an approved use for either vaccine. Public health authorities investigating a human bite occurrence will still probably demand that the animal be killed and it’s head tested for rabies virus. Neither of these vaccines will cause rabies. But there have been instances where animal already incubating rabies received vaccinations and later developed the disease. The stress of capture and shipping were probably responsible for vaccine failures in others. (ref) A 21 day post-vaccination blood antibody titer and periodic blood titers over the years are the only sure way to verify protection. Even then, there is no agreement as to the minimum titer for protection.( read here![]() ) Read more about rabies here.
) Read more about rabies here.
Leptospirosis
All procyonids are susceptible to leptospirosis and dog and livestock formulations of killed leptospirosis vaccines are available. A 1997 AAZA guideline (ref) mentions the option of vaccinating procyonids against leptospirosis “if local geographic or zoonotic conditions dictate” but I do not believe that is frequently , if ever, done. Leptospirosis vaccines cause a high number of undesirable side effects in domestic pets and livestock (ref) I do not suggest their use in captive procyonids or other small non-domestic mammals. Read more about leptospirosis here.
Weasel-like Animals (mustela)
Domestic and wild ferrets are also members of the weasel family; but the two critters to the far right are not.
All mustela are believed to be susceptible to the same diseases. Their varied natural lifestyles make the likelihood of those diseases vary between species.
Due to the popularity of pet ferrets as well as the growing number of pet skunks, veterinarians have considerable data on which to base their vaccine programs within that group. The fur mink industry gives us another detailed look at the disease susceptibility of mustela.
Canine Distemper CDV
All mustela are highly susceptible to the distemper virus of dogs. The disease is frequently seen in American skunks and may circulate naturally in Canadian river otters and martins as well. Sea otters are also a host of the phocine distemper virus, a close cousin of dog distemper. Canine distemper outbreaks were a factor in the final disappearance of most wild populations of black-footed ferrets in the grasslands and prairies of central North America. Read more about canine distemper here.
Since 2001, the vaccine that veterinarians in zoological practice have relied upon to vaccinate all species of mustela is Merial/Boeringer Ingleheim’s PUREVAX® FERRET – a recombinant vaccine that links small portions of the distemper virus shell (the capsid) to a living canary pox virus. That vaccine became only intermittently available in 2013 and unavailable by mid 2014 with not date given for its return to the market place. (ref) If it returns, it is, by far, the safest vaccine currently available for use in all mustela species. Canine distemper virus, once killed, does not stimulate good immunity on its own. No commercial killed (inactivated) distemper vaccine is currently available. Some Mustela (domestic ferrets, skunks, mink, otters) react well to certain modified live virus (MLV) distemper-containing vaccines. In less common mustela species, we are less sure of vaccine safety.
During periods when Merial’s Purvac Ferret was not available, Merck’s Nobivac® Puppy DP (aka Progard Puppy) was probably the safest choice for use in mustela. It has been used successfully by ferret breeders in Europe since the 1990s . They did not have the option to switch to Merial’s PUREVAX® FERRET because the product violated the European Union’s ban on genetically altered organisms (GMOs). Nobivac Puppy DP has also been used successfully by skunk breeders and wildlife rescue centers in North America. The same viral strain used in Nobivac was formerly used in Schering-Plough’s Galaxy-D®. That strain of virus was successful in producing antibody titer in fishers, another mustela, while United Vaccine’s Fervac-D® was not (Fervac-D®, which is no longer marketed, is the same as their current mink vaccine,Distemink®). (ref)
Over the years, various studies indicate that it may be harder to produce adequate vaccine titers in mustela than in other species. That is why the virus mass of recombinant canary pox/distemper in Merial’s PUREVAX Ferret was three time the amount found in their other recombinant distemper vaccine, RECOMBITEK® C3, for dogs.
So up to three vaccinations, beginning at 8-12 weeks of age or two injections in unvaccinated adults, may be required to produce adequate antibody titers. Some also feel better titers are obtained when the vaccine is given intramuscularly rather than subcutaneously as suggested by the manufacturer. (ref)
During periods when Merial’s PUREVAX Ferret, was not available, other MLV canine vaccines that have been used in ferrets such as (Boehringer Ingelheim’s Duramune Max 5, Zoetis’ Vanguard Distemper measles, Merial’s Recombitec C3 & 4, etc.) have been used in mustella. None, to my knowledge, have caused illness. However, the vast majority of these ferrets were previously immunized against canine distemper. So residual antibody and cell-mediated immunity from previous vaccinations could, conceivably, mask ill effects one might see in ferrets that had not been vaccinated before. However, it is difficult to find a non-vaccinated ferret in the United States. The primary breeding facility, Marshall Farms, vaccinates all of them with MLV mink distemper vaccine (DISTEMINK ®) before they are sold.
If you opt to administer Merial/Boehringer Ingelheim ‘s Recombitec C3 because it contains the same pox-vectored distemper virus that is/was present in PUREVAX, remember that Recombitec C3 only contains 1/3 the recombinant virus that PUREVAX Ferret distemper vaccine did.
Parvoviruses
(Feline Distemper, Feline Infectious Enteritis, Feline Distemper, Feline Parvovirus Disease, Cat Plague, Dog Parvo Disease, Mink Enteritis ) Read more about parvovirus here. (Not a common problem in ferrets – yet )
The parvovirus of carnivores are constantly mutating and recombining with one another.
Many information sources suggest that mustela are susceptible to feline panleukopenia. (ref1 ref2 ref3) Basically, given the right circumstances, the parvovirus commonly found in one carnivore species has potential to affect other species.
Although I know of no confirmed cases of non-variant feline panleukopenia occurring in any mustela, the group is definitely susceptible to a closely related parvovirus, the cause of mink enteritis (it is not the same parvovirus as the one that causes Aleutian disease in mink). If you vaccinate your mustela adequately with a killed feline parvovirus vaccine, the same inactivated products (Zoetis’Fel-O-Vax 3) I suggested for felines or and procyonids, you will give them a measure of resistance against the mink enteritis parvovirus as well. (ref) So will all the commonly used MLV canine distemper/parvo vaccine combinations (Such as Nobivac Puppy) that practitioners are using in ferrets during the current PUREVAX Ferret vaccine unavailability. If, and when PUREVAX ferret distemper vaccine again becomes available, Fel-O-Vax would be my choice for parvovirus protection.
In Mustela as in procyonids, If you want to lower the risk of an MLV parvo vaccines even further, give Fel-O-Vax 12-14 days before the MLV so the animals already have a degree of parvo immunity. (ref)
Leptospirosis Lepto
Several information sources mention the desirability of vaccinating mustela against leptospirosis in certain situations. (ref1, ref2) Leptospirosis vaccines are the most reactogenic (likely to cause side effects) of all vaccines on the veterinary market. (ref) There might, perhaps, be situations where vaccination is warranted. That would probably be in mustela collections where confirmed cases of leptospirosis have occurred in the past and efforts to control exposure were unsuccessful. Habitat and exhibit modifications are a far better approach. Read more about leptospirosis here.
But in those situations, the Merck Nobivac® Lepto 4 vaccine would probably be my choice (ref) Even then, only four strains (serovars) of leptospirosis would be covered as the vaccines are serovar-specific (there are 250 known pathogenic serovars of leptospirosis). I would scale the dose to the body weight of the animal. ( read here ) When giving that vaccine, I would not combine it with any other because of the vaccine’s known ability to decrease the effectiveness of other vaccines given at the same time. ( read here ) Leptospirosis antigen-containing vaccines has been known to cause immune complex glomerulonephritis in dogs and similar effects have been suspected, but not proven, in mustela. (ref)
Rabies
All species of mustela are highly susceptible to rabies. Although I know of no studies performed, Merial’s IMRAB (RABISIN®) vaccine, approved for ferrets and other domestic species, should work as well in all mustela. I prefer IMRAB-3, a product sold by Merial in North and South America and the Caribbean. I do not know of its availability elsewhere. Follow up blood tests to insure sufficient antibody level was attained (≥0.5 IU/mL) is always prudent, but quite difficult to do in non-domestic mustela, as many, like otters, violently resist restraint. Rabies vaccination is governed by local laws. In some localities, one is not allowed to vaccinate non-domestic animals, in others, the law dictates that biting wild animals be euthanized and sent for analysis regardless of their vaccination status. Read more about rabies here.
The largest number of wild mustela and procyonids animals are vaccinated against rabies in wildlife relocation and rabies-control projects targeting skunks and raccoons (with Raboral V-RG® and ONRAB®). (see here![]() & read here ) Some of those vaccines are carried on (vectored by) a living raccoon pox virus. How that living pox virus might affect mustela and procyonids is uncertain; but those products do pose risks to those that administer them. (ref)
& read here ) Some of those vaccines are carried on (vectored by) a living raccoon pox virus. How that living pox virus might affect mustela and procyonids is uncertain; but those products do pose risks to those that administer them. (ref)
When one vaccinates animals recently obtained from the wild, one should not assume that all animals are then protected from developing rabies. Rabies can have long incubation periods in mustela, and some may have been exposed to the virus before the vaccine was given.
Bovine Tuberculosis
The mustelid most associated with tuberculosis is the European badger. It commonly harbors the cattle form of tuberculosis which is infectious to a number of other animal species as well as to you. Wild meerkats are also affected. (ref)
As an alternative to the wholesale extermination of badgers in the the United Kingdom, vaccination with BCG attenuated tuberculosis vaccine has been attempted. (ref1, ref2) Many believe that it is an exceptionally bad idea to use a vaccine of this type in any captive animal population because it never entirely removes this dangerous bacteria from the collection. Read more about bovine tuberculosis here.
Botulism
Botulism, a paralytic disease caused by a toxin (Clostridium botulinum type C toxin) released by the clostridium botulinum organism. It is a serious cause of mortality in the fur farm industry where it affects both mink and, to a lesser extent, foxes. (ref) The source of the disease is generally contaminated food or slaughterhouse waste fed to the animals. When it occurs in non-fur farming situations, the best solution is to locate a more hygienic source of your animal diets and remove water sources that may have been contaminated with large amounts of animal or plant debris. Read more about botulism here.
In the fur industry, anti-botulism protection is available in various combination vaccines (see section on mink below). Mink are generally immunized at 10 weeks of age. These vaccines are not always effective.
Domestic Ferrets
Due to the popularity of pet ferrets (also members of the mustela family) veterinarians have considerable data on which to base the vaccine programs for this animal within the mustela group.
The general vaccine choice to protect ferrets against canine distemper in North America has been Merial’s PUREVAX ferret recombinant distemper vaccine. In late 2014, with this vaccine unavailable, the world’s largest ferret breeder, Marshall Farms, recommends the off-label use of Nobivac Puppy DP. This is not a government-approved use of the vaccine. It is generally given subcutaneously. Nobivac Puppy DP has been in common use among ferret owners and breeders in Europe and the UK for many years because Merial/Boehringer Ingelheim ‘s, its maker, did not market PURVAX Ferret there.
There are few studies on how effective this off-label use of the vaccine is, but a single dose produced sufficient titers (protection) in 2 out of 5 ferrets vaccinated with a very similar Nobivac product (Nobivac DHP). Even giving eight times the suggested dog dose did not cause illness in the ferrets. (ref) Since not all ferrets are protected by a single dose, I suggest the vaccination at 12 and 14 and 21 weeks in animals that were never vaccinated previously (do whatever your veterinarian suggests). Because most if not all ferrets from large producers were vaccinated on the farm as kits, one inoculation in previously immunized ferrets is probably sufficient. Immature ferrets seem particularly difficult to immunize successfully with products like Nobivac. (ref) Distemper immunity, one obtained, is long–lasting. Allergic reactions are always a possibility. So vaccination at a veterinarian’s office, with epinephrine and oxygen close at hand, is always desirable.
Domestic ferrets may have their own genetic bottlenecks that make them more susceptible to vaccine reactions. When Gilman Marshall began the ferret industry in the United States in 1939, he did so to control rat infestation in the stored dent corn on neighboring farms. He started with only a few ferrets. By the 1960s when I was purchasing ferrets from his son, Gary, for NIH research, we preferred as little genetic diversity as possible. Animals, and humans, with little genetic diversity (highly inbred) seem to have more problems with vaccines. Perhaps he later increased his ferret gene pool with additional ferrets from Europe or the UK – I do not know.
Domestic ferrets also need the periodic rabies vaccinations (IMRAB®3) I discussed under Mustelas in general.
Influenza
Ferrets, and probably other members of the mustela family, are highly susceptible to the human, avian and swine strains of the influenza virus (flu). That is why they have been used for many years in influenza research. They filled that role among the scientific community long before they became common as pets. The H1N2 flu virus, a rather common one in pigs, is highly infectious to ferrets, killing them or making them severely ill. It is readily passed from one ferret to another as they sneeze. (ref) It is one of the “monster” (“tripple-reassortant”) flu virus that is part bird flu, part swine flu and part human flu – something similar to what the unrelated parvovirus I mentioned previously appears to be doing in carnivores. The 2011 version of Sanofi’s Fluzone human flu vaccine which is normally given by injection, protected ferrets from the flu when it was modified and given intranasally. (ref) Influenza can be particularly severe in old ferrets and those in poor health from other causes. I do not know of any veterinarians currently vaccinating pet ferrets against influenza. Read more about influenza here.
Black-Footed Ferrets
Black-footed ferrets are often used as the poster children for undesirable vaccine reactions. Most veterinarians acquainted with them, attribute that to their near extinction in the 1980s as the result of intensive farming, prairie dog extermination and successive outbreaks of canine distemper among their dwindling numbers. Only 18 ferrets, collected in 1985, formed the initial basis of controlled breeding programs. (ref) So their current gene pool is small. Small gene pools are associated with increased risk of vaccination reactions. (ref)
Although Merial’s PUREVAX Ferret is/was the obvious first choice to vaccinate them, the offspring of black-footed ferrets and European ferrets were thought to have been successfully vaccinated against canine distemper in 1988 with an MLV distemper vaccine before Merial’s vaccine became available. (ref) But by 2006, those researches had changed their mind and decided that none of the distemper MLV were safe in black-foots or their hybrid crosses with European ferrets. (ref)
Skunks
Skunks are susceptible to canine distemper. Until it became unavailable, I vaccinated my skunks with Merial’s PUREVAX Ferret distemper vaccine. I also vaccinated them with Merial’s IMRAB®3. Neither was a government-approved use of the vaccines.
IMRAB®3 is not approved for use in skunks, but it was found effective in one study. (ref)
With PUREVAX currently unavailable, many skunk breeders and skunk rehabilitators vaccinate their skunks against canine distemper with Merck’s Nobivac Puppy DP. Three vaccinations at two-week intervals , beginning at 8 weeks is prudent.
Again, that is not a government-approved use of the vaccine. It is approved only for dogs. I do not know of titers having been run to confirm that the vaccine is effective in skunks, but I know of no reports of side effects from its use in skunks.
Other skunk breeding facilities tell me they vaccinate their skunks with Pfizer’s Vanguard5+ (@ 5- weeks of age with a booster at 12 weeks). Others use Merial/Boehringer Ingelheim ‘s Recombitek C4 or Merial’s PUREVAX Feline 4.
Feline Panleukopenia In Skunks (aka Feline Distemper)
It is often written that skunks are susceptible to feline panleukopenia – a strain of parvovirus. I have never seen a case in a skunk nor do I know of a confirmed case. However skunks are definitely susceptible to at least certain strains of the parvovirus that circulate in wild carnivores and pets. ( rptref ) Read more about feline panleukopenia here
The vaccines I mentioned to immunize skunks against canine distemper (other than Merial’s PURVAX ferret) all contain dog parvovirus. All carnivore parvovirus are closely related. So administering one of those vaccines should afford skunks a measure of protection against parvovirus as well.
But veterinarian may choose to be extra cautious and vaccinate skunks for the feline strain of parvovirus as well. Both Boehringer Ingelheim’s Fel-O-Vax IV (an inactivated (killed) product) and Merial’s PUREVAX® FELINE 4 have been used successfully in skunks. I prefer using the inactivated product.
Otter Vaccination Protocols Around The World
Canine distemper occurs in captive and wild otters. Most zoos that vaccinated their otters used Merial’s PUREVAX Ferret distemper vaccine. The Dallas Zoo also vaccinates their river and short-claw otters yearly with Boehringer Ingelheim’s Fel-o-Vax PCT for parvovirus protection. The National Zoo in Washington, DC vaccinates all its otters against rabies every three years with IMRAB®3. It was vaccinating them against canine distemper every year with Merial’s PUREVAX ferret distemper vaccine.
European zoos did not have the option of using Merial’s PUREVAX ferret in their otters because the product was not sold there – at least not through 2009. For a time, they utilized a killed distemper vaccine produced in the Netherlands. It produced good antibody protection (ref) The Kristiansand Zoo in Norway sees no need to vaccinate their river otters, meerkats, or wolverines at this time. That is because canine distemper is rare in the country – there has never been a case of distemper at the zoo.
The Jerusalem Zoo was vaccinating all their middle eastern and Asian short-clawed otters, meerkats, beech and yellow throated marten and ferrets with Merial’s PUREVAX Ferret Distemper vaccine through 2014 when it became unavailable. The Monterrey Bay Aquarium finds no need to vaccinate the stranded sea otters that pass through their care. Nor do the staff of the Wildlife Treatment Center in Santa Cruz.
Although a case of West Nile fever recently occurred in a sea otter at the Pittsburgh Zoo and Aquarium, the threat appears to be isolated and the vaccine is not recommended at this time. You can read other 2015 mustella vaccination suggestions here
Meerkats and Mongoose
These smaller carnivorous animals, in the Herpestidae family, are not mustela. Some include them in their vaccine recommendations for viverrids, although they are not members of the Viverridae family either. Since both groups have the same vaccine requirements, it is of not of much concern to me where taxonomists place them.
Mongoose are susceptible to the feline panleukopenia parvo virus in at least some of its many variants. (ref) Although they are said to be susceptible to canine distemper (ref) , I know of no confirmed cases. Very little is know of the susceptibility of meerkats to viral infections. They are hardy animals and little has been written about their disease susceptibility other than to bovine tuberculosis. The latest zoo manuals recommend that they receive the same vaccinations as mustella. Of course, that was when Merial’s PUREVAX® FERRET vaccine was available. Some zoos still immunize both with Boehringer Ingelheim’s Fel-O-Vax for parvovirus/panleukopenia protection. How either of them might react to a modified live virus distemper vaccines I do not know.
Wild mongoose are also said to be frequent carriers of leptospirosis, however the most frequent strain of leptospira carried by mongoose in southern Africa is not be one of the strains (serovars) that canine or livestock leptospirosis vaccines are designed to protect against. (ref)
They are also said to be susceptible to hepatitis E. (ref)
I do not believe that many zoos in the world vaccinate their mongoose or meerkats. I know The Copenhagen Zoo does not find it necessary nor do the French Zoos. However, The SanWild Wildlife Sanctuary in South Africa does vaccine all the rehabilitation mongoose and meerkats they receive against rabies with RABISIN® (aka IMRAB) before they release them.
The vets at the exotic animal section of the veterinary school in Onderstepoort South Africa vaccinate the meerkats and ferrets that they see with a killed canine distemper vaccine that is locally produced. (Design Biologix).
Mink
Most of the 50 million+ ranched mink in the Western world are vaccinated against canine distemper, the parvovirus adapted to mink (Mink enteritis/MEV) and botulism at 10 weeks of age and then yearly. The vaccine has also been used successfully off-label in martins, raccoon dogs, silver and blue fox and domestic ferrets. I know of dogs having receive the vaccine as well with out apparent side effects. It is only sold in bulk 250 and 500 ml containers. It is quite effective. The distemper portion is modified live virus (MLV) of the Lederle , avianized canine distemper strain (Distemink®, Biovac®-D, Biocom®-D). The same formula in Distemink®, was once sold for ferrets as Fervac-D. When I used that product in domestic ferrets, I saw an unacceptably high incidence of post-vaccination anaphylaxis. All responded to epinephrine and oxygen therapy but I ceased using it.
There is no government-approved, individually packaged, mink vaccine currently available in North America. But I was told that a distemper vaccine approved for dogs and manufactured by a small vaccine producer in Tennessee was successfully used to vaccinate 9,000 mink and 100 ferrets. This is a modified live virus vaccine prepared from the Rockport strain of canine distemper. Long ago, there was a reported case of that particular strain not being safe in red pandas and it has been repeated over the years. Red pandas are notorious for their bad reactions to vaccines – perhaps the report was true. With no scientific studies to go on, zoo vets are quick to avoid a vaccine on the basis of a single, poorly documented report – they have no other choice.
Civet-like Animals (viverrids)
Like everything else from Madagascar, the fossa in the upper right corner of the photo is a unique snapshot into an ancient times. It is a Euplerid, not a Viverrid, but it is similar to civets in many respects – including its veterinary needs.
Viverrids are a group of small to medium sized animals found primarily in tropical areas of the Old World. How they relate to felines, canines and the other groups I previously discussed, remains a matter of debate. However, they share enough genetic characteristics with them to be susceptible to the same diseases and to be vaccinated under the same protocols. I would use the ones I suggested for procyonids.
Where a group of animals sits in the carnivore family tree often influences the diseases it is susceptible to. There is considerable debate about where viverrids belong. We used to think that they descend from an ancient extinct species (miacids) that split, about 50 million years ago into what became felines and hyenas while others went on to become the other species I discussed. That is now uncertain.
Civets
In America, a “civet cat” is a skunk, generally a spotted skunk, and no close relation of any actual civet and, most certainly, not a cat.
There are several species of civets; they are native to most of Africa, the Spanish peninsula, southern China, and Southeast Asia. They have been introduced elsewhere. If you live in America, their personality and feeding habits could be compared to raccoons and opossums – not as clever as a raccoons, not as obtuse as an opossum – willing to accept most anything digestible as a food source.
We know most about the disease susceptibility of Asian palm civets. That is because they are the most common of all the Viverridae and the most closely observed. They are also the civet most likely to be exposed to viral diseases because they are often trapped and brought into the environment of dogs and cats. They were farmed intensively for meat in various locations in Asia and are kept confined to cages in the production of Kopi Luwak coffee. In some areas of Asia, they are considered an urban pest. They were farmed in battery cages in China for the exotic meat market until the practice was banned in 2003 – although some black market farming continues. In other locations in Asia, the practice continues.
Canine Distemper CDV
Traditionally, zoos believed that civets, like mongoose, might react badly to modified live virus (MLV) distemper vaccines. (ref)
Two brands of MLV vaccine that are no longer produced (Galaxy&FrommD strains) appeared safe to give annually. (ref) The Galaxy name is now associated with Merck’s Nobivac line of vaccines. Whether Nobivac® Puppy-DPv, which also contains a MLV dog parvovirus strain is safe to use in Viverridae remains unknown. The Onderstepoort strain of canine distemper it contains is a slightly different avianized strain of distemper virus from the one than was present in Galaxy and Fromm. (although Nobivac® Puppy-DPv so far appears to be safe in ferrets, raccoons and skunks). Read more about canine distemper here.
The few zoos in America that house and vaccinated civets in recent years, used Merial’s Purevax Ferret vaccine, those in Europe, an ISCOM vaccine produced experimentally in the Netherlands at Erasmus Medical Center and provided pro bono by Intervet (now Merck). None of the private civet breeders in the US that I know of vaccinate their animals.
Although most cases are reported in palm civets, canine distemper has occurred in zoo binturongs and genets as well. (ref) When CDV occurs in Viverridae, domestic dogs (generally stray and village dogs) are usually the source of infection. In zoo and breeder settings, raccoons could be as well.
Civets ill with canine distemper show many of the signs seen in dogs – vomiting, enteritis diarrhea, dehydration and depression, nasal and ocular discharges, secondary bacterial pneumonia, occasional pustules on their abdomen and inner thighs, encephalitis and convulsions. Even the telltale thickening of foot pads seen in recovering dogs has been reported. (ref1, ref2)
Civets were farmed in China for the exotic meat trade. That was officially banned in 2003 because of fear of SARS. But they are still farmed in crowded quarters and mixed with populations of unvaccinated dogs in other areas of Asia. In 2011, a canine distemper outbreak wiped out the civets at one farm in Thailand. ( rptref ) These civet farms supply the Kopi Luwak coffee trade.
Feline Panleukopenia Feline Parvovirus, Feline Distemper (FPV)
Viverridae are also susceptible to infection with carnivore parvoviruses. There have been recent (2014) documented cases of the feline variant, panleukopenia killing civet farms in Thailand, and in one recent-imported civet in Hungary. (ref) Older zoo guidelines recommend annual vaccination against it using killed (inactivated) vaccines. ( rptref ) Read more about panleukopenia here.
Although the cat form of parvovirus disease, panleukopenia is the only form I know of that has been reported to occur in Viverridae, I would be surprised if they were not susceptible to the dog and raccoon-adapted forms, given the right circumstances. Perhaps it would be wise to vaccinate them against the dog forms as well, as is commonly done in raccoons and skunks, using Merial/Boehringer Ingelheim ‘s Recombitek 3 which has the same recombinant canarypox vectored distemper virus (at 1/3 the virus mass) as Purevax Ferret or Merck’s Nobivac® Puppy DP. I know of no one doing that nor could I guarantee it would be without risk; but with the speed and agility with which the carnivore parvovirus constantly mutate, it might be prudent. Something like that seems to already be happening (ref1, ref2)
Rabies
Civets are most likely susceptible to all variants of the rabies virus. In 2009, a new variant rabies virus was isolated from an African civet that had bitten a child in Tanzania. The civet apparently obtained the infection from a bat. (ref). Other reported cases of rabies in civets did not determine which strain of rabies was involved. Read more about rabies here.
Vaccination of civets and other Viverridae with currently available inactivated (killed) rabies vaccine is probably effective against this variant, but unproven. (ref) I do not believe that anyone would or should trust a vaccinated viverrid animal more than a non-vaccinated animal in a case of a human bite exposure.
Influenza
Civets are also susceptible to – and perhaps a reservoir of avian influenza (Bird flu). (ref) Read more about influenza here.
SARS Corona Virus
SARS virus causes a disease with symptoms similar to influenza in humans – although the virus are not related. It has killed almost one out of ten people it infected in prior outbreaks in Asia. Civet farming in China was ended in 2003 because of suspicion that civets might play a part in transmission of SARS. The suspicion was that the virus moves from its permanent reservoir in bats, first to civets and then to humans. What signs, if any, the virus causes in civets is unknown. (ref1, ref2) Read more about SARS here.
It is unknown if corona virus containing vaccines designed for dogs, but administered to civets, would have any protective effect. In the lab, there is some cross reactivity (cross protection) between swine coronavirus antibody (TGEV) and SARS, but only weakly between canine coronavirus and SARS coronavirus. (ref)
Some Vaccination Protocols Used Around The World In Viverrids
The National Zoo, Washington, DC suggests that all Viverridae, when in their collection, be vaccinated with Imrab 3 rabies vaccine every three year. They also suggest that they receive a yearly vaccination against feline panleukopenia with Fel-O-Vax. When Merial’s Purevax Ferret Distemper vaccine was available, they suggested that as well.
The Royal Artis Zoo in Amsterdam was , for a time, vaccinating their civets with a killed
ISCOM-adjuvanted vaccine provided as a public service by Intervet (Now Merck). Supplies of that vaccine are now exhausted. Most European zoos, including Twycross, do not vaccinate civet or other viverrids.
Bears (ursids)
Some American black bears are brown.
Bears are the most disease-resistant carnivorous mammals I know of – both in their native wild habitats and in captivity. They are armored with an exceptionally robust immune system that protects them from most infectious challenges. As such, they are rarely vaccinated by veterinarians in zoological practice. Some attribute the bear’s resistance to having evolved as scavengers – more likely to encounter disease organisms than more active predators. Others attribute it to their solitary nature and sparse distribution over large areas that limit bear-to-bear disease transmission.
Bears do encounter various disease organisms in the wild and in zoo environments. None are specific to bears. Antibody evidence of prior exposure to various strains of distemper (morbilliviruses) virus, adenovirus, coronavirus, parvovirus, herpesvirus, calicivirus, West Nile virus, avian influenza, Eastern & Western Equine Encephalitis and orbivirus have all been reported in bear. (ref) But although these virus replicate in the bears for a short time after exposure, it is exceedingly rare for any of them to produce visible signs of disease.
To date, none have occurred commonly enough to warrant preventative vaccination programs in zoos or animal collections.
American brown bears (grizzly bears) are a species noted for their tough constitutions. Of the 125 grizzly bears that are known to have died between 2011 and 2013 in the Yellowstone Park area, no deaths were attributable to disease. Another study of black bear mortality in the United States southwest also found that no bear mortalities were due to infectious disease. The only illnesses I have personally encountered in captive bears were due to underlying malnutrition. When performing bears are kept humanely, they rarely become ill. The largest Florida bear compound of this type has been in operation for 88 years (Grizzly, Syrian and European brown bears). During that time, no animals have shown signs of infectious disease and no vaccinations have ever been given.
Canine Distemper CDV
Fatal cases of canine distemper do occur from time to time in bears. (rpt ref) When it has occurred it has generally been in an immature individual under stress. Several studies have found that the vast majority of bears are exposed to this virus without developing overt disease (subclinical exposures). Blood samples from polar bears in Norway and on the pack ice of the Barents Sea during the 1990s found that 8% of the bears had been exposed to canine or phocine (seal) distemper. Other studies found the exposure of polar bears off Alaska was quite substantial. (ref1, rpt ref2, ref3) The first case of active canine distemper I know of was reported in a wild Pennsylvania black bear in 2013. (ref) Read more about canine distemper here.
Finding anti-distemper antibodies that tell of prior exposure is not the same as finding actual evidence that the bears were susceptible to canine distemper illness. Considering a bear’s carcass-scavenging nature and the intermingling of stray dogs (or sick raccoons) and wild bears, more cases would have been reported by now if this virus was a current, serious threat. But situations are never static;
Many zoos in the United States now face great challenges in infectious disease control due to the increasing power of animal activists who encourage animal feeding stations in the wooded parks that surround the zoological facilities. This greatly increases the opportunities for cross-species infections of the zoo animals. (ref1, ref2, ref3, ref4)
Raccoons have become a common vector of canine distemper virus in the United States. In 2011, the first case of canine distemper was documented in a black bear in southwestern Pennsylvania. We do not know if that will remain an isolated event or if it signals an eminent sea shift in canine distemper disease dynamics. In 2014, a survey of black bears in Maryland found that 25 out of 82 bears had been exposed to canine distemper (as evidenced by antibodies against the virus). (ref)
If bears were to be vaccinated against canine distemper , the safest vaccine to use would have been Merial’s PUREVAX canary pox-vectored Ferret Distemper vaccine, which was found to be safe and satisfactory in Giant pandas. (ref) However, several doses might be required. When seals were immunized with this vaccine, two doses were required at a 2-month interval to produce persistent immune titers. (ref) With PUREVAX current unavailability, veterinarians do not have a tested, product to fall-back upon.
Since ferrets and other mustela appear to be considerably more sensitive to distemper than bears, perhaps one of the MLV vaccines that appear to be working well in ferrets would be a good choice in a small trial study. Such a study is unlikely to occur unless there becomes a pressing need to vaccinate bears against CDV in the future.
Rabies
From time to time, a rabid bear will appear in the wild. It is often during periods when the disease is on the upswing in the dogs, mustela or viverrids of the same area. (ref1. ref2) Read more about rabies here.
Occasional zoos in the United States vaccinate their bears against rabies. In some cases it is more to reassure the public and staff than to address a likely threat; in others, such as the National Zoo, rabies exposure of their collections is a very credible threat. (ref) The USGS Inter-agency Grizzly Bear Study Team does not have a single documented case of rabies-associated mortality in a wild bear since the project began in 1973. But when bears in zoological parks are exposed to wandering raccoons, skunks or the possibility of rabid colony bats in the area, immunizing them against rabies might be justified. The AAZA polar bear study group suggest a double dose of 2 ml administered at or after the age of 16 weeks, then at 12 months and from then on yearly or every 3 years. ( rptref) My choice would be Merial’s, tried and true, IMRAB®3 (aka Rabisin).
A 2014 study found 4 out of 77 black bears in Maryland had antibody titers against rabies. it is unclear if these were bears that naturally overcame rabies virus exposure or bears that had consumed Raboral V-RG® baits targeted at fox and raccoons in one of the mid-atlantic state wildlife vaccination campaigns. ( rptref)
Canine Adenovirus-1 CAV-1
Blood collected from wild and captive bears consistently show that a number have been exposed to canine adenovirus-1, the cause of infectious hepatitis of dogs and/or transient respiratory inflammations. At least one study attributed active hepatitis in a black bear to this virus, but most infections are probably sub-clinical (as they generally are in dogs as well). The closer bear populations are to feral or unvaccinated dogs, the more likely they are to have evidence of exposure to this virus. (ref1, rpt ref2) When bear populations exceed the natural carrying capacity of an area or when bears are overcrowded in display environments, the chances of canine Adeno1-related diseases are thought to be more likely. (ref) Read more about canine adenovirus-1 here
To my knowledge, no killed, inactivated canine adenovirus vaccines are currently available. If one should elected to vaccinate bears against Adeno-1 virus, the safest vaccine would probably be the intra-nasally administered adenovirus-2/Bordatella vaccine produced by Merck (Nobivac® Intra-Trac®3 ADT), which utilizes attenuated (MLV) canine Adenovirus-2, known (in a different brand) to cross-protect dogs against canine adenovirus-1. (ref)
Feline Panleukopenia and assorted Carnivore Parvoviruses
The parvoviruses of carnivores are forever mutating, recombining and forming new strains. Under the right conditions, all have the potential to cross species lines. (ref1, ref2) Read more about feline panleukopenia virus here.
I do not know of any reports of disease caused by canine parvovirus in bears. But the virus is known to circulate in both wild and captive bears in southern Europe (ref) , another study found evidence that both wild bears and captive bears in Croatia have been exposed to the canine form of the virus (CPV-2). The same AAZA guidelines for polar bears mentioned earlier suggest that polar bears be vaccinated against it . Should that be done, my choice vaccine would, be Fel-O-Vax®3 because of its inactivated ingredients. I would probably double the volume of the dose given to adult bears, similarly as is suggested by the zoo study group for rabies vaccination, to compensate for the bear’s great weight. Many believe that there is a degree of cross protection afforded by a vaccine directed against one species-adapted carnivore parvovirus against others. But in raccoons, many vaccinate them with a dog parvovirus strain as well as a feline one hoping for better protection across the various carnivore parvovirus variants (strains).
Equine herpes virus /= myeloencephalopathy EHV
The veterinarian at Chicago’s Lincoln Park Zoo brought this virus to my attention as a potential threat to bears. The EHV viruses are generally associated with horses and horse-like animals such as zebras. They usually only cause mild respiratory tract illness in those species. When the virus jumps to gazelles and giraffe kept in close proximity to equids, it has been known to cause fatal encephalitis. There are several of these herpes virus strains. EHV1/EHV9 will infect a very wide range of animals when given experimentally. (ref) In the last several years, we believe it was the caused fatal encephalitis in bears. (ref) EHV viruses are also present in wild herds of zebra in Africa. (ref) Read more about equine herpes virus here.
Although vaccines are available for several of the EHV strains that are common in horses, I know of no zoos using them in bears at this time. Instead, it has become common to maintain ample distance between exhibits of equid or artiodactyl (even toed) zoo species and bear exhibits, to be vigilant against cross-contamination and to service potential vectors last.
Brucellosis
Blood samples from bears in Europe and North America consistently find a small portion to have had contact with Brucella organisms, the cause of brucellosis. (ref1, rpt ref2, rpt ref3) I do not know of any reported cases of brucellosis-positive animals in zoological collections, and it remains unknown if any of the Brucella organisms are capable of causing illness in bears. Read more about brucellosis here.
Other than polar bears whose source of contact with the brucellosis organism is likely the consumption of brucellosis-positive seals; bears that are found to have been exposed to Brucella in the wild are thought to have been exposed through contact with native even-toed ungulates (cud-chewing ruminants) in their region – particularly through the consumption of placental tissue (afterbirth) and aborted fetuses. In grizzly bears found with positive Brucella antibody in Alaska, the source was thought to be caribou/reindeer, In Canada and Northern Europe, those species plus musk oxen. Most screening tests used in bears were for Brucella abortus. But an EAZWV publication lists the swine variant, Brucella suis as a threat to bears as well. (ref)
Black bears have been experimentally vaccinated against brucellosis as a prelude to the possible mass vaccination of Bison, in the Yellowstone National Park area with RB51 brucellosis vaccine. Unlike Bison given the vaccine, the bears did not seroconvert. (ref)
Tetanus
I do not know of any reported cases of tetanus in bears, wild or captive – but all mammals appear to be susceptible to tetanus to one degree or another so I suppose it could happen. Horses and other equines are the most susceptible. AAZA 2009 guidelines ( rptref) suggest that polar bears be vaccinated against tetanus. Double the standard 1ml dose is suggested. Some recommend revaccination every year, some every three years. The vaccine’s intended use is in horses where manufacturers (such as Merck) suggest a 1ml dose be given at 4 months of age or older and again 4-8 week later. That is followed by a booster at 12 months of age and boosters every 2 years thereafter. I know only of two zoos that administer tetanus immunizations to their bears, but there are probably others that do. Read more about tetanus here
West Nile Virus WNV
West Nile Fever is caused by an arbovirus (Flavivirus) passed by infected mosquitoes. It was thought to be an African and Middle Eastern problem until 1999 when it first appeared in the Queens Borough of New York City. Besides humans, various birds at the Bronx Zoo died in this initial outbreak. Since then it has spread across the United States. Its primary reservoir appears to be birds. An isolated case of West Nile Virus paralysis occurred in a polar bear housed at the Toronto Zoo in 2009. (ref) But otherwise, infection is only evident from animals having antibodies against WNV – evidence of a prior experience with the organism (seroconversion) that they overcame. The authors suggested that captive bears might need to be vaccinated against WNV. The virus apparently affects wild populations of bears in Croatia as well. (ref) Six out of 51 black bears trapped in New Jersey in 2002 had WNV antibodies denoting prior exposures. (ref1, ref2)
Veterinarians and physicians believe that West Nile virus causes no clinical signs in over 80% of the animals and humans that are exposed to it and only mild symptoms in most of the rest. Blood IgM antibody levels help diagnose a current infection while the presence of IgG antibodies signify a past infection and , probably, lifetime immunity. The dynamics of WNV changes from year to year and area to area. Migrating WNV-infected birds are thought to move the virus about.
Disease risk is in an ever-changing state of flux. Perhaps, under high-risk situations or in the midst of an outbreak, vaccination of zoo animals that are IgG negative might be warranted. No bear collections I am aware of currently do so. Several killed (inactivated) vaccines are available to protect horses against all three of the common causes of viral encephalitis (such as Merck’s Encevac®+ WNV or Merial/Boehringer Ingelheim ‘s RECOMBITEK® rWNV ). Their effectiveness in bears is unknown. You can read what is known of their use off-label in zoo species here. Read more about West Nile Virus here .
Calicivirus
The same Norwegian study that found evidence of exposure of polar bears to canine distemper also found antibodies attributed to calicivirus in 2% of the bears. The significance of that remains unknown. (rpt ref) Since seals are high on that bear’s menu, the calicivirus was most probably the same one occasionally found in seals and sea lions (San Miguel Sea Lion Virus, vesicular exanthema virus of swine). In seals, it is thought to usually be a mild, transient disease causing, at the most, transient (temporary) skin vesicles on the bottom of the flippers and at the margins of the mouth and anus (mucocutaneous junctions) – by 4 months of age, most California sea lions have been exposed to it. (ref) What, if any, lesions it causes in bears is unknown. It was last seen in swine in 1959 and is thought to not currently affect that species. I know of no vaccine that is available. Read more about calicivirus here.
Bluetongue virus /epizootic hemorrhagic disease virus EHDV
Some free-ranging Florida Black bears showed evidence of exposure to the bluetongue virus. (ref) Bluetongue disease is primarily a disease of domestic and wild ruminants. Tests to detect the antibodies produced by exposure can be confused by exposure to a similar orbivirus, epizootic hemorrhagic disease. (ref) That is a disease primarily seen in wild whitetail deer. Both are primarily passed animal-to-animal by biting insects; but there is some evidence the virus can be passed along by eating infected carcasses as well. (ref) That is thought to be a possibility in the Florida black bears. Inactivated livestock vaccines against this pathogen are available. I do not know of them ever having been administered to bears. Read more about bluetongue here.
Leptospirosis
Bears, like most mammals, are susceptible to leptospirosis when exposed to the organisms. There are over 250 pathogenic strains (serovars) and a vaccine intended for one is often inefficient in protecting against other serovars. Vaccines intended for use in dogs protect against four of the more common ones, those for cattle or pigs the same plus one additional serovar (Hardjo). Read more about leptospirosis here.
Some suggest the option of vaccinated bear against it yearly. Because the leptospirosis organism exists in many “strains” or serovars, one would have to take into account the serovars present in the area in choosing a vaccine. In a 2014 study, 14 out of 61 wild Maryland black bears had evidence of prior Leptospirosis exposure (2 to L. i. pomona, 3 to L. i. Icterohaemorrhagiae, 1 to L. canicola, 4 t o L. i. grippotyphosa and four to L. i. bratislava) some were positive for multiple serovars. ( rptref) As in most killed antigen vaccine products, the resistance (antibody titer) produced is often dependent on the dose volume (bigger animals require more). (ref) Leptospirosis products cause the greatest number of adverse reactions of all the veterinary vaccines, so increases in dose (antigen mass) need to be carefully thought out. In some species, vaccination against leptospirosis can cause false-positive reactions in diagnostic tests for other diseases, such as brucellosis. ( read here )
Most authorities believe that the vaccination of bears against lepto needs to be done only when it is a known problem within the animal collection as a whole. I do not know of anyone currently giving these vaccines to bears. Identifying the source of the organism and limiting exposure is a better approach.
Some Vaccination Protocols Used Around The World In Bears
Omaha’s Henry Doorley Zoo vaccinates its bears yearly against rabies and tetanus; The El Paso Zoo does as well.
The National Zoo in Washington DC vaccinates its bears every 3 years with Merial’s Imrab-3 ; Albuquerque’s BioPark Zoo vaccinates its bears against rabies as well.
Neither the Dallas, TX Zoo, Seattle Washington’s Woodland Park Zoo nor The Johannesburg Zoo find it necessary to vaccinate their bears.
Large compounds of stressed and injured Asiatic black bears are kept in rehabilitation centers in Viet Nam, Cambodia, Laos and China. None of the veterinarians associated with those facilities find it necessary to administer vaccines to their bears. They tell me that biosecurity and keeping their compounds and the surrounding vicinity free of wandering dogs and livestock has been sufficient to protect them from infectious disease.
Monkeys, Apes And Prosimians (primates)
Because of their similarity to us and their use in virus research; we know a great deal about the disease susceptibilities of primates.
The chief source of infectious disease in captivity are the people who come to view and care for them. The chief source of infectious disease in wild colonies near human habitation are indigenous people, their livestock and village dogs. Primate disease susceptibility and vaccination needs are varied. The less specialized prosimians primates, like the ring-tailed lemur in my illustration, might need only periodic rabies vaccinations (ref), while a vaccination program for chimpanzees or gorillas would minimally include measles, polio and tetanus and might include rubella, influenza and hepatitis vaccination as well. (ref)
Primates are not only vaccinated by us to protect them; they are also vaccinated to protect the people who care and associate with them. Even free-ranging monkeys that frequent tourist sites and temples are occasionally vaccinated for that purpose. Sometimes, it is more efficient to vaccinate the people who care for the monkeys than the monkeys and apes (Pongidae) themselves. (ref1, ref2)
Prosimians Lemurs, etc.
Prosimians are in the primate line of descent. But the group is more ancient than primates and does not possess many of the attributes and, apparently, does not share many of the diseases that primates are susceptible to. The most well known in the group are the lemurs.
Lemur breeders rarely immunize their animals. Several facilities, including the Bronx Zoo and the St. Catherine’s Island colonies they managed, vaccinate their lemurs against rabies. Those on the Georgia island also received periodic tetanus vaccinations. Zoo guideline do not contain specific immunization recommendations for prosimians. (ref) Those that are housed in situations where the public is at risk of bites are often immunized against rabies.
Marmosets Tamarins and Squirrel Monkeys
These smallest of primates rarely receive vaccinations. Both breeders in North America and Irish Zoos warn about the dangers of administering vaccines designed for humans or domestic animals, to these small creatures. (ref) The few I know that have experimented with vaccines in these primates (as well as squirrel monkeys) scaled the doses down to account for their small size, but most feel the risk of serious vaccine reactions greater than possible vaccine benefits.
Monkeys
Many zoos, and some research monkey colonies vaccinate their monkeys against Tetanus. Infants receive the vaccine at 6-12 months of age, then get a booster vaccination about a year later, then every 5-7 years. Two brands that I know are used are Zoetis’ Tetanus Toxoid/ Equivac® T and Colorado Serum Company’s Tetanus toxoid-unconcentrated. In facilities where primates are less likely to have ground contact, the practice is less likely. Tulane National Primate Research Center in Covington, LA utilizes Zoetis’ tetanus toxoid. Their standard dose for all monkeys is 0.5ml administered yearly. Yerkes does the same, but at a 10-year interval.
Many veterinarians feel that the use of human DPT vaccine is not the best way to obtain tetanus protection in monkeys. Too many adverse reactions are produced. ( rptref)
Monkeys housed in research colonies were often vaccinated against measles – generally at 6 month of age with titer determinations afterwards. Since human measles vaccine has become unavailable in the United States in 2009 (other than in combination vaccines), most veterinarians have gone over to using Zoetis’ Canine Distemper/Measles vaccine (Zoetis DM) to protect monkeys. Canine Distemper virus and measles virus (both morbilliviruses) are closely related with cross-protectivity. There has been great consolidation within the veterinary pharmaceutical industry. Products that generate only modest revenues, such as Distemper/measles vaccine are sometimes discontinued. But as of the fall of 2014 when I wrote this article, Zoetis tells me they will continue to produce it. The NIH rhesus monkey colony staff tell me that they have used the human MMR vaccine successfully in their rhesus and cynomologus monkeys, but I do not know of other facilities in the United States administering it to monkeys. The MLV (modified live virus) mumps and rubella virus it also contains are something most primate veterinarians shy away from. Some do so for fear of reactions, others because the monkeys are destined for vaccine or other research where positive mumps and rubella titer could influence results.
Some zoos, such as the Henry Doorley in Omaha , NE vaccinate their monkeys against rabies as well as tetanus. The National Zoo in Washington, DC does as well. Most private breeders of monkey in the United States do not administer vaccines to their monkeys.
Some of the South African zoos vaccine their monkeys against pseudotuberculosis and yersinia enterocolitica. The first disease is most often seen in squirrel and owl monkeys, the second as scattered cases among many primate species. Their vaccine is produced locally in Pretoria (Design Biologix). Colorado Serum Company produces a pseudotuberculosis vaccine. I do not know of it having been used in monkeys.
Vaccination of pregnant monkeys should always be avoided.
What Is A Proper Size Dose?
When a vaccine is used off-label in a monkey whose body weight is considerably less that that of the species for which it was intended, I usually decrease the dose volume proportionately. That is particularly true with killed antigen containing vaccines where the full antigen load necessary to stimulate immunity is contained in the vial of vaccine. Others, such as the California Regional Primate Center, take that approach as well. (ref)
Greater And Lesser Apes Gorillas, Orangutans, Chimpanzees and Gibbons
People that attempt to keep track of primate numbers (ISIS/360 and the IUCN), believe that there are about 875 gorillas housed in zoos as of 2015 and perhaps 95,000 left in the wild (although many of those may have recently been killed by the Ebola virus – there are mixed thoughts on that [ref]). Their records show 898 orangutan in zoos and, perhaps 50-60,000 in the wild. Bonobos in zoos account for about 200 individuals and it is thought that perhaps 30-50,000 remain in the wild. There are about 1,200 chimps in zoos and probably less than 200,000 in the wild. Siamangs and gibbons in zoos number just over 500 and, perhaps 50 to 60,000 remain in the wild.
These large primates appear to be more susceptible to a number of diseases than we rarely see in their smaller cousins. Their rarity and value in collections also influence the increased number of vaccinations they often receive. In general, zoos and animal collections in the United States administer considerably more vaccines to these animals than do zoos and facilities in the rest of the world.
When vaccines are give, the most common ones are vaccinations against tetanus, measles and polio (poliomyelitis ). (ref1 rptref2)
The Mesker Park Zoo, Evansville, IN, vaccinates their lesser and greater apes against tetanus and rabies; so does the Henry Doorley Zoo in Omaha, NE, the Detroit Zoo, the National Zoo in Washington, DC and many others. Tetanus boosters are given every 5-7 years, rabies every year or 3 years depending on brand of vaccine used.
The Detroit zoo, Zoo New England and other US facilities also vaccinate their gorillas against human influenza using the human quadrivalent brands (ref) optimized for that year’s flu season. Zoo New England also gives their juvenile gorillas the standard childhood MMR vaccinations.
Chimp Haven in Keithville, LA supports 204 chimpanzees. They vaccinate juveniles with MMR, polio, rabies and Diphtheria/Tetanus vaccine. Adults receive DTaP (diphtheria/tetanus/pertussis) and MMR boosters when the animals vaccine history is uncertain. When the Yerkes National Primate Center had chimps, they followed this same protocol. (Chimpanzees as research subjects are no longer tolerated in North America or Western Europe. As Ebola rages in Africa, that may prove to have been a short-sighted decision. Read one veterinarian’s lament here.)
The Melbourne zoo utilizes the ADT vaccine in their gorillas to immunize them against tetanus and diphtheria. They administer booster every 5 years. The Taronga Zoo in Sydney utilizes it a well in their gorillas, but also vaccinates their gorillas against the EMC virus due to previous mortalities.
Zoo Zürich vaccinates its great apes only against tetanus, the Hong Kong Zoo, and La Palmyre Zoo, Les Mathes, France, like many other European and Asian zoos, do not currently give vaccines to greater and lesser apes.
Specific Vaccines In Primates
Human Influenza Flu
As I mentioned, zoos generally reserve flu vaccinations for their great apes. When these animals develop influenza or other respiratory virus infections, they are highly susceptible to fatal secondary bacterial pneumonias. (ref) Although apes generally become infected from their caretakers, the virus can also move in the opposite direction. So everyone needs their flu shots. (ref) One needs to assume that just about every respiratory tract virus that affects humans has the potential to infect primates – sometimes with considerably more severe results. Read more about influenza here.
Diphtheria / Pertussis
Although some continue to administer DPT (aka DTP and DTwP) or DT (aka TD) to monkeys, most reserve them for the great apes. Many veterinarians, including myself, avoid administering them to smaller primates because of a high number of adverse reactions. Those reactions are often associated with the pertussis portion of the vaccine. If you elect to give them, it is probably safer to use a vaccine followed by the letter “a”(eg DTPa) than one followed by the letter “w” (eg DTPw) (ref) Those with lower case d and t are less likely to cause adverse reactions because they contain less antigen. But they are somewhat weaker in their ability to confer protection. Read more about diptheria/pertusis here.
Some veterinarians doubt that primates are highly susceptible to pertussis. In stressful, caged conditions they may be – particularly baboons. (ref)
Poliomyelitis Polio
Oral polio vaccines are generally reserved for great apes – although the infants of smaller primates can be experimentally infected. (ref1, ref2) The inactivated, injectable formulas rather than oral formulas, are the safest. (ref) A standard human dose is generally given at 3, 6, and 9 months and at 2 years of age. but vaccine instructions vary – follow the product insert that comes with the vaccine. (ref1, rptref2) The National Zoo, in Washington, DC vaccinate its great apes against polio. They administer 0.5 ml of inactivated human poliomyelitis vaccine IM when the primates are 2 month old and repeat with 2 additional boosters (the CDC advises these boosters be given at 4 months and 6-18 months of age). Read more about polio here.
Poliomyelitis is not only a threat to the great apes of zoological parks. In November-January of 1966, many of the chimpanzees of the Gombe Stream National Park in Tanzania developed polio. Six were were permanently disabled, six died. The epidemic, which was probably passed to them by their human neighbors, was finally halted by giving them oral polio vaccine hidden in bananas.
Measles
Measles can wreak havoc in primate colonies. We had several outbreaks in the rhesus monkeys I managed at the NIH. (ref) Most died of secondary bacterial pneumonia due to the immunosupression measles virus commonly causes. (ref) I used to immunize rhesus and cynomologus monkeys with the MMR vaccine produced by Merck which protected against Measles, Mumps and Rubella at 3-4 months of age, with a booster at one year of age (ref) using the standard human 0.5ml dose given SC. Most facilities that vaccinate now use Zoetis’ puppy Distemper/measles vaccine which appears to be less reactogenic (less bad reactions). Read more about measles here.
Measles causes more deaths in some primates than others (colobus, silver leaf monkeys and some new world monkeys seem to be particularly susceptible) (ref) Some revaccinate as frequently as annually depending on risk, experience in their specific collection of primates and the persistence of protective antibody in the animals as determined by serology. Young apes can still have levels of measles antibody at 1 year of age, passed on through the milk by immunized or recovered mothers. Those juvenile animals need their final vaccination at about 15 months of age.
Many veterinarians, myself included, hesitate to use modified live measles vaccine in very small monkeys, such as tamarins and marmosets. (ref) It can take up to 4 weeks for MMR vaccines to protect. In the midst of an epidemic in a primate colony, human gamma globulin injections may be a better alternative. (ref)
It is always wise to confirm that all of your staff have adequate measles antibody titers. Live attenuated measles-containing vaccine is immunosuppressive. I would not administer it at the same time other vaccines are given, or shortly before shipment or transfer.
Canine Distemper Expanding Its Range
Canine distemper virus and human measles virus are closely related morbillivirus. We used to believe that monkeys and apes were not susceptible to canine distemper. We now know that was wrong. As I mentioned earlier, there have been two major canine distemper outbreaks in monkey colonies, one in Japan and one in China. Primates vaccinated against human measles are probably considerably less likely to become clinically ill with canine distemper. (ref1, rptref2, rptref3, rptref4) Read more about distemper here.
Viral Hepatitis
An enormous amount of information exists on hepatitis in monkeys because they serve as the chief animal model for that disease in humans. There are five hepatitis virus that are of concern in primates. Each exists in many variations and more will probably be discovered. They are chiefly a concern in captive animals because of worries that they might be a source of infection to the people who care for the animals. The one of most concern in most collections is hepatitis B and many zoos vaccinate against it in infant great apes and gibbons when the animals are quite young (during the animals first few weeks) and follow with revaccination at 1 and 6 months of age. Glaxo Smith Kline’s recombinant hepatitis B vaccine has been used in Gibbons at the full 0.5 ml human dose. (ref) Many vaccinate the animal keepers as well. Gibbons, woolly monkeys and chimpanzees are often mentioned as most likely to carry hepatitis B virus (ref); but as time goes by, more and more monkey species have been found to be positive for one or another of the many hepatitis B strains. In most cases, the virus do not appear to cause disease in the primates – particularly when the strain is associated with the species in question. As of 2014, various hepatitis B virus strains had been isolated from orangutans, a captive land gorilla (ref), free-ranging rhesus monkeys in Florida, woolly monkeys (ref) African green monkeys etc.
Yet, the potential of these hepatitis virus to cause disease in primates or to infect their keepers remains unclear. There was a time when veterinarians believed that primates that harbored or showed evidence of prior hepatitis exposure had become infected from their human handlers. Although that no doubt could occur, it now appears that one form or another of hepatitis virus circulate naturally in wild primates – at least the larger ones. (ref) Whether that is a hazard to the monkeys or the people who come in contact with them remains to be seen. For instance, although wild gibbons and orangutans are reported to have a 22-33% and a 15% incidence of antibody to hepatitis B, it was reported that none were symptomatic (ill) nor was there a record of a human having been infected with hepatitis B through contact with them . (ref1 ref2)
Between 2004-2006, hepatitis E virus was detected in outdoor breeding colonies of monkey in Japan, perhaps due to close contact with feral swine which carry their own strain of hepatitis E. No mention was made of the virus causing illness in the primates. (ref) Chimpanzees are apparently also susceptible to infection with the virus as well (ref)
Hepatitis A apparently also circulates in wild monkeys. (ref) There are reports of a hepatitis A strain causing illness in cynomologus and African green monkeys (ref1, ref2)
Chimpanzees are known to be susceptible to hepatitis C – at least under experimental conditions (ref)
There was also a time when some authorities warned that vaccinating primates against hepatitis was a bad idea because it would make them show positive on future blood tests. (rptref) But with the availability of PCR tests that look for the actual virus rather than antibodies against it, that is no longer a valid concern. (ref)
Another problem with using hepatitis blood antibody titer tests as a way of judging the effectiveness or need for revaccination your primates is that immunity to infection can last considerably longer than antibody can be detected in their blood. That is because cell-mediated immunity is thought to be a large factor in immunity to hepatitis B. (ref1, ref2)
If I vaccinate my primates with standard human hepatitis B vaccines, will they be protected against other hepatitis virus ?
The monkeys will probably derive some resistance to all hepatitis B strains – although that is not firmly established. If they do become infected with a variant strain, they may shed the virus for a time, but should not become ill. (ref)
They will not be protected against Hepatitis A or C. Separate human vaccines against hepatitis A exit – one was used successfully in rhesus monkeys. (ref) I do not know if they have been used in primates.
There is no vaccine currently available for hepatitis C. (ref)
EMCV
A picornavirus, encephalomyocarditis virus (EMCV ) occasionally causes sudden death in primates. You read about EMCV most frequently when elephants are lost to it, but it occasionally affects primates and many other species as well. (ref) We understand very little about its epidemiology in zoo animals – why it passes through most with no apparent illness, while at other times mortality occurs. Perhaps some strains of the virus are more pathogenic than others. (ref1, ref2) It is indistinguishable from its close relative, the Mengo virus. Rats are a natural carrier and reservoir of this virus (ref), although other rodents also have that potential. (ref) Stray cats can carry it as well. (ref) It does not appear to affect them, but when it jumps to domestic pigs, as it commonly does, swine can develop fatal heart inflammation or abort their offspring. Although the EMC virus’ potential to cause serious disease in humans is debatable, in one study veterinarians who tend to swine had a 27-47% serological evidence of exposure to EMCV. (ref) Cases tend to occur in warm climates during the fall and winter. In 2009, many cases occurred at the Tacugama Chimpanzee Sanctuary in Sierra Leone and a fatal outbreak occurred in a chimps and other zoo animals at the Taronga Zoo in Australia. (ref) The Australians produced a vaccine and provided some of it to help out the folks at Tacugama. But losses occur now and then in zoos throughout the world. A vaccine is intermittently available. You can attempt to find it by Inquiring of the AAZA Elephant Study Group , the EAZA or the Pirbright Institute to find a vaccine source. Read more about EMCV here.
Large Cow-like Wild Animals (bovids)
The number of American bison housed in zoos around the world is estimated by Species360 to be about 1000 individuals. The IUCN and others estimates those in the wild and on ranches number 200-300,000. European bison in zoos account for approximately 1,400 animals. Those reintroduced to the wild, close to 3,000 individuals. The wild population of Gaur is estimated to be 13,000-30,000; those in captivity about 155. The world zoo population of Banteng number about 218 individuals; with 5-8,000 remaining in the wild. Lowland anoas in zoos number about 100 while the reported number of mountain anoas in zoos is only 3. The combined population of anoas in the wild is probably less than 7,000.
The vaccination needs of wild bovine animals are quite similar to the vaccination needs of agricultural cattle, sheep and goats that live in their immediate vicinity. When housed in zoos that are physically isolated from such areas, their vaccination needs can be minimal. (ref) When they are mixed with the general population of cattle, such as may occur in water buffalo dairies and farm-raised bison, their vaccination needs are quite similar to cattle. However, their ability to tolerate the effects of modified live virus vaccines can be less than that of domesticated ruminants.
Of all the wild bovids, veterinarians know the most about American Bison because they are extensively ranched in North America. Bison herds have demonstrated their susceptibility to not only cattle diseases but also to cross-over diseases of sheep and goats. Although Bison numbers were reduced from 30-60 million to less than 1000 in the 1800s in North America, they seem to have preserved a hearty disease resistance.
In contrast to American Bison, European bison appear to have high disease susceptibility. That has been attributed to bottlenecks in their genetic makeup (inbreeding). They were hunted to near extinction (by the 1920s only 54 closely related animals remained) before their populations increased in European zoos and reserves. Foot and Mouth disease and bluetongue mortalities have plagued them at various times in the few reintroduced wild groups that remain.
Gaur are also reported to be at increased risk of certain clostridial infections and foot and mouth disease – something also blamed on inbreeding.
Water buffalo have a reputation for high disease resistance. In areas where they are common, they tend to have less infectious disease problems than the cattle that surround them. The most common problem among them in those areas is pasteurellosis (Pasteurella multocida) They also appear to be more resistant to Foot and Mouth disease than cattle. (and to contagious bovine pleuropneumonia = Mycoplasma mycoides). Some US veterinarians administer the same innactivated (killed) vaccinations to Yak as they do to cattle. Yak are also susceptible to EHD/BTV for which vaccines exist. (ref) (Read about EHD/BTV under the deer heading.)
Banteng are also known for high resistance to cattle diseases. In zoo situations and when housed with cattle and sheep, blackleg (Clostridium chauvei) and BVD have caused mortalities, as has Malignant Catarrhal fever.
While many wild cow-like animals, such as bison, appear to be less susceptible to the effects of certain cattle diseases, the presence of antibodies in their blood show that many of these virus and bacteria live within them for a time. They just appear to have a better innate ability to overcome those infections and resist disease. Some of these animals, such as water buffalo and domesticated gaur (gayal) derive from domesticated stock that is comfortable in confinement. In those that are not, (spooky, fearful) the prolonged cortisol release of chronic stress can overcome that innate disease resistance.
Why Might I Need To Vaccinate Bovids In One Situation And Not In Another?
Most of the infectious diseases that affect bovids are passed to them through close contact with other infected bovids or smaller ruminants such as sheep, goats or antelope. When that threat is not present, vaccination needs are minimal. The exception are the clostridial diseases. Those bacteria are ever-present in ruminant environments. The need for vaccination against them is primarily based on husbandry practices. That is why vaccination needs for the same animal, housed in a zoo or another isolated environment, is much less than the need for the same animals kept in conditions of intensive agriculture.
Some diseases, such as Anthrax, occur only in specific soil types and tend to increase in threat after soil or water disturbances. Others, like foot and mouth disease, rinderpest and brucellosis are confined to certain areas of the world.
The need for clostridial vaccines greatly increases in all ruminants when they are over-fed concentrates, rich hays like alfalfa (lucerne), cubes (hindgut acidosis) , confined at high density, or when animals originating from different sources are combined or trickled into their immediate environment. Excessive consumption of farmed fruits (“fast-fermentors”) due to their high sugar content also favors the overgrowth of clostridia. (ref1, ref2) In North American bison production, placing the animals in a “hot” pasture (overly rich plant growth) is also associated with increased risk of Clostridium perfringens deaths. Zoos sometimes feed all their ruminants similar diets – regardless of the fact that the animal’s natural diets and ability to process feed ingredients are widely different. (ref) These diets can be too “energy dense” – both for the species and for their restricted activity, having too low NDF/NDR vaues.
Your animal vaccine programs might also need to be expanded or booster vaccinations given when stressful situations increase, animal density increases or animals are relocated.
When To Give Bovine Vaccines:
A few weeks before breeding is often the best time to give vaccination boosters to adults.
Fractious animals are generally vaccinated when they are restrained for other purposes.
Offspring are often vaccinated at or shortly before weaning time (3-5 months) with a booster vaccination 4- 6 weeks later. Because infectious disease tends to occur in the younger animals, periodic vaccination of mature animals after their first year or two is less likely to be practiced.
Clostridial Diseases
Clostridia are a normal inhabitant of the intestinal tract of ruminant and other plant-ingesting, animals. Their spores persist for long periods in moist soils rich in organic material and manure. As such, there is no way to prevent exposure to them. Clostridia are inhibited by the normal bacterial flora of the digestive tract. When diet changes or other factors that alter intestinal flora occur, the bacterial can proliferate to toxic levels. In other cases, they enter as wound contaminants and proliferate in the animal’s flesh and muscle, releasing dangerous toxins. (ref) A “7 way” clostridial vaccine is the most common vaccine that large bovid animals are likely to receive in North America subsequent to weaning. Periodic booster vaccinations are rarely administered outside of zoo and research situations. When they are given, it is often because transport to a new location is anticipated.
Inadequate control of gastrointestinal parasites also lowers the animal’s resistance to a number of diseases, including clostridia. (ref)
Most veterinarians, tending to non-domestic bovid animals will administer a 7 or 8-way clostridial vaccine intended for domestic cattle. Breeders and ranchers of these animals generally administer that vaccine as well. Blackleg is the most common clostridial disease they encounter.
Many in commercial enterprises do not repeat the vaccination in animals beyond their first year. That is based on their experience of not seeing Clostridial diseases in their older animals. Zoos are more likely to continue periodic clostridial booster vaccinations throughout the animal’s life as are intensive commercial enterprises. For example, the National Zoo in Washington, DC boosts all their ruminant animals yearly with a 7-way clostridial vaccine plus Tetanus. The largest water buffalo operation in my region does as well and most ranched bison destined for feedlots are given booster vaccinations prior to shipment due to the anticipated stresses they will encounter.
Among the vaccines that are most commonly used in North America to protect bison and water buffalo from Clostridial disease are Merck Animal Health’s Covexin® 8 plus or their Vision 7 w/spur adjuvant which has a lower, more convenient, 2ml volume per injection. Covexin also includes tetanus protection. Bison calves usually receive it at 4-6 months of age with a booster 4-6 weeks later and another the following year. In the midst of an outbreak, it is best to accompany the vaccination with an injection of long acting antibiotic (such as Duplocillin LA) since vaccine protection takes time to develop. The largest bison operation in the United States prefers Boehringer Ingelheim’s Alpha7®; given at 6-8 months of age. But if they don’t see cases in a specific ranch they do not vaccinate against it. The initial vaccination is rarely if ever boosted.
Hemophilus somnus
This organism is quite common in cattle. It is commonly included as an add-on ingredient to multivalent (against many different virus), killed, respiratory tract/digestive tract vaccines given to cattle. Many cattle are simply carriers of the bacteria. The same appears to be true in bison. Hemophilus somnus has been isolated from bison calves experiencing seizures, staggers and blindness, although, as in cattle, it is unclear if the organism is acting alone or if other pathogens are involved. Two inoculations are thought to be required to provide protection but no controlled studies that I know of have been done. Read more about Hemophylus somnus here.
Tetanus
Although tetanus is seen most frequently in horses and lambs, any mammal is susceptible to it, subsequent to puncture wounds or surgery such as castration or dehorning. Read more about tetanus here.
It is zoos that are most likely to vaccinate their non-domestic bovids against tetanus. When they do, it is either by using a clostridial vaccine that includes Clostridium tetani among its ingredients or by utilizing a tetanus vaccine produced for horses.
The National Zoo in Washington, DC specifically vaccinates all bovine animals against tetanus yearly, as does the Jerusalem Zoo in Israel.
Should I Vaccinate Against Common Cattle Respiratory An Intestinal Tract Viruses ?
The majority of non-domestic bovines in controlled situations do not receive any of these vaccines. Perhaps the more inbred species, like European bison, and those living in stressful conditions or close to cattle and sheep should. In making that decision, the associated risk of stress and animal injuries during vaccination restraint need to be factored in.
Many combination vaccines are produced to protect domestic cattle simultaneously against Bovine Virus Diarrhea/Mucosal Disease (BVD), Infectious Bovine Rhinotracheitis (IBR), Parainfluenza 3 Virus (PI3) and Bovine respiratory syncytial virus (BRSV). Many have add-ons against other common pathogenic bacteria of cattle.
The most popular vaccine formulations in the beef cattle industry contain weakened, living virus (modified live virus or MLV vaccines). Although these vaccines are safe in cattle when given as instructed, they are not necessarily safe to use in non-domestic bovine animals. Most veterinarians that use vaccines against intestinal and respiratory virus in non-domestic bovines rely on vaccines that contain only inactivated, non-living (“killed”) ingredients. Even those occasionally cause problems – probably due to the proprietary adjuvants they all contain. The traditional belief was that killed products do not provide as long lasting an immunity as MLV products. It is no longer clear that that is always true. (ref1, ref2)
Inactivated multivalent vaccines, prepared from these organisms, are used extensively in the dairy industry. When used in non-domestic bovids, it is an off-label use. Although there have been few studies on their effectiveness in non-domestic bovines, observations in the field are that they do appear to protect these animals. The largest bison producer in the US only vaccinates with these respiratory/intestinal combination vaccines when faced with a specific problem. In those instances, their preferred product is Novartis’ (killed) VIRA SHIELD® 6. These inactivated vaccines all contain different proprietary adjuvants. He feels he gets the best titers with this one.
Bovine Virus Diarrhea/Mucosal Disease (BVD)
About one third of the bison in the herds of Yellowstone National Park show evidence of prior BVD infection, based on the presence of antibody against BVD in their blood. (ref) Despite that, evidence that the disease causes illness in them is lacking. But there are bison breeders who administer killed vaccines containing BVD to bison destined for feedlots.
Modified live virus BVD vaccines have caused diarrhea when they have been administered to recently weaned bison calves. They may also temporarily depress immunity to other viral and bacterial diseases – particularly in animals that are very young. They should not be given to pregnant non-domestic bovines. Read more about BVD here.
The BVD virus is established in domestic cattle all over the world. Many apparently health cattle carry it. At least two serotypes exist, type 2 tending to be more severe than type 1 in cattle. Neither commonly cause disease in bison unless they are housed in stressful conditions such as feedlots. When killed virus vaccines containing BVD are given to Bison, they require two initial vaccinations of killed (inactivated) vaccine at 3-4 wk intervals and yearly revaccination or perhaps boosters every several years to maintain effectiveness. Controlled studies have not been performed. The ingredients in killed virus BVD-containing vaccines vary between manufacturers. This is particularly true among the proprietary adjuvants used to stimulate immunity. They will occasionally cause problems in younger animals.
Because of these uncertainties, many field veterinarians servicing bison ranches hesitate to administer BVD-containing vaccines unless operations mix bison and domestic cattle.
Never-the-less some water buffalo and bison breeders in America have administered Novartis Animal Health’s VIRA SHIELD® 6 all-inactive IBR, BVD Types I and II, PI3, BRSV, Vibrio and 5 strains of Lepto vaccines to their animals. An AgriLab product, ResProMune 4 I-B-P + BRSV, no longer produced, was also utilized in Water Buffalo herds for many years without side effects. Other vets administer Boehringer Ingelheim’s inactivated-virus Triangle® 9.
Infectious Bovine Rhinotracheitis (IBR, Bovine Herpesvirus-1)
We know even less about the susceptibility of non-domestic bovines to IBR. Again, a bit less than one third of the bison tested in Yellowstone National Park had antibodies as evidence of susceptibility to the virus and prior exposure. (rptref) However, like BVD, no disease could be attributed to it. Read more about IBR here.
The virus is another constituent of the multivalent killed vaccines used to protect cattle from a variety of respiratory and digestive tract infections.
Parainfluenza 3 Virus (PI 3)
As with the former two virus, we only know that bison exposed to it develop antibodies against it. A bit more than one third of the bison in Yellowstone National Park showed evidence of exposure in one 1991-92 survey. (ref) No ill health was associated with exposure to the virus in bison, so as with BVD and IBR, vaccinating them against it at this time is probably unnecessary. The virus has also been isolated from Argentinian water buffalo. (rptref) Although the water buffalo from which the virus was isolated in Argentina displayed respiratory and reproductive problems, it was unclear what, if any, the contribution of PI 3 was or if healthy water buffalo harbored the virus as well. Read more about parainfluenza virus (PI 3) here.
Bovine Respiratory Syncytial Virus (BRSV)
As with the preceding three virus, it is common for free-ranging bison to have been exposed to the virus without showing visible signs of illness. (rptref) Read more about bovine respiratory syncytial virus here.
Leptospirosis
Leptospirosis can occur in non-domestic bovine animals. However, the threat of the disease is closely tied to management techniques and the local presence of leptospira in the immediate environment. Facilities that have experienced losses on their premises tend to vaccinate against it. Those that have not, don’t. One to 7% of the Bison in Yellowstone Park had antibody evidence of prior exposure to leptospirosis organisms. Leptospirosis has been reported by others as a cause of overt disease in bison. (ref1, rptref2) Read more about leptospirosis here.
Vaccines that have been used successfully in Alberta bison when leptospirosis-protection was desired are Merck’s L5 SQ and Novartis’ Vira Shield® 6 + L5. First vaccination is at about 6 month of age, booster 4 wks later, occasionally boosted at 1 year, often never. But most managers of large bison herds only vaccinate when survey blood titers in their stock indicate a need. A few years ago, survey lepto titers were positive in a large bison herd in Nebraska. That was attributed to a wood rat infestation of the round bales they had purchased. That herd was vaccinate – but only that year.
Some veterinarians might hesitate to administer a leptospirosis vaccine that is sold in combination with many other viral and bacterial ingredients if the animals were docile and easily restrained for inoculation at multiple times. In some species, leptospirosis ingredients appeared to lessen the protection afforded by vaccines against the other pathogens for which it was intended. ( read here ) I do not believe that anyone has explored that in bovines.
There is also a report that in cattle, leptospirosis vaccinations can be the source of false-positive brucellosis tests. ( read here )
Malignant Catarrhal Fever (MCF)
The herpes viruses that causes Malignant Catarrhal Fever are common in sheep in North & South America, Europe and Australia, that appear healthy and in the wild wildebeest herds of Africa (OvHV-2 and AlHV-1). Wildebeest also show no evidence of disease (asymptomatic). When the virus infects deer, antelope, water buffalo or bison, it is often fatal. MCF is a significant disease in Indonesian banteng (Bali cattle) as well. In domestic cattle exposed to the virus, the disease can be more prolonged. (ref1 rptref2) Read more about malignant catarrhal fever here.
As of late 2014, no commercial vaccine against MCF exists. However USDA/ARS has made discoveries regarding the virus’ life cycle that may make future vaccines possible. (ref) The only current method of control is to screen for the virus (ref) before animals are introduced to facilities or herds along with a long period of quarantine for new ruminant animals.
Brucellosis Brucella abortus
Like all ruminants, non-domestic bovids are quite susceptible to brucellosis. Because chronic infections decreases bovine fertility and because the organism can be passed to humans, it is a concern for public health officials and veterinarians the world over. Extensive culling of infected animals and periodic testing have eliminated the disease from many European countries. Read more about brucellosis here.
Both American bison and water buffalo appear to be more resistant to the disease effects of Brucella abortus than cattle (ref) ; but symptoms similar to those seen in cattle do sometimes occur when farm-raised bison become infected. (ref) Yellowstone Park’s buffalo herds have been carriers of brucellosis since at least 1917. It is thought that it was introduced into the herds by domestic cattle. Recent surveys of wildlife in that area found that a substantial percent of the elk (3.7-21.9%) and bison (63.9%) there have been exposed to Brucella. (ref)
In the United States, federal officials are under great pressure from animal rights activists to not employ traditional culling methods used to eliminate disease from bison. Under that pressure, they agreed to consider vaccinating the entire free-ranging bison population with a newer anti-brucellosis vaccine, RB51. The US agricultural agency, APHIS, paints a rosy picture of the possibilities for success. (ref) But the effectiveness of that vaccine in such a situation, remains in dispute and many professionals believe that is an entirely unrealistic expectation. (ref) In water buffalo, the RB51 vaccine was ineffective in preventing abortions. (ref) Some Colorado bison producers vaccinate their heifer calf bison against brucellosis as well. The RB51 vaccine (“Bangs shot”)is said to be about 70% effective in cattle…………(In the United States, laws regarding the use of RB51 vary state by state. )
Anthrax
Anthrax disease appears in all ruminant animals in areas called “hot spots” or “anthrax belts”. Those are areas where specific soil types and climatic conditions occur that favor the anthrax organism (Bacillus anthracis). When outbreaks occur, they are usually after severe climatic events such as flooding or the disturbance of land and soil. One farm may see many cases while a neighboring farm sees none. Read more about anthrax here.
It would be unlikely for zoos to vaccinate non-domestic bovine animals against Anthrax. However, less isolated bison and water buffalo residing in anthrax belts might benefit from vaccination. In the United States, the current (2014) sole manufacturer of anthrax vaccine is Colorado Serum Company. (ref) Trial use of the vaccine in bison indicated that the immunity conferred by the vaccine did not always last a full year in bison. Some veterinarians have experimented doubling the recommended initial dose. Other veterinarians in anthrax areas vaccinate bison once at 6 month and again at 12 months or space out two 1ml initial injections. The largest user in bison administers the double dose using a needleless injector. I was told that they got a 10 fold increase in titer; but that it stayed that high only for about 6 months.
Bluetongue Epizootic Hemorrhagic Disease EHD
Bluetongue and EHD are two, slightly different virus. Both can affect non-domestic bovine animals. Both are spread by small, flying, biting insects (culicoides = midges = “no-see-ums”) Usually, the disease in bisons is short lived with, perhaps a period of temporary joint stiffness and lameness. The disease is often considerably more severe when it occurs in antelope and deer. Vaccines exist, their effectiveness is debatable and they are rarely given. Read more about bluetongue here.
Johne’s Disease Paratuberculosis
All hoofstock (Artiodactyla) are susceptible to this disease. The organism is one of a class of slow-growing bacteria called acid fast organisms. Many apparently healthy animals are silent carriers of the bacteria and shed the organisms in their manure. The disease is occasionally seen in American bison and water buffalo and has been reported in guar, anoa and domesticated banteng as well. Read more about Johne’s disease here.
Boehringer Ingelheim markets a killed vaccine to reduce the effects of Johne’s disease in infected herds of cattle through the vaccination of young calves (Mycopar®). Its use has not been proven to be more effective than strict sanitation measures and culling symptomatic adults that spread the disease to their offspring. I do not know of the vaccine’s use in non-domestic ruminants.
Mycoplasma bovis
This organism is routinely found in domestic cattle (40% to 60% of healthy cattle carry it). When it causes disease in domestic cattle, it is generally in young animals as part of the bovine respiratory disease complex where multiple respiratory tract virus (along with secondary bacteria) attack the respiratory system. But in bison, Mycoplasma bovis appears to be a primary pathogen, capable of causing disease on its own – particularly when bison are crowded together in feedlot situations. In those situations (and occasionally among non-stressed bison) pneumonia and/or the lameness associated with polyarthritis can occur. Up to half the herd has been lost to this disease in the US North West. Read more about Mycoplasma bovis here.
Cattle vaccines do exist. They are of varying effectiveness. (ref1, ref2) There are worries that such vaccines might make the situation worse in young bison by actually increasing their sensitivity to the disease. (rptref) The country’s largest bison producer vaccinates all bison yearly against M. bovis. The vaccine is produced for him using two bison isolates from his stock by Newport Labs. Overrun production can be purchased by other breeders – you have to call to see when they might have it available. This is a newly recognized problem and it will take time to sort things out and discover the best ways to control it.
Rabies
A few zoos, such as the National Zoo in Washington, DC, vaccinate their bovine animals against rabies. In Texas, that is a permitted off-label use of any brand of rabies vaccine that is approved for livestock. Read more about rabies here.
Some Vaccination Protocols For Bovids Around The World
Some Asian water buffalo herds receive Clostridium perfringens-containing vaccines. Veterinarians in Botswana tell me that no cape buffalo herds maintained in Southern Africa receive vaccinations of any kind. There was some talk about vaccinating those of Kruger National Park against bovine tuberculosis which has spread through the population as far north as southern Zimbabwe and of vaccinating Namibian cape buffalo against (endemic) Foot and Mouth Disease in the hope of lessening its spread to local cattle. But no action has yet been taken. The Jerusalem Zoo does vaccinate all its ruminants against FMD, and large bovids against brucellosis as well. The National Zoo in Washington, DC vaccinates all its ruminants yearly with 7-way clostridium bacterim and tetanus toxoid, and yearly against rabies as well because of the periodic rabies epidemics that occur in the wooded park that surrounds it. (ref) Read other non-domestic bovine vaccination suggestions here.
Sheep And Goat-like Animals (ovi + caprids = ovicaprids)
These smaller ruminants are common in zoos throughout the world. There are so many species in the group – within the antelope alone there are 91. Common species in captivity in North America includes dama gazelles, scimitar horned oryx, addax, aoudad, eland, bongo, markhor, blackbuck and sable antelope, springbok, eland, waterbuck, impala, lechwe and mouflon.
Besides being on public display, these animals are extensively farmed in the United States in both free-range and more restricted environments (and valued at over 700 million dollars in 2007 alone). The first three I listed above are endangered species in their native countries; but in surplus here.
On those large American game ranches, wild sheep, goats and antelope are rarely if ever vaccinated. When done, it is almost always to comply with government transport regulations. That is because the ranchers have learned through experience that more animals are lost to injury in the process of vaccination than might be saved through vaccination. In zoos and confined breeding programs, however, vaccination is an important tool in preserving small ruminant health. That is because as animal numbers per area rise and species mix, the probability of bacterial and viral infectious diseases rise as well. It is not only diseases that pass from animal to that animal that rise. As diet shifts away from their wild native pasture, forbs and brush (shrub tips and buds) and moves to rich commercial hays and concentrates, the clostridial diseases increases in frequency as well.
Clostridial Diseases
As I mentioned, when small ruminants are naturally distributed on open range, their vaccination needs are minimal. But when they are penned or their numbers increase above natural levels, the potential for a number of diseases caused by the clostridial bacteria increase. Keeping animal numbers above the natural carrying capacity of the land or in confined quarters disturbs the natural grazing patterns and plant preferences of animals. That alters the normal protective bacterial flora of the ruminant digestive tract and increase their susceptibility of these animals to the clostridial diseases. Veterinarians are fortunate to have excellent vaccines to deal with this problem.
Clostridium perfringens
The most common immunization given to small, non-domestic ruminants is one against C. perfringens bacteria. As it is commercially sold in combination with Clostridium tetani (the cause of tetanus) and sold under a “CDT”,“CD&T” , “CD3+T” or similar name. Read more about Clostridium perfringens here.
The cause, Clostridium perfringens (usually type C or D) are a normal part of the intestinal flora of all ruminants. Overeating disease or enterotoxemia tends to occur when diets rich in protein, starch and sugars and low in long-stem fiber are fed. In those conditions, rumen pH drops (increased acidity) and stomach and intestinal motility slows allowing C. perfringens to rapidly overgrow the animals normal bacterial flora and increase to toxic levels.
As I mentioned before, game ranches here do not normally vaccinate. But in my part of the world, South Texas, when we do wish to protect exotic hoof stock from this disease, Merck’s Vision CD-T with Spur adjuvant is the most common used. There are other veterinarians here who prefer to use Boehringer Ingelheim’s Bar Vac CD/T. Generally, the vaccine is give soon after weaning or when adults are darted or trapped for other reasons. A second injection 3-4 weeks after the first would be optimal if the animals are easy to capture and restrain (which they rarely are). Yearly boosters are desirable – preferably a month or so before the breeding season so that temporary immunity is passed on to their offspring.
7 & 8-Way Clostridial Vaccines
Most zoos and some veterinarians servicing the exotic hoof stock industry prefer giving a vaccine that protects against a broader range of clostridial pathogens. The zoos that administer them generally do so annually. It is a considerably less common practice in European zoos than in American zoos, yet clostridial diseases are a very rare problem in those overseas collections. Veterinarians there, with whom I have discussed this, often mention differing feeding practices as the likely reason it is so uncommon in their facilities.
The National Zoo in Washington administers these vaccines annually to all ruminants (Artiodactyla); I am told that Omaha’s Henry Doorly Zoo does as well. In open-range and drive-through game parks like Orana Wildlife Park in Christchurch, NZ, the vaccines are only given when the hoof stock are darted and restrained for other reasons. Brand of vaccine that are often mentioned in the US as used in exotic hoofstock are Merck’s Vision® 7 with SPUR adjuvant, or their CAVALRY® 9 as well as Novartis’ Clostri Shield® 7 . They try to give a second booster a few weeks after the first – if that is a safe option for the animals.
These inactivated multiple detoxified toxin products are also part of the annual exotic hoof stock vaccination program at the Jerusalem Zoo and facilities in Dubai. (ref)
Tetanus
Most facilities that vaccinate, administer tetanus protections as part of the CDT”,“CD&T” or “CD3+T” vaccines that are given against Clostridium perfringens or one of the 7 & 8-way clostridial vaccines mentioned above . It would be unusual to administer one without the others in that environments that increase the dangers of one often increase the risk of the others. Read more about tetanus here.
Respiratory/Diarrhea Disease Complex
You can read more about the many virus and bacteria that interact in these complicated diseases in the previous section on larger bovid hoof stock.
The virus involved in these diseases often work in tandem to potentiate the disease produced. Secondary bacterial invaders take part as well. Disease is generally associated with crowding, stress and the introduction of new animals into an existing group or heavy parasitism. Changes in management practices are more effective in solving these problems than vaccines, but vaccines can play a part as well.
The vaccines used in these smaller hoof stock are the same ones mentioned in my section on larger non-domestic cow-like bovids like bison. It is always safer to administer, inactivated (killed) vaccines. In South Texas, Boehringer Ingelheim’s Triangle® line of vaccines are often used. (ref1, ref2)
Besides BRSV and BVD, Pasteurella multocida and Mannheimia haemolytica (aka Pasteurella haemolytica) are often implicated in respiratory disease in these smaller ruminants. When that is the case, Colorado Serum Company produces an inactivated vaccine (bacterin) directed against them.
Anthrax
I do not know of any display facilities that vaccinate these smaller ruminants against anthrax. Although anthrax belts run through several of the South Texas ranches that hold large populations of these animals, none I know of vaccinate against anthrax either. The vaccine’s administration has been discussed as, perhaps, justifiable in small hoof stock destined for release in areas where anthrax exists. (rptref) After natural catastrophes that stir up soils in anthrax zones, vaccination of all ungulates might be prudent. Read more about anthrax here.
Epizootic Hemorrhagic Disease EHD Bluetongue BTV
In the United States, these related virus have primarily been a problem in deer farms. When a vaccine against these virus is administered, it is generally because of losses on other deer farms in the same area. Those areas in the United States and Europe have been steadily increasing in number – expanding into areas once thought to cold for the transmitting vector (culicoides midges =noseeums ) to over-winter. Read more about epizootic hemorrhagic disease here.
These virus have the potential to infect all small hoofstock. Most infections in these small ruminants (other than deer) seem to be mild inapparent infections that cause few or no clinical signs. But the viruses have, on occasion, killed bighorn and mouflon sheep as well as pronghorn antelope. In the United States, the few zoos that vaccinate against it, administer the vaccine to their cervids (deer) and antelope. Most of Colorado Serum’s EHD vaccine production goes to deer farms, but a few shipments are routed to zoos in epidemic zones.
The two large deer breeder coops in the USA provide their members with an autogenous (produced from isolates from the customer’s own herd) vaccine. One provides it only to members; the other is more liberal in its sales policies.
Newport Laboratories offers a vaccine to your veterinarian though more open channels. It’s composition changes from year to year, based on the strains of the virus most common that season. In 2014, three strains (1, 2 & 6) of EHD are included of the 8 that circulate worldwide, as well as 4 (12,17,11 & 3) of the 24 strains of BTV that are known internationally. Use of their vaccine requires the approval of each state’s official veterinarian. It can not be legally shipped internationally. The manufacturer suggests that livestock receive the vaccine in the spring, prior to breeding and that the offspring receive it at 6-8 wks of age with a booster 2-4 weeks later. (ref)
These virus have recently become a problem within the sheep and cattle populations of Europe. (ref) Mortalities there have also occurred in blackbuck antelope, mouflon sheep and ibex as well as a number of larger non-domestic hoofstock.
The killed vaccines currently available are helpful but not always protective. Many commercial deer breeding operations in the USA supplement their use with commercial fogging machines (using synergized permethrin) during periods when the carrier insects are plentiful.
Leptospirosis
You can read about the various vaccines against leptospirosis and their use in my section on large non-domestic bovids that precedes this one. Read more about leptospirosis here.
Many zoo publications mention vaccination against leptospirosis as an option. Often the words, “geographically appropriate” are used to qualify its use. I am not sure what they had in mind and I know of no one using leptospirosis vaccines in smaller non-domestic ruminants. Most rely on reducing exposure with management changes that reduce vector sources (eg rodents) following a case.
Rabies
The National Zoo in Washington, DC vaccinates its gazelles and other small hoofstock against rabies every three years. They are uniquely situated in an urban park with an extremely large raccoon population that has experienced periodic rabies epidemics. (ref). I am told that Henry Doorley Zoo in Nebraska vaccinates their hoofstock against rabies as well. Read more about rabies here.
Foot And Mouth Disease FMD
This is one of the diseases that North American veterinarians like me are blessed not to have to deal with. But in some parts of the less-developed world it can be a serious problem in exotic hoofstock. I know it appears as a periodic problem in exotic hoofstock in the Middle East. You can read about how veterinarians utilize vaccines to help control it there in these reports: (ref1, rptref2, ref3) Read More about foot and mouth disease here.
In Sub-Saharan Africa, the principle reservoir of FMD appears to be water buffalo that show few if any symptoms of the disease. (ref) From there, it apparently makes its way to the Middle East. Although much of South Africa is free of it, the Kruger National Park is an endemic foot-and-mouth-disease area because of its African buffalo and FMD periodically jumps to other cloven-hoofed ruminants there.
FMD reappeared in Europe in 2011 (in Bulgaria). I believe that as of late 2014, all 28 EU members are free of it. However, it is present next door in Turkey.
Goat Plague aka Ovine Rinderpest aka Peste Des Petits Ruminants (PPR)
This is another hoof stock disease veterinarians do not currently have to deal with in North America. It is caused by a morbillivirus, from the same group that causes human measles and canine distemper. If interested, you can read how it is dealt with through vaccination in other areas of the world the following articles: (ref1,rptref2) Read more about rinderpest here.
The virus is quite similar to the rinderpest virus and the vaccines cross-protect. Some believe that eland, kudu, wildebeest, ourebi and impala are more susceptible to overt disease than the smaller gazelles. (rptref) Outbreaks in Africa in these exotic hoofstock have also been caused by the rinderpest virus itself. (ref) In domestic cattle the disease is often subclinical. (ref) Domestic goats are highly susceptible to severe PPR disease. (ref)
Effective live attenuated vaccines against PPR are available that are thought to give a life long immunity. (ref)
Contagious Caprine Pleuropneumonia CCPP
This disease is caused by Mycoplasma (M. capricolum or M. mycoides The second organism also affects large bovids). (ref) It is generally considered a disease of domestic goats, in which it causes severe, often fatal, pneumonia. Outbreaks occur periodically in Africa, Asia and the Middle East and have extended into Eastern Europe. The United States and Canada are free of the disease. Although it is associated with goats, it affects small non-domestic ruminants as well. (ref1, ref2) Read more about CCPP here.
Deer-like Animals (cervids )
As with the goat and sheep-like animals, most deer will do quite well in collections around the world without vaccinations. Optimal management techniques, proper diet, uncrowded facilities and isolation from new stock and other ruminants that might bring disease into the facility are sufficient to maintain good health.
But there are situations where optimal density and husbandry are not practical solutions. Breeding herds of whitetail deer, reindeer and elk require higher animal densities and supplemental feeding; animal densities in zoos are quite high as well. And some diseases, like Epizootic Hemorrhagic Disease, Bluetongue. West Nile Fever and the clostridial disease are not dependent on animal density. The first three are carried by biting insects that can be blown onto the premises from quite some distance away. When the surrounding area experiences an outbreak or birds migrate through the area, good management may not sufficient to protect the deer from insect carriers. (ref1, ref2, ref3)
Here in Texas, there is potentially a third (genetic) problem. Breeding whitetail deer is a $900 million+ industry directed at producing “genetically superior trophy bucks” However, what “genetically superior” in this case means is a large deer with an enormous rack of antlers – not a “scrub” deer with the resistance to disease and resilience that Nature intended. (ref)
Similar genetics manipulations for specific market traits make New Zealand red deer population and reindeer quite different in their disease susceptibility than their wild cousins that are culled by natural selection. (ref)
Epizootic Hemorrhagic Disease & Bluetongue EHD & BTV
In the United States, more deer are vaccinated against Epizootic Hemorrhagic Disease than anything else. That is because these two diseases are the number one threat to commercial deer breeding here. Deer concentrated in breeding facilities are hardest hit, but even those in the wild are thought to have experienced 20% losses. Most other hoofstock become silently infected and form protective antibodies without ever showing disease symptoms. (ref) Read more about this disease here.
EHD/BTV are a group of related Orbivirus that sporadically (off and on) cause disease in all areas of the world where cattle and sheep production occur and the biting midges that transmit it are found. These virus exist in many serotypes or strains with little cross-immunity protection. The primary viruses responsible for the yearly epidemics change from year to year. That is why a commercial vaccine with a stable formulation has never been available. United States laws allow for “custom” vaccine production incorporating virus or bacteria obtained from a particular herd. The vaccine has its limitations. It is not always effective and it is unclear if that is because infection was with viral strains not included in the vaccine, administration errors, specific deer genetics, concurrent disease or ineffective vaccine.
Because EHD/BTV disease often appears in a herds only every few years, it is unclear if the vaccine was responsible for the years EHD/BTV did not cause mortalities. Regulations that govern the testing of custom-made vaccines such as EHD/BTV are less stringent than those that receive permanent USDA approval. To the best of my knowledge, the producers do not have to submit evidence that the vaccines are effective.
The manufacturers, Newport Laboratories, suggest the vaccine be given to fawns at weaning and boosted in 3-4 weeks and then given to does prior to breeding to give some temporary immunity to the fawns.
Malignant Catarrhal Fever MCF
This is another viral disease of wide distribution wherever sheep and goats are farmed or in areas of Africa inhabited by wildebeest. There are at least 10 strains of the Alcelaphine (antelope) Herpes virus that cause it (AHV-1 of wildebeest, AHV-2 caprine/goat and ovine/sheep forms). Read more about MCF here.
Although one study found 61% of goats and 3% of sheep carried or had been exposed to MCF, almost no sheep and few goats become ill. (ref) Farmed deer and Zoo deer in epidemic areas, however, are particularly susceptible. (ref1, ref2) It has been a particularly lethal problem in farmed European red deer in New Zealand and elsewhere. Caribou herds in close contact with sheep have also been affected.
The MCF virus has been particularly difficult to grow in the laboratory; so as of 2014, there are no commercially available vaccines – although some are in development. (ref)
Respiratory/Diarrhea Complex
Pneumonia and diarrhea are the two most common causes of death in intensively farmed deer in North America. (ref) Some producers administer, custom vaccines produced against a very large number of organisms that are commonly isolated from deer in those cases. Those vaccines commonly contain Pasteurella multocida, Fusobacterium necrophorum, E. coli, Mannheimia haemolytica, Arcanobacterium pyogenes, Bibersteinia trehalosi , Truperella pyogenes and Mycoplasma hyopneumoniae. Many also include EHD/BTV protection – all in a single vaccine. Their use is controversial, the benefits of the vaccine hard to evaluate. Read more about respiratory/diarrhea complex here.
Antibodies against three of the common cattle respiratory virus (IBR, BVD, PI-3) are found in caribou and elk – but they appear resistant to disease and generally remained free of symptoms in natural settings. (ref) The same is true in whitetail deer. (ref)
In intensive North American deer farming, deer have both been vaccinated with inactivated cattle vaccines widely used in the dairy industry. Some utilize Boehringer Ingelheim’s Triangle 9 at 12 and 16 weeks of age and boost annually.
Clostridial Diseases
Deer, like all ruminants, can be vaccinated against the clostridial diseases utilizing vaccines approved for sheep, goats and cattle. (ref) The vaccines are effective. Depending on disease experience within the group, either a Clostridium enterotoxemia/C. perfringens/tetanus vaccine is used (aka “CDT”,“CD&T or “CD3+T”) or a broad spectrum clostridial vaccines such as Novartis’ Clostri Shield 7 or Merck’s Calvary 9 (all generally at 3 months and boosted 2 wks later, then annually). Some reindeer breeders alternate years, giving the 7 or 8-way one year and the CDT the next. Read more about clostridial diseases here.
Deer and other hoof stock are susceptible to fatal clostridial overgrowth when they are fed inappropriate diets that are too high in simple sugars, starch or protein (low NDF/NDR rations) (ref) Most deer, other than elk, are browse nibblers and some, such as moose (and reindeer/caribou), do quite poorly when forced to eat nutrient-rich diets suitable for cattle. (ref) Those differing feeding habits and abilities to process nutrients are sometimes not sufficiently appreciated. (ref) Also, as with the larger bovine ruminants, excessive consumption of farmed vs wild produce (“fast-fermentors”) favors hindgut acidosis due to their high sugar and starch content (ref) and the overgrowth of clostridia. (ref1, ref2) So does the free access to rich pasture like alfalfa (lucerne), or over-access in hay or cube form. When nutrient-rich diets cannot be avoided, vaccination against the clostridia is a valid and effective option.
Tetanus
Tetanus is also a clostridial disease. Read more about tetanus here. Some Zoos, such as the National Zoo in Washington, DC, do make tetanus vaccination a specific goal of their vaccination program. Most others, give tetanus protection to hoofstock as as a side benefit of using a “CDT”,“CD&T” or “CD3+T” vaccine directed primarily against Clostridium perfringens. The few remaining forest reindeer now residing at the Helsinki Zoo receive yearly vaccination with Merck’s EQUILIS® te, a univalet tetanus product designed for horses.
Collibacillosis
Certain strains of the bacteria, Escherichia coli , are capable of causing fatal diarrhea in young deer. Generally, those are offspring that, for one reason or another, did not receive sufficient colostral antibody in their first days of life. Even after the short window of time the doe’s milk antibodies can pass into the fawn’s blood stream, fawns still benefit from the protective value of antibodies present in the doe’s milk within the fawns intestine. We are still uncertain if colibacillosis scours is due to insufficient maternal antibody or if certain strains of E. coli are more able to break antibody resistance than others (invasive serotypes) , or if both those factors are involved. Collibacillosis problems are common in young elk, red deer and reindeer in farmed or crowded situations. Both diarrhea and meningitis occur. Read more about colibacillosis here.
Newport Laboratories markets a multivalent vaccine that incorporates several deer isolates of E. coli along with other pathogens. In the past, a killed K99E Colivaccine was given to pregnant does and boosted 2-4 wks closer to parturition in the hopes of boosting the antibody content of their colostrum. It has never been confirmed that that technique is effective.
Several other ruminant pathogens can be involved in scours in young deer. Merck’s Guardian® Calf scours vaccine contains the K99E strain of E. coli along with some of those other common pathogens. Although I know of no deer breeders using it, one respected Canadian expert considers vaccines of that nature to be, at the least, harmless. (ref) Some US fallow and whitetail breeders utilize Boehringer Ingelheim’s Bar-Guard 99TM oral E. coli K99 whole cell antibodies to provide passive (temporary) immunity against E. coli K99 in their new born deer (2-3cc/deer).
Leptospirosis
Leptospirosis is not a common disease among deer in zoos or farmed in North America. When the disease is seen, rodent and raccoon vectors contaminating water sources and the environment with their urine are thought to be the primary sources (although even stray cats are a potential vector). (ref) In Nevada bison, wood rats arriving in round bales were thought to be the source. Leptospirosis is not a significant problem in wild deer in North America, although whitetail deer, elk and moose occasionally have antibodies as evidence of prior exposure. Read more about leptospirosis here.
New Zealand has an extensive deer and elk farming industry. It rivals, and perhaps surpasses, Texas in its scale. In New Zealand, leptospirosis has been a recurrent problem in deer herds since the 1980s. (ref1, ref2) In those herds, Leptospira pomona causes abortions, and elevated losses of nursing and recently weaned deer. Those infected with L. Hardjo-bovis are less likely to suffer overt disease. L. i. Copenhageni has also been isolated.
Merck markets two leptospirosis vaccines approved for use in deer in New Zealand, Leptavoid® 2 (L. .Pomona and L Hardjo antigens) approved for sheep, beef, dairy cattle, swine and deer or Leptavoid® 3 (inactivated Leptospira interrogans serotypes Pomona, Hardjo and Icterohaemorrhagiae antigens) for beef, dairy cattle and deer. Both are extensively used in the deer industry. (ref) Young deer are vaccinate at about 3 months of age and boosted 4-6 weeks later. Unvaccinated adults get a “sensitizer” (initial vaccination) in the neck and a booster 4-6 weeks later. After that, they are boosted yearly – does about 3 weeks prior to calving. Some fallow and whitetail breeders in the USA, utilize Merck’s Covexin® 8 leptospirosis vaccine (2cc at 12 & 16 wks, boosters yearly).
Pasteurellosis Pasteurella multocida, Hemorrhagic Septicemia
Pasteurella multocida and similar pasteurella are found the upper respiratory tract , mouth and throat (pharynx) of many animals that are not ill. In those locations, they are considered part of the animal’s natural bacterial flora. However, under stress, the organism can move into the lungs, causing pneumonia, into regional lymph nodes causing abscesses, or into the blood stream causing septicemia (“blood poisoning”). Many strains or serovars exist. Some cause common snuffles in rabbits, some are responsible for fowl cholera of chickens, turkeys ducks and geese others are involved in atrophic rhinitis of swine. Strains appear to vary in their ability to cause disease. Most, if not all, can jump from one species to another. It is one of the organisms commonly involved in shipping fever of cattle. Outbreaks in deer often follow periods of stress. (ref1, ref2) Read more about pasteurelosis here.
In New Zealand deer farms and zoos, it is associated with stressors including transport, inadequate nutrition, overcrowding, concurrent viral infections, inclement weather (especially hot temperatures) heavy rains and wind and high parasite loads (particularly lungworms). (rptref)
One of the many shotgun vaccines prepared by Newport Laboratories contains inactivated Pasteurella multocida, along with EHDV virus, BTV (bluetongue) virus, Mannheimia (Pasteurella) Haemolytica, , Fusobacterium Necrophorum, Clostridium Perfringens Type A and Arcanobacterium Pyogenes.
Necrobacillosis Fusobacterium necrophorum, Lumpy Jaw, Foot Rot, etc
Fusobacterium disease has so many names because it presents in so many different ways and in so many species of animals. The “lumpy jaw” form is often seen in kangaroos. It is a common pathogen isolated from sick deer. In young deer, the infections is often systemic and leads to rapid death, in older deer, longer term foot or mouth and throat lesions are more common. The organism generally enters the deer’s body through a cut or scrape and forms an abscess – often not far from the point of entry. The most common form in whitetail deer are abscesses of the jaw aka “Lumpy Jaw” – It can be found alone or in association with other pathogens like Actinomyces. I have also seen it present as paralysis due to infection of the spine. Exposure to these organisms can not be prevented as it is often present in the intestinal tract of disease-free animals. Many species of deer throughout the world develop fusobacterium-related disease when they are subjected to overcrowding, malnutrition, or chronic stress that lowers their immune resistance. Read more about necrobacillosis here.
Fusobacterium is another of the antigens incorporated in Newport Lab’s bacterin vaccines for deer.
Another option is Novartis’ FUSOGARD® (It is an “off label” use, The product is labeled for use in cattle). Neither have been scientifically tested for their effectiveness in deer and neither are an acceptable alternative to husbandry changes that lessen the likelihood of the disease. A primary and booster vaccination are required. The first is generally given to young fawns (1/4 CC Fusogard Sub Q at 2-3 weeks of age, revaccinated in 2-3 weeks).
A group of venerable microbiologist that direct the IUMS, seem compelled to periodically give bacteria completely new names designed to confuse veterinarians and others that are concerned with animal health. The next two bacteria, currently called Truperella and Bibersteinia, led a number of prior lives under various different aliases.
Truperella pyogenes (= Arcanobacterium aka Corynebacterium aka Actinomyces ) pyogenes Cranial Abscessation Syndrome CAS
Bucks are particularly susceptible to infection with this bacteria subsequent to antler damage or loss. In those instances, Truperella can penetrate the skull and cause abscesses in the brain. The organism is also thought to be capable of causing pneumonia – at least it is often found with other bacteria in deer with severe lung disease. It is a common isolate in postpartum metritis (after-calving womb infections) of dairy cattle. (ref) Truperella was thought to be a common opportunistic pathogen – only taking advantaged (opportunistic) of a stress-weakened animal or working in tandem with other bacteria to cause disease. (ref) But in some cases, it was thought to capable of causing illness in deer on its own. (ref)
T. pyogenes is another organism incorporated in Newport Laboratories multivalent inactivated deer vaccines. Penned deer occasionally have recurrent losses due to what they still call A. pyogenes (Truperella) associated lung infections. Since the 1980s, a custom bacterin produced against A. pyogenes was the only vaccine the Kerrville Texas Whitetail Deer Center administered to their deer. In 2014, they changed to the Newport Labs 9-way due to the expense and time involved in ordering a univalent (single bacterial ingredient) custom vaccine
Bibersteinia trehalosi aka Pasteurella haemolytica type T aka Pasteurella trehalosi, aka Mannheimia haemolytica
This is another organism that is chiefly a problem in the deer farming industry. It is also an ingredient in Newport Laboratories 9-way (multivalent) pneumonia/fawn diarrhea vaccines. Like many of the organisms contained in that vaccine, B. trehalosi is a common inhabitant of the upper airways of deer and sheep.
Under non-stressful conditions, they causes no disease. When the animal’s immunity is decreased due to other issues, it takes advantage of the situation to invade other areas of the body. One of those underlying causes that allow B. trehalosi to become pathogenic are heavy lungworm infections due to overcrowding and cohabitation with cattle and domestic sheep. But B. trehalosi is almost never the sole underlying cause of a health problem.
Yersinia pseudotuberculosis Yersiniosis
Pseudotuberculosis or yersiniosis is another disease that occasionally causes illness in deer. The organism is widely distributed in animals so deer exposure is quite likely to occur. But like the preceding two organisms, Yersinia pseudotuberculosis only causes disease when the animals immune system has been weakened or the animals are under stress. That can be the stress associated with weaning, hard winters, crowding, poor nutrition or inclement, rainy weather. Some strains and species of farmed deer may be more genetically susceptible to yersiniosis than others. There are many serotypes (strains, serovars) of the organism. Some are thought to me more pathogenic than others. Yersiniosis is a major health issue in farmed deer in New Zealand. These are usually deer in their first year that experience severe diarrhea and subsequently die of dehydration and blood acid/base disturbances. It sporadically (occasionally) kills small hoofstock in zoos as well. Read more about yersinia here.
In New Zealand, Merck markets YERSINIAVAX® vaccine, composed of inactivated Yersinia pseudotuberculosis serotypes I, II, III. The product is approved for use in deer. Two ml of the vaccine are given in the neck sc, 3-6 weeks apart – prior to anticipated periods of stress. The vaccine is said to be quite effective. The veterinary school in Utrecht, Netherlands made available another killed pseudotuberculosis vaccine for use in European zoos (Pseudovac®). I do not know if it is currently available.
West Nile Virus WNV, West Nile Fever
West Nile Fever is a mosquito-transmitted, viral disease that occurs on all continents in a wild variety of animals including deer. Most cases are subclinical – no disease signs or only mild illnesses being noticed before antibodies rise high enough to purge the virus from the animal’s body. But occasional cases lead to fatal encephalitis. Read more about WNV here.
Some believe that native North American deer are naturally immune to the disease effects of WNV. That although they are commonly exposed to the virus, they overcome it without visible illness. Others believe that the WNV does not replicate in deer. One study found 0.9% of hunter-bagged deer in New Jersey has been exposed to WNV. West Nile virus is certainly not a currently important cause of death or illness in wild whitetail deer. One fatal case in a wild whitetail deer has been reported. (ref)
The situation in North America’s farmed reindeer has been different since 2002. Since then, Minnesota and Wisconsin breeders have experienced a number of WNV cases in their stock. Being a new problem for them, it was first suspected that the staggering and nervous system symptoms were do to Chronic Wasting disease or brain worms. Eventually WNF was found to to be the cause. Many reindeer breeders now immunize their animals using schedules and vaccines that have been successfully used in llamas and alpacas. Most use Merial’s RECOMBITEK® Equine rWNV vaccine (some had tried Zoetis’ WEST NILE-INNOVATOR in an initial trial (ref) but experienced reactions in their herds). In llamas, three IM injections of the Merial/Boehringer Ingelheim ‘s vaccine given at 3-5 week intervals stimulated adequate antibody response. I do not know if similar data on effectiveness exists for reindeer, but many reindeer breeders follow the llama protocol. The vaccinations are begun in early spring, prior to mosquito season. Vaccination of pregnant females is avoided. Boosters given the following springs. Some run blood titers and only give the complete initial 3-shot series to animals that have no titer.
Camels And Camel-like Animals (camelids)
New and Old World camels spring from the same ancestors as ruminant sheep, antelope, deer and cattle. Camelids regurgitate the fermented plant material (cud) they have eaten similar to ruminants; but because they have a three-chambered stomach rather than the four-chambered stomach of a ruminant, they are not true ruminants.
However, because camelids are even-toed hoofstock – in the same group (Artiodactyla) as cattle, antelope, deer, giraffes, sheep and goats – they have the potential to develop many of the infectious diseases those species do. Some experts believe that it is the genetic distance between camelids and ruminants that, make them more resistant to the ill effects of some of those common hoofstock diseases such as tuberculosis, brucellosis, and many of the viral diseases of cattle sheep and goats. (ref)
Most zoos and camelid breeders in North America have vaccination programs for their Old World and New World camels. Those in Europe and elsewhere with camelid collections are considerably less likely to vaccinate. For instance, Norway’s Kristiansand Zoo and the Copenhagen Zoo do not find need to give their camels any vaccines and the working camels of Asia and North Africa are rarely vaccinated. A small number of camelid breeders in America I know of do not vaccinate their animals either.
When camelids do receive periodic vaccinations, the one most commonly given around the World is to protect them against Clostridium perfringens and Clostridium tetani, two bacterial organisms that are widely dispersed in our natural environment. Camel collections throughout the world – from American zoos (eg Rolling Hills Zoo in KS, Cheyenne MT Zoo CO, Potter Park Zoo, MI, Smithsonian/ National Zoo, etc. ) to the Bedouin camels of Jordan, the milking and racing camels of the UAE/Dubai and the photo-op/tour camels of Israel all receive this vaccine periodically. (ref)
Clostridium perfringens and Tetanus Vaccination
Livestock vaccines are often marketed containing a combination of these two bacteria. When that is the case, the product usually caries a “CDT”,“CD&T” , “CD3+T” or similar name.
The need for vaccination against Clostridium tetani (tetanus) is exposure driven. Animals usually become ill only after the organism enters an accidental wound or puncture or through the incision of a recent surgery (eg castration). (ref)
The need for Clostridium perfringens (enterotoxemia/septicemia) vaccination is management-driven. The disease is associated with unhealthy changes in natural bacterial population of the animal’s digestive tract. Generally, the cause is a diet too rich in sugar starch and protein. ( ref1, ref2, ref3 , ref4 ) Enterotoxemias are particularly likely to occur when changes to richer diets occur too abruptly in younger animals.
It is common to vaccinate New and Old World camelids with this vaccine a month prior to weaning and then yearly and to re-vaccinate pregnant females 4-6 weeks before they deliver their crias or calves. Young animals might benefit from earlier vaccinations if their blood IgG levels were initially low; and from additional boosters. Some drop the vaccube dose volume to 1ml in very young offspring. Many avoid vaccinations of any kind early or very late pregnancy.
Because no controlled studies have been performed in camelids to establish optimal vaccination programs , there are innumerable variations in when the vaccines are given. Read about some of them here: 1 , 2, 3
A few New World Camel breeders administer only a yearly tetanus vaccine designed for horses. A veterinarian acquaintance of mine in the Negev Desert tries to give this tetanus booster to dromedary camels prior to his plans to castrate them and always 2 wks subsequent to the operation. That can be hard to do when dealing with nomadic people; easier at the ranches that give camel tours.
Boehringer Ingelheim’s Bar-Vac® CD/T vaccine is one or many that are commonly used in New and Old World camelids in North America and around the world.
Broader Spectrum Clostridium Protection
Intensive agriculture always increases a herd’s risk for infectious disease. Besides maintaining larger than natural numbers of animals in close proximity, natural grazing without supplementation is no longer possible. In those situations, camelids are at increased risk for a number of other fatal clostridial diseases. Neither New World, nor Old World camels have digestive tracts that were designed to handle high protein/high carbohydrate/lower fiber diets. They were designed by the Creator to thrive in marginal areas and under harsher environmental conditions than true ruminants.
Feeding richer diets (high in non-structural carbohydrates=NSCs and protein ) than they would naturally receive (over~ 8% crude protein, over~ 10% NSC) increase the potential for an overly acidic gut and a die-off of the normal protective digestive tract bacteria. In those situations, the small number of potentially toxic clostridial bacteria that are naturally present in camels cam rapidly increase to toxic levels. Short-chopped roughage is also thought to contribute to rumen dysfunction in camelids. As many have said, “a camel is not a cow with a hump” You can read about high NSC forages as they relate to horse health here and here.
Clostridial disease are relatively common among racing and milking camels in the Middle East when the animals are not vaccinated against them. That is probably due to the Arab tradition of giving them dates, clover, honey, and cow’s milk prior to the races as well as feeding milking camels strawberries, dates, other sweets and carrots in an attempt to lessen the “brushy” and salty taste of their milk.
Clostridial problems can usually be avoided by administering a “7” or “8-Way” clostridial vaccine designed for cattle, sheep and goats. Many give an initial vaccination at 3 mo of age, a booster 30 days later, and annual boosters thereafter. Many prefer brands with a reduced, 2ml volume. In New Zealand and Australian Alpaca farming, a “5-Way” is standard. (ref)
Vaccines that are commonly administered include Merck’s Vision 7® with Spur adjuvant or their Covexin® 8 or their Heptavac-P® Plus. There are over 30 pathogenic clostridia – no vaccine can protect against all of them. These formulas differ and the choice your veterinarian makes is based on your herd experience and prior mortality experiences in the immediate area. Some dromedary breeders in the US give the vaccine twice a year – particularly those that include sizable amounts of alfalfa (lucerne) hay and high NSCs in their diets.
It is not unusual to get vaccination site reactions – particularly with the large volume products and epinephrine needs to be close at hand to deal with occasional anaphylactic reactions that occur. Stay with vaccines with a 2ml recommended dose – some are a 5ml dose.
Rabies
The third most common vaccination that Old and New World camels around the world receive is against rabies. Numerous US zoos (including the Detroit Zoo and the National Zoo) administer it to their camels. The 3-4000 camels in Israel are all supposed to receive it and the 14,000 in Jordan as well. In those large camel populations, unvaccinated pariah dogs (unowned village dogs) , jackals and fox are the primary source of the disease. (ref) In North America, the vectors vary with the region. Read more about rabies here.
But in the USA, vaccinations against West Nile Virus probably exceed rabies vaccinations in both new and old world camels.
The initial rabies vaccine dose is often given to camels at 4-6 month of age, repeated at one year and boosted yearly. I know of no rabies vaccines that are approved, labeled or proven effective in camelids. If human exposure to a bite or spit occurs, prior rabies vaccination may not convince public health officials to spare the animal. But Merial/Boehringer Ingelheim ‘s Imrab and Imrab-3 (aka RABISIN®) are commonly used rabies vaccines in Old and New World Camels. Others use various rabies vaccines that are approved for use in cattle and horses.
I have heard rumor that both old and new world camels are slow to develop rabies antibody following an initial vaccination. Many give a booster vaccination 2- 4 weeks after the first in an attempt to develop adequate immunity. I was told that those in Dubai and the UAE get boosted every 6 months.
West Nile Virus WNV
Although the West Nile Virus is present in much of the world, most camelids (and most other hoofstock) simply sero-convert without evidence of disease. Migrating birds spread the virus through mosquitoes. WNV is diagnosed in American llamas from time to time. When a case occurs or when horses or birds in the area become ill with the disease, it is common to vaccinate camelids there as well. But some exotic livestock vets in the USA, automatically include a WNV vaccination in their yearly llama/alpaca vaccination program. The veterinary staff in Irbid, Jordan also vaccinates camels against WNV yearly. Those in Israel, the UAE and Dubai do not. Read more about WNV here.
The most commonly used vaccine for that purpose in North America is Zoetis/Ft. Dodge’s West Nile-Innovator®. Generally, three doses, 3 weeks apart are given but some follow the first injection with only one booster 3-6 weeks later. Others have used Merial’s Recombitek Equine WNV. Yearly boosters are given with both.
It is not uncommon for there to be some post-vaccination swelling at the site of injection and an occasional anaphylactic reaction – so epinephrine needs to be close at hand. Some veterinarians vaccinate pregnant animals, others are reluctant to do so.
No one is sure how long these vaccines protect – the vaccine-induced antibody levels tend to drop rather rapidly.
Equine Herpes Virus-1 & 4 (rhinopneumonits)
Both New and Old World camels are susceptible to these virus. They circulate among horses, so camelids that cohabitate with horses, particularly where equines come-and-go through sale, purchase and travel are most at risk. In those rarer situations, one might consider it in a camelid vaccination health program. Read more about Equine Herpes virus here.
In those situations, or during an equine epidemic, vaccines are often given at 3-6 months of age and boosted 2-3 weeks later and then yearly.
Zoetis’s PNEUMABORT-K® +1b (a killed vaccine) has been a frequent choice in New World camels.
Leptospirosis
As with Equine Herpes-1, leptospirosis vaccine protection is limited to uncommon situations where, for various reasons, management practices can not be modified to reduce exposure to leptospira. The disease has caused abortion in llamas in North America and is known to circulate in Middle Eastern camels (where the primary serotype is L. autumnalis). Cattle vaccines are utilized that incorporate the most common leptospira serotypes found in the region. Immunity may only persist for a limited time and protection may be only partial. (ref) Read more about leptospirosis here.
Combination Livestock Vaccines for Bacterial and Viral Pneumonias and Diarrhea
From time to time, studies identify antibodies in the blood of New and Old World camels that attest to their exposure and recovery from a number of virus that cause disease in domestic hoofstock. These include, IBR (BHV-1), BVD, Adenovirus, Parainfluenza 1,2&3, and bovine respiratory syncytial virus. Possibly, under severe stress and crowding, these organisms could cause disease in camelids. But in most situations, infections appear asymptomatic or, at the most, very mild. If one should attempt to use cattle vaccines against them, killed products, such as Novartis Animal Health’s VIRA SHIELD® 6 or Boehringer Ingelheim’s inactivated-virus Triangle® 9 would be preferred by me over live virus products.
Coronavirus diarrhea
Coronavirus diarrhea has been an occasional problem in young alpacas and lamas in North America. Some veterinarians utilize Zoetis/Pfizer’s Calf-Guard® as well as their Scourguard® 4KC or Novartis’ Scour Bos®4 vaccines in the dames in an attempt to prevent it.
Anthrax
All mammals are susceptible in areas where anthrax persists in the soil. Read about it under bovine animals. If you elect to vaccinate camelids, some report that they can be quite sensitive to anthrax vaccines. (ref) Read more about anthrax here.
Foot and Mouth Disease FMD
This disease is not currently present in North America –so I have no experience with it. I am told that when it affects Old and New World camels, the disease is quite mild. But a veterinarian friend in Beersheba, Israel told me that the National Veterinary Health Service vets there, chase any camels they encounter and vaccinate them against FMD. The vaccine does not necessarily prevent FMD carrier animals from developing. (ref) Read more about FMD here.
I was told that Merial’s FMD product has caused vaccine reactions in Israeli camels.
Equine Encephalitis Eastern and Western
Some camel and lama collections in the United States receive yearly vaccinations against Eastern, Western and Venezuelan encephalitis – most do not. The disease is mosquito-borne, and I suppose that in the midst of an epidemic in local horses, the vaccine may have a use. Zoetis’ WEST NILE-INNOVATOR® + EWT protect against Eastern equine encephalitis , Western equine encephalitis and West Nile virus (WNV) in a single vaccine. Read more about equine encephalitis here.
Colibacillosis
Very young Old and New World camels are susceptible to scours caused by E. coli K99. When the problem occurs repeatedly, diet, sanitation and stress factors need to be examined. Some zoos and camel production/dairy facilities deal with the problem using custom-produced E. coli bacterins and give them to pregnant camels about 8 and then 4 weeks prior to calving.
Colorado Serum Company in the US produces a bovine antibody serum (BOVI-SERA) containing, as one of its many ingredients, antibodies against E. coli K99 for a similar purpose, but I do not know of any veterinarians using the product in camelids.
Wild Horses And Horse-like Animals (equines)
Although donkeys, like the one in the front left of this image, have roamed wild for centuries; they are domestic animals – probably derived from extinct cousins of the Somali wild ass in the center front of the image. (ref) The majestic wild mustang in the top center of the image is also a domesticated animal that found its way back into the wild (a feral horse). The closest living relative of that mustang, and all domesticated horses, is probably the Przewalski’s horse to the top left. (ref) The plains zebra to the lower right is a much more distant relative. (ref)
The ISIS/360 and IUCN believe that there are about 500 Przewalski’s horses housed in zoos and about 325 re-released into the wild. Onagers and khulans in zoos around the world account for about 800 animals with another 1,200 or so remaining free in the wild. Somali wild ass number about 165 in zoos and it is thought that about 570 remain wild in North Africa. One hundred and twenty-four kiangs are known to be kept in zoos with perhaps 50-60,000 left in the wild.
Eons ago, there were a great many species of wild horse-like animals. Today – depending on whom you ask – there are only 7-9. (ref)
Those that remain today are isolated remnants in semi-natural protected pockets or zoos. Other than zebras, they are all highly inbred. The Somali asses in zoos all descend from 17 captured animals, preserving the genetics of perhaps 6-10 founding individuals. It is also uncertain how much crossbreeding with feral domesticated North African donkeys occurred over the years. It was once thought that domestic donkeys descended from these Somali asses. More recent genetic studies make that less likely to be true. (rptref) The onagers, kulans, kiangs and khurs in zoos and Asian reserves are also highly inbred. Przewalski’s horses (takhis) are in a similar state – all descending from 12 captured individuals, some of whom probably had domestic Mongolian pony blood in their heritage.
Wild equid genetics is of interest to veterinarians like myself because in a number of species, genetic bottlenecks (small gene pools/inbred ) are associated with increased disease severity and increased undesirable reactions to vaccines. That is particularly true when vaccines contain living (attenuated/weakened) disease organisms. Decreased breeding success, increase mortality among their offspring and a shorter life span are other negative events that are sometimes associated with small gene pools. Random-bred donkeys and mustangs do not suffer from this problem.
Because of their social nature, free-ranging horse-like animals are also more sensitive to epidemics of disease (epizootics) than more solitary animals. The fact that dominant males collect their female harems from great distances also increases the risk of infectious disease (Przewalski’s horses easily cover 16 to 28 miles to reach water sources in the Gobi desert [ref]) ; the plains zebras, the 150 miles between Namibia and Botswana.
What Vaccinations Might These Horse-like Animals Require?
Many zoos and breeding facilities vaccinate their wild equines with combination vaccines that protect against the same diseases that domestic horses in their area are likely to be exposed to. However, in stable equine animal exhibits in an urban setting, the use of many of those “broad spectrum” multiple-ingredient vaccines are probably unnecessary – something considered in the Evidence-Based immunization philosophy of horse practitioners in many parts of the world. (ref)
In making those decisions, actual risk is one factor. Another is the potential injuries that can be caused when gathering the animals up. That risk depends on animal temperament, facilities design, and staff training. Another is the amount of time and resources available for the task.
Zoos outside of North America are less likely to vaccinate their non-domestic equines (which are primarily zebras). Zooparc de Beauval in France vaccinates based on prior disease experience. They finds no need to vaccinate their Somali asses because they have never experienced the equine diseases for which vaccines exist. I know of several zebra breeding facilities in the United States that also do not give vaccines. In those facilities, it is anti-vaccination sentiments and the potential for vaccine reactions that are the driving reasons.
In situations where the animals can be safely restrained, a vaccination against tetanus is often the only immunization that is given. That is the case at the Helsinki Zoo, The Jerusalem Zoo, the Birmingham Zoo and probably many other facilities around the world.
The next most common vaccination given is probably against western and eastern encephalitis, then West Nile Fever and then, in breeding situations, Equine herpesvirus types 1 and IV. The equine herpesvirus are unlikely to cause illness in the equines (primarily zebras) but animals that are asymptomatic carriers of EHV1 & 4 can spread the infection to non-equine zoo animals in which the virus can be fatal. (ref) (Others have found zebras to be a key conduit for pathogen flow through animal networks [ref]) Some zoos, like the National Zoo in Washington, DC, vaccinate all mammals, including equines, against rabies as well. In 2014, their equine collection consisted of 21 Przewalski’s horses and 6 onagers.
Why Would You Prefer One Vaccine Brand Or Combination Over Another – Aren’t They All USDA/EU–EEA Approved?
When domestic horse vaccines are given to species other than domestic horses, their safety and efficacy in those other species have never been scientifically validated. In those situations, veterinarians generally feel more secure using killed (inactivated) vaccines rather than modified live (attenuated) vaccines. Killed vaccines require ingredients (adjuvants) to boost their effectiveness. Those adjuvant recipes are proprietary. To be patentable, they must be unique. That is probably one reason why some vaccines cause more side effects than others. An alternative to adjuvanted killed vaccines are the newer recombinant vaccines where only a small, non-infectious portion of the equine virus is “grafted” onto virus from another animal species that does not have the capacity to cause illness in horses (replication-defective) (eg ALVAC technology, similar trials have used attenuated Flavivirus chimeras).
Some of these adjuvanted killed equine vaccine were later withdrawn from the market, at least temporarily, (eg MetaStim™) when it was noted that they caused an unacceptably high number of anaphylactic reactions, colic and respiratory distress. (ref1, ref2). The most studied post-vaccination titer variability by brand are for rabies vaccines used in dogs ( read here & ref2) , an Indian study noted that as well. (ref)
The Bureau Of Land Management Vaccination Protocol
As I mentioned, there are no studies that test the effectiveness of horse vaccines administered to non-domestic equines. But the Wild and Free-Roaming Horses and Burros Act of 1971 inadvertently funded the largest free-ranging burro vaccine study in the world. The vaccination program is administered by the BLM to all burros and wild horses gathered by their wranglers and offered to the public for adoption. Their estimated 2014 census was about 8,400 burros and 40,800 mustangs roaming on 42.4 million acres. This same year, 961 burros were gathered up and vaccinated prior to adoption.
Once rounded up and given a health inspection, all burros and mustangs received a single 2ml IM dose of Merial/Boehringer Ingelheim ‘s Imrab® Large Animal rabies vaccine as long as they were 3 month old or older at the time. The first of two IM doses of Boehringer Ingelheim’s inactivated “8-Way” Vetera® GoldXP is also given (protects against Equine Influenza [Clade 1 & Clade 2], Herpes (aka Rhinopneumonitis/ EHV-1 and EHV-4), Eastern & Western Encephalomyelitis, West Nile Virus and Tetanus) They follow that with a booster of the same vaccine about one month later. Burros and mustangs also receive a 1ml, IM dose of Boehringer’s Strepvax ® II, Streptococcus equi /strangles vaccine. If they are still at the facility 6 months later, they get a second booster Strepvax vaccination as well as an additional “8-Way” (this time it is usually Zoetis’ FLUVAC INNOVATOR® that is used).
Vaccine reactions are quite rare. They occasionally see some transient swelling at the injection site in the mustangs – almost never in the burros. On those rare occasions, it is the strangles vaccine that is responsible. There have been no reported vaccine failures.
In prior years, Merck’s PRESTIGE® V with HAVLOGEN® or their ENCEVAC® T with HAVLOGEN® performed satisfactorily for them as well.
ENCEVAC® is a simpler product that would be sufficient in itself for all horse-like animals in many zoos, isolated equine collections and urban settings. It protects against Eastern & Western encephalitis and tetanus. That ingredient style vaccine is used at the Louisville, KY, Henry Doorley NB and Ft. Wayne IN zoos as well as the Fossil Rim Wildlife Center. in Glen Rose, TX, and, I am sure, many other zoos.
But here in Central Texas, a veterinarian aquaintance who services most of the private zebra-raising facilities pretty much duplicates the BLM vaccination protocol. Show donkeys here in Texas receive it as well, with boosters timed to precede shows and exhibitions.
Tetanus
As I mentioned earlier, a tetanus vaccination is the most commonly administered vaccine given to domestic and non-domestic equines. It is particularly desirable to have this protection before castration surgery is contemplated.
Although a single dose is usually protective, two initial doses, given four weeks apart offer more security. The 2012 American Association of Equine Practitioners guideline suggests a 3-dose protocol in foals less than a year of age with the 1st at 4-6 months, again 4-6 wk later and at 10-12 months – then yearly (preferably prepartum). The 1998 AAZV guidelines for non-domestic equines are similar. (ref) Read more about tetanus here.
However, there is no data that confirms that equines need tetanus boosters that frequently (perhaps for 2-3 years after the initial series but certainly not for the entire life of the animal). Studies in humans show that antibody persists at protective level for at least 10 years. In the UK, after the 5th dose of tetanus toxoid, humans are considered immunized for life but veterinarians in the Wales area still suggest horse owners vaccinate their animals every two years. In Australia, the standard among veterinarians is to vaccinate equines every 5 years – but again – that is not based on any published data or the vet’s having seen tetanus cases in previously vaccinated animals. The Zoetis tetanus toxoid marketed in Australia suggests revaccination of horses at 5-year intervals. When sold in the USA, the same product suggests revaccination yearly. Most US horse and zoo veterinarians still give the vaccine yearly. Yearly tetanus vaccination is the case with the Przewalski’s horses and zebras at the National Zoo and Tierpark Hellabrunn (Munich Zoo) as well as the Somali asses and Grant’s zebras at Zoo Basel.
Eastern Western And Venezuelan Equine Encephalomyelitis EEE WEE and VEE
Many zoos in North America vaccinate their non-domestic equines as well as their petting zoo burros yearly against these mosquito-borne virus – generally as ingredients in vaccines with tetanus or as a component in a 5-8 way domestic horse vaccine. It is particularly important to give to zoo stock during times when cases of the disease are being to be reported in horses in the same general area (late spring). Read more about equine encephalitis here.
Not all equine vaccines contain the Venezuelan virus variant – although there is evidence that there is a degree of immunization cross-protection between strains. High antibody levels from these vaccines often do not persist for a full year; but long enough to get the animals through the mosquito season.
Many zoos that vaccinate horse-like animals , give a booster injection 4 weeks after the first. The American Association of Equine Practitioners suggest that equines less than a year old receive a third vaccination in their first year and pregnant mares a booster 4-6 wks prepartum; but the environments of the horse population they attend to is quite different from those on zoological display.
West Nile Virus WNV
This mosquito-borne virus is present in Africa, the Middle East, Southwest and Central Asia, Europe, Australia and, North and South America.
The National Zoo in Washington, DC, the Oregon Zoo, and the Cleveland and Akron OH zoos among many others, vaccinate their equines yearly against West Nile virus – so generally does every zoo in areas that experience West Nile cases in horses, crows, ravens or blue jays within their state. The Bureau of Land Management’s “8-way” vaccine contains West Nile and is given yearly to all burros and horses that can be captured. The vaccine used at the Bronx, St. Louis, Philadelphia and Audubon Zoos when the threat was first appreciated was Zoetis/Ft. Dodge’s WEST NILE-INNOVATOR®.
These vaccines’ efficacy in domestic horses has only been demonstrated for 6 months after a 2-dose initial series. If mosquito season in your area exceeds that, a booster vaccination might be advisable. The American Association of Equine Practitioners recommends a 3-dose series in domestic foals under a year of age. Nothing is known of the effectiveness or optimal dosing schedule in non-domestic equines. We just assume it is similar. I have never been a fan of vaccinating pregnant animals, but some do. Read more about WNV here.
Rabies
It is a good idea to vaccinate equine animals kept in petting and children’s zoo situations where human nips are likely to occur. The same goes for rare non-domestic equines kept in reserve situations – when they can be safely gathered up or shot with pneumatic dart rifles or blowpipes. Some zoos, like the National Zoo in Washington, DC, routinely vaccinate most mammals, including their zebras and Przewalski horses every 3 years with Merial’s Imrab-3 (the product label suggests yearly in horses). The Munich Zoo has vaccinated their Przewalski horses kept in outdoor paddocks against rabies yearly (there is a resident fox population on their 89-acres). The Bureau of Land Management relies on a single 2ml dose of Merial/Boehringer Ingelheim ‘s Imrab- Large Animal rabies vaccine in their burros and mustangs with the suggestion that the adoptees continue at yearly intervals. However the American Association of Equine Practitioners revised their recommendations in 2012 to suggest two injections in colts and unvaccinated adults at 4-6 months and 4-6 weeks later (Merial/Boehringer Ingelheim ‘s large animal and multi-species Imrab formulations do not give that 2-dose instruction on their label. the AAEP is worried that high-titer, recently vaccinated mares might pass antibody to their foals that might lessen the vaccine’s effectiveness). Read more about rabies here.
Equine Herpesviruses Rhinopneumonitis
EHV-1 & EHV-4 are best known, but EHV strains 2, 3, 5 and 9 also exist
One or more of these viruses commonly occur in horse-like animals. Because of their similarities, they have the potential to recombine with one another to form new variant types. (ref)
Once infected, this virus dwells in the animal for the remainder of its life. Many horse-like animals and domestic equines receive the virus from their dames before their immune system is fully developed. A very small number die, considerably more become lifelong, silent carriers of the virus that may again shed infective virus in times of stress. (ref)
EHV-1 variant has been known the longest. It is a problem in the domestic horse industry – particularly in younger horses where it generally causes mild respiratory symptoms. But the virus also has the potential to leave the respiratory tract for the blood stream (become viremic), cause abortion and blood vessel damage (vasculitis) in the nervous system (Equine herpesvirus myeloencephalopathy = [EHM]) and foal death. EHV-4 is more likely to stay confined to the respiratory tract. Strains of EHV virus are also naturally present in the wild zebra herds of Africa. (ref1, ref2, ref3) Read more about equine herpesvirus here.
Although the EHV viruses can, on occasion, cause abortion and disease in stressed non-domestic equines, these animals are given EHV-containing vaccines primarily to protect adjoining non-equine animals in the zoo or park. Infected, zebras, wild asses and burros appear to have a natural resistance to symptomatic EHV disease. However, apparently healthy carrier equine animals have the potential to infect other species kept in close proximity to them. To date (2014) lethal infections of the nervous system due to EHV have occurred in polar and black bear, giraffe, llamas and Thomson’s gazelles (ref) as well as abortion in an Indian rhinoceros. There is no reason to believe that considerably more animal species are not susceptible when kept in close proximity to equines. (ref1, ref2)
All of the animal and human herpes groups of virus share this ability to remain dormant within the body for long periods of time and become contagious again (recrudescent) under stressful conditions or under the stress of coexisting diseases, deficiencies or the weakened immune system of advancing age. Many herpes virus also share the ability to jump species when given the opportunity. In animals that are not the well-adapted natural equine hosts of the virus, the disease they cause is often fatal. Besides EHV, herpes B virus of monkeys is capable of this (ref) – human herpes virus, vice versa. (ref) Human chicken pox virus, another herpes virus, is quite lethal to mice. (ref)
When non-domestic equines are immunized against EHV 1 & 4, a schedule less intensive to that suggested for domestic horses is generally used. (rptref) Weanling foals (4-5 months old) are vaccinated twice at a 4 week interval. Zoos tend to revaccinate yearly, horse breeders more frequently. Those vaccinations usually do increase EHV antibody levels, but the vaccines will not produce complete (“sterile” or absolute ) immunity because the virus has the ability to persist even in the presence of substantial antibodies produced against it. (ref) However it does seem to many veterinarians that when exposed to natural infection, symptoms in vaccinated animals are less severe and – hopefully – the animals less infectious to others. (rptref) Many believe that the effectiveness of EHV vaccines is quite short – perhaps as little as 4 months. The American Association of Equine Practitioners takes a considerably more intensive approach against EHV in the domestic horse industry. (ref1, ref2)
Zoos that use a vaccination program similar to the Bureau of Land Management include this vaccine. It was recently added to the vaccine program of the Salzburg Zoo, the source of the reintroduced Przewalski’s horses in Mongolia (with Merck’s Equilis® Resequin).
Equine Influenza Horse Flu
If you administer one of the common inactivated “8-Way” horse vaccines, the equine will be partially protected against the most common equine influenza virus circulating in North America, Europe and Asia at the time. Equine Influenza is an unlikely occurrence in a well-managed zoo and the disease it causes in domestic horses is usually quite transient (when it occurs in foals, they are more at danger of secondary bacterial pneumonias). So a 3-week quarantine of new animals is the best guard against equine influenza virus entering a facility. Even when vaccinated, the animal’s immunity is often incomplete. (ref1, ref2)
Equine Influenza may, however, pose a more significant threat in non-domestic equines that have small gene pools. In an equine influenza outbreak in a herd of reintroduced Przewalski’s horses, there were considerably more deaths due to secondary pneumonia than there were in the surrounding donkey population. (ref) In these non-domestic horses, the use of Merial/Boehringer Ingelheim ‘s canary-pox vectored equine influenza vaccine may be the better choice. (ref) Again, the vaccination protocols used in most zoos is not as intensive as that recommended by the AAEP for domestic horses. Immunity after a single killed vaccine dose is unlikely to persist more than 6 months. If antigen drift (virus mutation) is occurring rapidly, it is less likely to remain effective. (ref) Read more about horse flu here.
Strangles Streptococcus equi
Vaccination against Strep equi is part of the standard vaccination program for the donkeys and wild domestic horses managed by the US Bureau of Land Management. It might be a prudent vaccine to administer to young non-domestic equines that are subject to transport, recently captured wild stock or in zoo and reserve situations where strangles has a history of frequent occurrence. Two vaccinations are required and the subsequent partial (less severe infections in vaccinated animals are common) immunity takes time to develop. In stable zoo and reserve situations, vaccination is probably unnecessary. Older (>4yrs) equines rarely if ever develop serious cases of strangles. Read more about strangles here.
There are many strains of Streptococcus equi subsp. zooepidemicus. Some are more pathogenic than others. Some consider them to be part of the normal bacterial flora of horses, others do not. The organism has a very wide potential host range including swine, sheep, llamas, cows rabbits, seals and humans. Long-term carrier horses and zebras occur naturally (ref) and can pose a risk to animals in adjoining displays and vice versa.
Of the commonly administered equine vaccines, killed Streptococcus equi bacterin is the most likely to cause reaction site inflammation, occasional cases of anaphylaxis and occasion cases of purpura hemmorrhagica.
Anthrax
Anthrax is a disease that only occurs in areas where soil conditions allow the anthrax bacterial spores to survive. Those areas are known because of cattle mortalities that periodically occur there – usually after floods and periods of inclement weather.
Anthrax disease is primarily a concern among free-ranging African zebra. There have been attempts made to vaccinate them in Kenyan wildlife areas. In 2006, 630+ Grevy’s zebras were vaccinated there against anthrax using dart rifles. A senior keeper from the St. Louis Zoo participated in the project. (ref)
Pregnant animals should not be vaccinated with anthrax vaccine; nor should they be used concurrently with antibiotics. The AAEP suggests a second injection 3-4 weeks after the first. The sole US vaccine supplier (Colorado Serum Co.) also suggests two injections when exposure is likely. The vaccine is quite reactogenic. Read more about anthrax here.
Giraffes and Okapis (giraffids)
ISIS/360, keeps track of the number of giraffe and okapi housed in zoos around the world. As of 2015, they believe that there are approximately 1,300 giraffe in zoos. The IUCN and others estimates the number of giraffe remaining in the wild. They believe there are about 55-80,000 remaining in Africa. Okapi data submitted from various zoos to ISIS/360 accounted for about 176 animals in captivity. Various estimates give the total number remaining in the wild at 10–30,000.
Most European and Australian zoos do not find it necessary to vaccinate their Giraffe or Okapis. That is the case at the Kristiansand Zoo in Norway, Zooparc de Beauval in France, the Vienna and the Budapest Zoos and the Taronga Zoo in suburban Sidney. The London Zoo finds no need to vaccinate its giraffes, but does immunize their okapis with a 10-way clostridial vaccine.
They know that given the right circumstances giraffe are susceptible to various diseases. But over time, they have found that those circumstances do not currently exist at their facilities. I know of one Australian zoo (Werribee Open Range Zoo) that does periodically give their giraffes a 5–Way clostridial vaccine; the Johannesburg zoo “considers” it as well (Merck’s MULTIVAX-P ®). None I know of have ever seen a clostridiosis case in their giraffe.
It is not only the differences in zoo animal husbandry in North America and Europe that influences the decisions on what vaccines their zoo animals receive. General vaccination philosophy differs between Europeans and Americans. Humans also receive considerably more vaccinations in North America than they do in Europe. (ref)
In North America, zoos are considerably more likely to vaccinate their giraffes and okapis. Here, the general philosophy is to vaccinate against known susceptibilities as long as the vaccine is not, in itself, dangerous and the risk of injury to the animal during restraint is minimal. Because that risk is real in giraffes, most American zoo veterinarians reserve periodic vaccinations to the occasions when their giraffes must be restrained chemically or immobilized in a crush for other purposes.
The St. Louis Zoo and Cheyenne Mountain Zoo administers multivalent clostridial vaccines to their giraffes opportunistically. Some, like the Louisville Zoological Gardens and Fossil Rim Wildlife Center give the multivalent clostridial vaccines that include tetanus only to giraffe calves and youngster up to 2 years of age and continue on with only tetanus and rabies booster throughout adulthood. The National Zoo attempts to give a 7-way clostridial vaccine yearly.
A third situation exits: There is now a substantial presence of veterinarians within the extensive systems (free range) and restricted environments of Southern Africa. There, bush veterinarians commonly inject immobilized giraffes with polyvalent clostridial vaccine after they are trapped in bomas for translocation or other required treatment. In cattle anthrax zones, those vaccines are often included as well.
Tetanus
Tetanus protection, either as an individual vaccine product or, more commonly, in a multiple clostridial disease vaccine, is the most common vaccination that captive giraffes and okapis receive. Despite that, reported cases of tetanus in non-vaccinated giraffes are quite rare. One occurred at the Toledo Zoo in 2001 when other horned species (kudu) were inadvertently mixed with giraffe. I know of no other. Read more about tetanus here.
The National Zoo in Washington, Lion Country Safari in Florida, The Miami MetroZoo, Cheyenne Mountain Zoo in Colorado, the Birmingham Alabama Zoo, and most other North American facilities vaccinate their giraffes specifically against tetanus. A few give the vaccine yearly, most opportunistically, but the ACZM suggests a booster tetanus vaccination every two years. (ref) Many zoo veterinarians prefer to give the vaccines “opportunistically” such as when the animals are restrained for transfer, health examination, animal trauma or prior to surgery.
The Enteric Clostridial Diseases
Enteric Clostridial bacteria are part of the normal bacterial flora of all ruminant animals. They only become a problem when diet, stress, management practices, parasitism, injuries or a combination of similar circumstances allow for their uncontrolled growth. Some of those factors are readily avoidable and can be practically reduced in controlled environments. Some are not.
The Importance Of Diet To Managed Giraffe Health And Their Susceptibility to Enteric Clostridial Disease
Diet and the likelihood of clostridial problems go hand in hand.
Giraffes, like all strict browsing animals are difficult to feed properly in zoological collections. One really cannot separate their diet from their potential disease susceptibility and the food composition fed to giraffe and okapi are quite different in American zoos versus zoos in Europe. (ref)
Some consider giraffes to be frail – perhaps because they violate the common mammalian shapes we see around us. But actually, they are quite hardy animals when they are not dietarily challenged or placed under undo stress and have the longest potential life span of all ruminants kept in zoological collections (giraffe up to 38 yrs, okapi 33). (ref)
In all plant-eating species (herbivores), the potential for clostridial diseases (other than tetanus, and C. perfringens/botulinum-contaminated feedstuffs) go hand in hand with proper nutrition. (ref) Giraffe and okapi are browsing animals with habits, digestive system and gastrointestinal microorganisms (ref) quite distinct from grazing ruminants like cattle that rely primarily on grass for their sustenance. Feeding browsing ruminants such as giraffids, moose or duikers in zoos poses a challenge. That is because adequate sources of suitable twig, bud and leaf browse are difficult to obtain. Even when available locally, their collection is very labor intensive. Some European zoos have gone so far as to attempt to silage local browse for their giraffes. (ref) An additional factor is that the tree species browsed in nature contain unique compounds that govern which organisms survive and prosper in the giraffe’s gastrointestinal tract. (ref) Other factors, such as fiber length, chewing and cud time, induced salivation, specific carbohydrate type, and feeding schedules may all interplay.
So giraffe facilities around the world are forced to feed their animals hay products and commercially formulated concentrate products that are only a rough approximation in content and texture (ref1, ref2) of the animal’s natural diet. (ref) These diets and common feeding routines are thought to be the cause of a rather high number of digestive tract problems some of which (acute fore gut acidosis/‘‘peracute mortality syndrome’’) can result in deaths that resemble animals lost to clostridial toxins. Indeed, isolating clostridia from the gastrointestinal tract of giraffes that die acutely is not sufficient to prove that clostridia were the underlying cause of death – clostridial bacteria multiply quickly in moribund and dead animals.
Livestock veterinarians know that in cattle, increased gastrointestinal acidity associated with high carbohydrate/high protein diets stimulate clostridial growth. (ref) Slower developing diet-related problems result as well. (ref). Similar bacterial changes occur in carnivores. (ref) European zoos are more inclined to feed their giraffes basic traditional ingredients. (ref)
Another potential problem with all browsing ruminants in collections is that they are genetically programmed to prefer the choicer, higher energy shoots, buds and flowers over older, coarser tree foliage. Because of that, they are sometimes called “energy concentrate selectors”. In the wild, that is not a problem because those high-energy tidbits are in short supply. But in captive situations, that also makes them prone to consume more concentrates than is healthy for them.
I take the sheer number of articles devoted to this problem is evidence of its importance. You can review these problems and our incomplete understanding of why they occur here: (refs 1, 2, 3, 4, 5, 6, 7, 8, 9)
In the future, perhaps veterinarians and zoo nutritionist will learn to determine the “microbiomic signature” of the resident population of microorganisms within their giraffe and other herbivorous animal’s digestive systems as compared to wild populations as a more accurate way to evaluate the adequacy of the diets they develop. Read about that here: (ref1, rptref2, ref3) There are also recent studies that may give us some added insights into how infections spread through mixed or adjoining animal displays. (ref1, ref2)
The only exposure to clostridial disease in giraffe that most American veterinarians encounter in their training is a slide on pathology quizzes labeled “clostridiosis-giraffe”. No one knows the source of those slides. Rumor has it that the original tissue block resides at the veterinary school in Davis, California with the source long forgotten. My inquiries to a large number of veterinary school necropsy/pathology services did not locate anyone who had ever encountered or heard of a case of clostridia infection in a giraffe or okapi. Searching the records of the Philadelphia zoo as far back as 1921 found no recorded cases. No veterinarians in Australia that I asked had seen a case either. That lead me to believe that perhaps repeated vaccinations against multiple clostridium strains other than tetanus were unnecessary and that veterinarians administer those vaccines opportunistically because there is little or no downside to doing so when the animal is already restrained. After all, it is a ruminant and all veterinarians know that ruminants are susceptible to clostridia.
Giraffe, like all herbivores, probably have normal clostridial flora in their gastrointestinal tract. If some die due to interactions with Clostridia is unclear. But if they can safely restrain the animals, many zoo veterinarians vaccinate them against clostridia as the vaccines appear rather safe.
Those were my thoughts through late 2014 and the American zoological community tended to agree. (rptref1, ref2) The 2015 edition of Fowler’s is not adamant about clostridial disease protection either. Of the 670 giraffe mortalities reported to ISIS/360 in the USA between 1988 and 2005, none specifically identified clostridia as the cause of death; although an occasional diagnosis of colitis or hemorrhagic enteritis was made.(ref)
However, late that year, one veterinarian recalled to me a case of C. perfringens Type A occurring in 2003 in a 15-month-old giraffe calf in a Texas animal drive-through park; then, another vet in Georgia, a possible case of C. sordellii in a giraffe in Idaho in 2010 (although the autopsy results were inconclusive). Later, the director of Dubai’s Central Veterinary Research Laboratory sent a note that they often isolate C. perfringens Type A from necropsied giraffe ”mostly in conjunction with Fat Atrophy”.
And as I mentioned earlier, veterinarians servicing the Southern Africa game farming industry have begun opportunistically administering 10-way clostridial vaccines to giraffe “as an insurance policy”. I do not know whether that change was case-driven, risk-drive, or the natural tendency of private practice veterinarians the world over to utilize all options available to them. They consider “sponssiekte” (gas gangrene/malignant oedema = C. novi aka C. oedematiens) the major threat – subsequent to bruising and penetration wounds sustained in boma capture and the drastic diet changes that accompany penning. Clostridium chauvei has also been isolated. They vaccinate as frequently as annually. The vaccines most frequently mentioned are Merck’s COVEXIN-10® and Bravoxin 10®. Opportunities to give a second booster 6 weeks later are rare, but some do so in controlled environments with fall-out darts.
Giraffe in typical collections should probably receive at least 5-way clostridial protection
periodically when the animals are restrained for other purposes. These vaccines are known to be quite effective in better-studied species. The only known downside is the occasional injection site abscesses that occur (I know that the frequency of injection site abscesses varies considerably between institutions; but I do not know if the individual vaccine formulation or administration procedure is the cause). It is good insurance against a risk whose likelihood is difficult to predict. The desirability goes up considerably when clostridial disease deaths have been confirmed in other ruminant species in the collection, when appropriate browse is in short supply, when animals are subjected to stress or crowding or when the public participates in feeding schemes that are not closely regulated. I am told that there are situations when officials regulating transport between governing entities also demand this vaccination. Some believe that the Giraffe’s normal high feeding habits might limit their exposure to clostridial spores. That is unproven. But individual giraffes, particularly when bored, do increase their curiosity licking at lower levels. Perhaps, animals with that temperament might be at more exposure risk than others – again, unknown.
When environment and husbandry favor clostridia, mortality has a tendency to migrate to clostridia species not included in a vaccine. So the use of the broader spectrum clostridial formulations can be desirable. A single vaccination with any of the clostridial vaccines designed for grazing livestock is not sufficient to provide solid protection. In the farming industry, it is always followed by a booster 3-6 weeks after the first. There is also a considerable lag time in the development of protection. Vaccination late in pregnancy imparts early immunity to the offspring through colostrum but that and booster vaccinations all carry risks to non-domestic, fearful hoofstock that are not present in the domestic livestock for which they were designed.
Rabies
The CDC data banks do not contain any records of rabies occurring in a Giraffe in the United States. Cases do occur very sporadically in wild populations in Kenya and Namibia. (ref) Although unconfirmed, standard rabies vaccines are as likely to be effective in giraffes as in the domestic bovine animals in which they have been tested. So opportunistic or yearly rabies vaccination is wise for giraffes maintained in drive-through parks or in settings where the possibility exists of contact with resident wildlife populations. It is also advisable when programs exist that allow interaction with the public and hand feeding – if only to give comfort to zoo or park visitors. Read more about rabies here.
Yearly rabies vaccination of giraffids is the practice at the National Zoo in Washington, DC, Florida’s Lion Country Safari and Fossil Rim Wildlife Center in Texas. It is encouraged by the AAZA and the AAZV. (ref1, rptef2)
I know of no large animal rabies vaccine that is rated for over a year in livestock. I have been told by the manufacturer that Merial/Boehringer Ingelheim ‘s various injectable rabies lines all contain the same product. So use of their 3-year labeled rabies vaccine in giraffes is quite unlikely to be more beneficial than one labeled to be given annually.
Vaccination Against Neonatal Diarrheas
Coronavirus, Rotavirus and Pathogenic E. coli
Young okapi, and occasionally giraffe, occasionally experience serious and sometimes fatal diarrhea. (ref) Lack of sufficient colostral immunity, passed on from the mother, is thought to be a major contributing factor. Often, more than one pathogen is involved and, as in many diarrhea syndromes, other organisms (like cryptosporidium) can probably play a part as well. (ref1, ref2, ref3, ref4) Adult giraffe are, on occasion, susceptible to similar problems. (ref)
Generally, any or all of these potential pathogens are present in the at-large hoofstock collection but only become a problem when a series of conditions intersect. Since some are unpredictable, some are seasonal and some remain unknown, facilities that experience diarrhea in giraffid pre-adults sometimes use cattle vaccines in addition to husbandry modification in an attempt to thwart the problem. Those vaccines are also more likely to be given when offspring must be bottle-fed. (ref1, ref2)
The two products most frequently utilized are Zoetis’ ScourGuard 4K® and/or Calf-Guard® products. The first product, ScourGuard, an inactive/killed product, has been given to pregnant females, twice – the last dose 4-6 weeks prior to delivery. However, inflammation at the site of injection has occurred.
The second, Calf-Guard®, is given to the offspring by mouth as soon after birth as possible. Some continue vaccination of the young at intervals during the calf’s first 3 months. Others have used the oral, Calf-Guard formula intramuscularly in an attempt to avoid the injection site inflammation often caused by ScourGuard (The London Zoo uses an alternative subcutaneously injected product, Trivacton6 ). Interference with the mother and calf shortly after birth has the potential to interfere with bonding and should be done only after careful consideration of the risks versus the benefits.
Botulism “lamsiekte“
Giraffe, in extensive systems and more controlled environments in Southern Africa occasionally succumb to botulism (Clostridium botulinum). In farms and terrain with a history of prior mortality, giraffes have been vaccinated opportunistically against the disease. Merck’s BOTUVAX® is a brand that has been utilized, although a trivalent Merck product, SUPAVAX®, that also protects against Anthrax and C. novi probably more commonly used. It is unclear how giraffe obtain this toxin. Perhaps due to calcium/phosphate (hydroxylapatite) craving as occurs in local cattle (ref) Read more about botulism here.
Anthrax
Like botulism, anthrax vaccination would only be a consideration in giraffe in extensive systems that overlap known grazing animal anthrax belts or were fed forage obtained from those areas. I would expect it to be even rarer in tree browsing giraffes than land grazing ruminants. In the Kruger and Etosha National parks, it occurs in giraffe considerably less frequently than in the park’s buffalo, kudu and wildebeest. But I do know of one Bloemfontein helicopter vaccination service that incorporates multivalent vaccines with an anthrax component (Merck’s SUPAVAX) into their drop-out dart protocol. Anthrax did, however, kill 11 out of the 44 Rothschild’s giraffes in a 2011 outbreak in eastern Kenya. Subsequent to that mortality, the remaining animals were vaccinated against anthrax with Merck’s BLANTHRAX anthrax/Clostridium chauvoei vaccine. (ref) Read more about anthriax here.
In various parts of the world, giraffids have experienced Bluetongue virus disease, West Nile Fever, Foot And Mouth Disease, Equine Herpesvirus and Leptospirosis. I know of no concerted programs to vaccinate giraffes against any of those organisms – although it might occur in the context of a particular zoological facility or geographical area experiencing an outbreak in their hoof stock.
Pig-Like Animals (suids)
True wild pigs (the Suidae family) are not native to North or South America. Our American equivalents are the peccaries – the common, North American one in the upper right being the javelina or collared peccary, the lower, its South American relative, the Chacoan peccary. Peccaries are smaller than true pigs and members of their own family, Tayassuidae.
All are hearty animals that experience few health problems when housed in zoological collections. Although they are thought to be susceptible to the entire range of infectious diseases of swine (ref), most zoos around the world find no need to vaccinate them against such a broad spectrum of diseases.
When describing the vaccination needs of non-domestic swine and peccaries, various zoo publications suggest that consideration be given to vaccinations against erysipelas, leptospirosis, tetanus, porcine parvovirus, rabies, TGE, atrophic rhinitis, pseudorabies, rota and coronavirus. (eg ref1, ref2) Suggestions are usually given to follow the vaccination protocols used by veterinarians in the pig farms in the zoo’s general area. In typical zoo displays, that is seldom done because the likelihood of an intermingling of hog farms and the zoo’s animal collection is very remote.
Among European zoos, I know that the Copenhagen and Opel zoos do not find it necessary to vaccinate this group of animals. Neither warthogs nor bush pigs (aka red river hogs) are vaccinated at the National Zoological Gardens of South Africa either. In more extensive South African park environments warthogs are rarely restrained for any reason because of their tendency to hyperthermia. (ref)
At the other end of the spectrum, the Duisburg Zoo has an extensive vaccination program in place for its red river hogs (African “bush pigs). Juvenile and adult specimens receive Merck’s Erysorb Parvo® (inactivated porcine parvovirus/ Erysipelothrix vaccine) with annual boosters. Before sows farrow, they are given Boehringer Ingelheim’s Enterisol Coli- Clost® (inactivated E. Coli, Clostridium perfringens vaccine). I do not believe that either vaccine is marketed in the Americas. Merck’s American parvo/Erysipelothrix vaccine also contains lepto. The European formulation is adjuvanted with aluminum hydroxide while Merck’s US product (MaGESTic® 7) uses their patented Spur adjuvant. Enterisol ® marketed by Boehringer in North America is directed against a different organism (Lawsonia intracellularis). European boars housed at the Basel Zoo also receive an extensive vaccination program based on that of commercial Swiss swine.
Here in North America, when non-domestic pig-like animals are vaccinated, it is usually due to the zoo’s general policy of vaccinating all animals within the facility against tetanus and rabies – not because of a particular susceptibility of swine or peccaries. In the case of swine, tetanus is a recognized herd health problem when animals are castrated in less-than-optimal farm operations – something less unlikely to occur in a zoological setting.
Vaccination against rabies and tetanus is the policy for warthogs at Zoo Atlanta. At the National Zoo in Washington, DC, peccaries, receive only a rabies vaccination every three years while at the Toronto Zoo, the red river hogs and warthogs receive vaccinations yearly against rabies and erysipelas.
Canine Distemper And Peccaries
In 1989, an epidemic (nervous system derangement) occurred among wild collared peccaries (javelina) in southern Arizona. Canine distemper virus was subsequently isolated from these animals. (ref) Serum from wild peccaries harvested from 1993 to 1996 detected canine distemper antibodies in 58% of the peccaries, indicating that canine distemper virus was persistently present (endemic) in that population. (ref) A veterinarian acquaintance of mine in Sonora, Mexico told me that sporadic cases were observed there in the wild peccary population that mimicked the outbreak in Arizona. However, virus isolation and CDV titers were not performed.
There was a collaborative program and study through 2016 breeding collard peccaries at the Phoenix Zoo. The offspring, as well as trapped nuisance peccaries, are destined for release in Mexico in an attempt to decrease jaguar and mountain lion predation upon livestock by supplying the cats with alternative food sources. Prior to release, the peccaries are vaccinated against canine distemper and rabies. The vaccine used was Merial’s Purevax ferret distemper vaccine. I do not know how the program is dealing with the current problems we have in obtaining that vaccine.
The canine distemper virus can also infect domestic swine and, perhaps, non-domestic ones as well; but through 2014, I do not believe that overt disease has been reported under natural conditions. (ref) It is unclear yet if the strain of CDV isolated from peccaries circulates in peccaries or if it is a spill-over from domestic and feral dogs. (ref)
Leptospirosis
The feeding habits of swine make them particularly susceptible to leptospirosis when the organism is present in their environment. That is a common situation in commercial swine operations and can be in specific zoo situations as well. When vector control is ineffective or impractical or animals in the zoo’s general animal community maintain positive leptospirosis titers, vaccination of swine and peccaries in the collection is quite appropriate. Peccaries are farmed in Peru. In one study, 64.6% of the animals sampled had positive leptospirosis titer (representing 15 different leptospira serovars). None of the peccaries appeared ill. (ref) In a different study conducted in western Brazil, 46% of the peccaries had positive leptospirosis titers. (ref) Read more about leptospirosis here.
Traditionally, leptospirosis transmission was associated with the presence of rats. Rats still pose a threat. However, in North America, raccoons have probably become a principal vectors of non-arthropod-borne diseases in zoos. In a 2014 study, all of 34 live-trapped raccoons collected in Indiana cultured positive for leptospira. (ref) Feral cats are another novel potential spreader of leptospirosis. (ref) (raccoons are another important carrier of canine distemper virus as well as a parvovirus variant, feral cats a potential spreader of traditionally feline diseases [rptref] and house sparrows of salmonella [ref1, ref2])
Domestic and non-domestic pigs in less controlled settings:
There are zoos and other non-farm setting in which various types of swine are maintained; often in close contact with the public. In those situations, vaccination against a broader range of potential pathogens is wise. A vaccination program developed for miniature pigs would suffice. (ref) In discussions with the author, he mentioned that he considers erysipelas vaccination the most critical – along with periodic rabies vaccination to satisfy the public’s health concerns. Traditional serologic tests cannot reliably identify erysipelas carrier animals although novel methods of doing so are under development. (ref1, ref2 )
Tapirs (ref)
Of all the tapirs, the Malayan or Asian tapir is the most endangered. Less than 2,000 are thought to remain in the wild. Estimates range from 127- 201 in zoos, 49 of which are in the USA. Baird’s tapir has been listed as endangered since 2002. Less than 5,500 are estimated to remain in the wild and only 160 in zoos, about 125 of which are in the USA. The mountain tapir has been listed as endangered since 1994. Less than 2,500 are thought to remain in the wild and only 11 are known of in captivity (5 in Los Angeles, 2 in San Francisco, 2 at Cheyenne Mountain zoo and 2 in Ft. Langley, BC. The common Lowland tapir (aka Brazilian or South American tapir) has the most extensive range. Its total numbers in the wild remain unknown. A 2006 ISIS/360 zoo population estimate was 268 in captivity.
Tapirs tend to have few infectious problems when housed in zoo environments. Their vaccination needs in well-managed display situations remain minimal. In the wild, their solitary nature and low natural population densities make epidemics among them rare to non-existent. (ref1, ref2)
Tapirs are browsing animals; hind gut fermenters that are assumed to have the same disease susceptibility as the other odd-toed ungulates in their family (the perissodactylids), equine animals and rhinoceros. However, although many of the disease organisms that affect horses show evidence that they on occasion multiply in tapirs, there is little evidence that they cause illness in tapirs.
Like all browsers, tapirs prefer sweet, high caloric, low fiber food items when those items are a feeding option in zoos – they have a sweet tooth. And like all browsers, they are prone to digestive tract problems when they receive them in excess. Sugar overload probably accounts for the relatively high incidence of rectal prolapses, intestinal accidents and colic seen in captive (“ex situ”) tapirs. The accompanying changes in gastrointestinal flora probably also account for the occasional opportunistic bacteria and protozoa such as enterococcus, salmonella, pasteurella, campylobacter, giardia and balantidium that are sometimes isolated from sick tapirs that suffer those conditions. (ref1, ref2, ref3)
A similar situation, “grain overload”, occurs in captive moose (ref) and domestic horses that consume these food items in excess. (ref1, ref2) Diets fed to tapirs in captivity commonly contain about one third agricultural fruit. Cultivated fruit that is available to zoos, is considerably higher in sugars (ref) than the fruit that tapirs consume in the wild, and even in the wild, the amount of fruit consumed is restricted and seasonal. (ref) In much of the natural range of the common tapir, fruit of the Mauritia flexuosa palm (aka buriti,aguaje,canangucho) is the most common fruit eaten. That fruit is 46% fiber on a dry weight basis. Pears and apples, in contrast, are only 15% and 21% fiber respectively on a dry weight basis.
Typical pasture hays are probably not an adequate replacement for browse. Browse, available throughout the day, although labor intensive to harvest and supply, probably ought to constitute, at a minimum, about a third of a tapirs diet. Over-feeding of substitute products, perhaps, encourages oral problems such as lumpy jaw (ref1, ref2, ref3) as it does in deer. (ref) However, the resorptive tooth lesions often seen in zoo tapirs appear to affect wild tapirs as well. (ref) Custom vaccines against these opportunistic pathogens are available from Colorado Serum Company, now a division of Merial/Boehringer Ingelheim ‘s, and are extensively used in the deer farming industry. (ref) But management changes are a far better solution. Some tapir specialists theorize that inbreeding in captive tapir populations might also be a contributing factor.
Disease Exposure In The Wild
Evidence of exposure and threat of disease are not the same thing. A recent sampling of wild lowland tapirs in Brazil found antibodies against bluetongue virus, eastern and western equine encephalitis, infectious bovine rhinotracheitis and porcine parvovirus. However, these sampled animals all appeared healthy. (ref)
Blood samples collected in 2007/8 from 27 Baird’s tapirs in display situations in Panama were antibody seropositive for Venezuelan equine encephalitis, Equine herpesvirus 1 and 4, vesicular stomatitis and West Nile virus. Again, no evidence of disease was reported. In both studies, the authors could not guarantee that similar virus were not responsible for cross-reactions. A high exposure rate to leptospirosis appears quite common in native tapir populations – at least in the fragmented and unraveling environments in which they remain. (ref1, rptref2, ref3)
Published Tapir Vaccination Guidelines
Tapir vaccination guidelines usually note that the use of inactivated (killed) vaccines is safer than the use of modified live virus vaccines. That is always the case in non-domestic species in which vaccine trials have not been attempted. Modified live virus vaccines also have the theoretical potential to infect other adjoining or commingled species in which their effect (virulence) is unknown.
Most published guidelines for the zoo industry suggest that tapirs be vaccinated against tetanus and rabies and that one should consider vaccinating them against equine encephalitis, WNV, broad-spectrum clostridial protection, leptospirosis and IBR – based on serological evidence of exposure to any of those agents or, based on diseases occurring in livestock surrounding the zoo or based on mortalities in other herbivorous species within the zoo. The majority of facilities do not do the first, American zoos are the most likely to do the second or third. (ref1, rptref2, rptref3, rptref4, Fowlers8)
Of these diseases, I only know of rabies and tetanus having caused a few mortalities in captive tapirs. Although tapirs are occasionally positive for antibodies against the equine encephalitides, including West Nile, EEE, WEE and VEE, I know of no reports that document any of them being related to tapir illness or mortalities. Never-the-less some zoos find it prudent to vaccinate against them. When they do, it is usually Zoetis/Ft. Dodge’s West Nile Innovator+EWT® that is given because it protects against all of these organisms and tetanus as well. In most species, vaccinations are timed to precede the expected mosquito season. (ref)
Based on a single suspected equine herpes virus loss of a Malaysian tapir (rptref) and, perhaps, a suspicion that equine herpes viruses (rhinotracheitis etc.) might be involved in some way in the corneal cloudiness and keratitis sometimes seen in tapirs, a 2000 publication suggested pre-release vaccination of tapirs with Merck’s equine Prestige II ® multivalent vaccine for its herpes virus (EHV1 & EHV4) protection (ref) (that vaccine has since been reformulated as Prestige® V and Prestige® V + WNV to including Eastern and Western Encephalomyelitis, Tetanus, Flu, Rhino and West Nile virus protection as well.)
Tapir Vaccination Programs At Zoos Around The World
The larger zoos in Argentina, such as Bioparque Temaikèn, vaccinate their tapirs against tetanus. In areas where equine encephalitis is common in horses, multivalent equine encephalitis vaccines are often given as well. I do not know of any of the smaller zoos that range as far north as Belize that vaccinate their tapirs.
Both the National Zoo in Washington, DC and Zoo Atlanta administer only rabies and tetanus vaccinations to their tapirs annually. When the Calgary Zoo had tapirs, they limited vaccination to tetanus and rabies as well.
The Henry Doorley Zoo in Omaha NE has, on occasion, vaccinated its tapirs against West Nile Virus. The perceived threat varies from year to year. (ref) They also vaccinate their tapirs against tetanus and rabies. Lion Country Safari in Loxahatchee, Florida immunizes its tapirs against tetanus, rabies and the Equine encephalitides as well.
The Budapest Zoo does not find it necessary to administer any vaccines to their tapirs at this time; nor do the several smaller UK zoos with which I am acquainted that house tapirs.
Rhinoceros (ref)
Rhinoceros are considered to be most closely related to tapirs, horses and zebras (the odd-toed ungulates) and, as such, veterinarians sometimes vaccinate them against the same set of diseases. To of the 5 rhino species are native to Africa – three to Asia. With a potential weight of 7,920 lbs (3,600 kg) the White Rhino is the second or third heaviest mammal on land. White rhino once roamed most of sub-Saharan Africa. Although census data disagree, today it is thought that there are about 6,487 remaining black rhino world. Black rhinos once numbered over 500-800,000. (1/24/24 update: “I noticed that your article references an outdated stat. You mentioned that there are “5,000” black rhinos left in the world. Based on our most recent data, these figures have been updated, and according to the latest research and data, the number of black rhinos worldwide is more than 6,487. Best Regards, H.P. World Animal Foundation ) In captivity, rhinoceros breeding success has been less than stellar. Indian rhinos (aka Greater One-Horned Rhinos) number about 3,000 in the wild and less than 200 in captivity. Sumatran and Javan rhinos are also critically endangered.
What Vaccinations Might Rhinoceros Require ?
The most recent American zoo guidelines at the time of this writing suggest only periodic (annual) leptospirosis vaccinations for captive rhinoceros. However they suggest that vaccinations against rabies, tetanus, West Nile virus and the other mosquito born encephalitis (ref) be considered when outbreaks of those diseases are occurring within the zoo’s animal collections or in the zoo’s immediate geographical area. (ref)
Leptospirosis
Although all zoo vaccination guidelines that I know of suggest annual or biannual vaccination of rhinoceros against the common large-animal leptospira strains, I believe that very few rhino collections follow that recommendation. There are several reasons: First, restraint of the animals carries its own inherent risk. Second, leptospirosis vaccines are notorious for their side effects (anaphylaxis and abscessation) and third, a degree of doubt that all the illnesses reported as leptospirosis-induced were actually due to the organism. Leptospira are notoriously difficult to culture. It is rare that blood samples are available to detect a rising titer (the gold standard diagnostic test). Leptospirosis vaccines marketed for cattle are known to only produce incomplete, short-term immunity in horses – a distant cousin of the rhino. And fifth, all the tests available to veterinarians today on occasion give false positive as well as false negative results. Non pathogenic leptospira are common in the environment. We do not know how much they contribute to “background noise titer”; nor do we do not know what titers constitute evidence of active leptospirosis infections in rhinoceros or what constitutes protective titers. Read more about leptospirosis here.
No doubt, occasional cases of leptospirosis could occur in captive rhinoceros. But unless a mixed animal collection is plagued by recurrent leptospirosis cases, most collections I am acquainted with do not administer the vaccine.
In stressful situations, rhinoceros can suffer mortality and illnesses that include acute hemolysis, anemia and liver and kidney shut down [aka idiopathic hemorrhagic vasculopathy syndrome (IHVS)]. (rptref)
Those symptoms can also associated with leptospirosis infections. (ref) However, stress, vitamin deficiencies, dietary glucose excess, hypophosphatemia, viral infections, pharmaceutical and chemical compounds, wood preservatives, rodent-control compounds, pesticides, creosote and other wood preservatives, favabeans, oak and maple leaves, wild onions, kale and cleaning agents have all been suggested as possible causes as well.
When leptospirosis vaccine is administered, Zoetis’ LEPTOFERM-5® is a brand that is often mentioned, or a six-way bacterin (with the addition of serovar bratislava). You can read some pertinent article on the subject here: (1, 2, rpt3, 4, 5, 6)
The Equine Encephalitis EEE WEE
Rhinoceros in the United States are occasionally vaccinated against these mosquito-borne diseases. I do not know of any confirmed cases in rhinoceros in North America. (ref) ; although a low titre against Eastern equine encephalitis was once reported (ref).
Some zoos, such as San Antonio and San Diego, have used or considered EE vaccines (or ones in combination with WNV ) at times when cases of either become common in the horse community surrounding them.
West Nile Fever WNV
As with the equine encephalitides, some American zoos immunize their rhinoceros against West Nile Fever. Antibodies against the disease, thought to indicate prior infection, have been found in North American rhinos. (rptref) Whether these rhinoceros are likely to develop clinical disease from the WNV agent remains unknown. When American rhinos are vaccinated against WNV, Merial/Boehringer Ingelheim ‘s Recombitek® Equine is the product most often mentioned. At one time or another, the Cincinnati, San Francisco, Toronto, Calgary and Wilds immunized their rhinos against this disease (ref) Other zoos, like the Henry Doorley, do as well. Zoetis’ West Nile-Innovator WNV vaccine has become less commonly used since one study found that antibody response to it in rhinos was insufficient. (ref) Australian zoo veterinarians (at Dubo) have discussed the possible need to use the same vaccine against the recently-mutated strain of kunjin virus that has sickened horses there. But to my knowledge, as of 2015, no zoos there are giving it to their rhinos. Read more about WNF here.
Tetanus
Many zoos routinely vaccinate all their hoof stock against tetanus – rhinos included. Rhinoceros are not known to be at any greater risk than other fore or hindgut fermentors. A tetanus vaccination is the most common vaccine administered to rhinoceros in the United States. (ref1, rptref2) It is less frequently administered to rhinos in other parts of the world. Taronga zoo did at one time, but decided that restraint risks outweighed the possible benefits. Read more about tetanus here.
The Other Clostridial Diseases
Rhinoceros are browsers – with the exception of the grazing white rhinoceros and Indian rhinoceros (ref) – and as such, are susceptible to the enteric clostridial diseases. How susceptible remains debatable. As in other species, enteric clostridial disease susceptibility is dependent on diet, sanitation and housing circumstances. In zoological collections, it is not uncommon for browsing black rhinos to be feed diets and hay supplements (eg lucerne/alfalfa) more appropriate for grazing animals. On such diets, the microbial populations of the hind gut can be altered allowing opportunistic clostridia to proliferate to toxic levels (ref) or increase susceptibility to other intestinal problems. (ref1, ref2) Read more about the clostridial diseases here.
Until quite recently (2014), management and dietetic changes were the way that enteric clostridial threats were usually managed although vaccination was occasionally resorted to. (ref) RhinocerousHusbandry4.pdf
However, the dynamics of the rhinoceros horn trade appears to be changing that. In 2009, South Africa, by then the only remaining area with large populations of black rhinos, banned internal sale of farmed rhino horn – humanely sawn-off or not. Perhaps as a result, poaching skyrocketed and these unique ranchers were forced to pen their animals (under 24 hour armed guard) at higher-than-natural concentrations and feed supplemental commercial hay. (ref) (Increased wealth within Asian and Middle Eastern populations also drove the increased demand for horn.)
In those penned situations, acute rhinoceros mortality increased. Clostridium novyi and C. chauvoei were isolated from a number of those cases. The natural hind gut flora of rhinoceros is very complex (ref) and I know of no studies that positively established that clostridia – a natural member of the flora of fermenting, plant-eating animals – was the underlying cause of the mortality and not an incidental finding. The South African veterinary community is similarly split on the significance of clostridia in these mortalities. Similar mortalities have occurred in Kenya. (ref1, ref2)
The vaccine most commonly used in rhinoceros in penned and extensive systems in South Africa is Merck’s Covexin10 (unavailable in North America through 2015). Zoetis’ Ultrabac7 has also been used. Both have a high incidence of swelling and abscessation – at least when delivered by dart. (ref) Some are also given a locally-produced C. novei against “swellenhead” [dikkop] ref1, ref2)
Rabies
In the very few instances where rhinoceros are vaccinated against rabies, it is done as a general program throughout the animal collection to re-assure the public or to meet Federal, state local or provincial health codes. (ref)
Rhino-Hippo-Tapir-StandardsJune2013HA1.pdf
(The DelhiZoo did have two recent rabies mortalities in their OHR rhinos and now vaccinates them periodically) Read more about rabies here.
Salmonella
Young rhinos and recently captured and stressed adults occasionally develop intestinal or septicemic (blood borne) forms of salmonellosis due to a variety of salmonella species. (rptref1, ref2, ref3) Apparently healthy individuals carry these organisms as well (~10-12%). (rptref1, ref2, ref3) Under optimal husbandry, these bacteria are kept in check by the other resident bacteria of the rhinoceros’ gut. Read more about salmonella here.
Although vaccines exist for salmonellosis in horses and cattle (and it is known that they can instill cross-strain protection (ref) , I do not know of any instances when they have been administered to rhinoceros. Instead, veterinarians rely on the same treatment and preventative protocols used in horses and cattle. (ref1, ref2) Read my general article on salmonella here.
Anthrax
In extensive systems, where anthrax cases occur in grazing hoofstock (anthrax belts), anthrax has the potential to affect rhinoceros as well. Most experience in the use of commercial cattle vaccines in rhinos pertain to southern and central Africa; but they have been used in rhinoceros populations of Asia and the Indian subcontinent as well. In Southern Africa, Anthrax-containing vaccines are more commonly given to rhinos in Namibia where livestock anthrax losses are common than farther east in the areas near Kruger where mortalities are less common. Chennai’s Arignar Anna Zoological Park vaccinates their rhinos against anthrax as well – as the park sits in an anthrax endemic zone. Some references: ref1, ref2, ref3 Read more about anthrax here.
Asymptomatic evidence (silent infecton without signs of illness) of Other Infectious Agents In Rhinoceros
Surveys of the blood of rhinoceros have found antibodies against numerous livestock virus. Commercial and experimental vaccines exist for many of these virus; but since their ability to produce disease in rhinoceros has not been documented or insufficiently documented, available vaccines against them are not currently administered. They include: EHV-1, (ref) Rift Valley fever, Akabane disease, bluetongue, African horse sickness, epizootic haemorrhagic disease of deer, parainfluenza type 3, bovine herpes-1, bovine viral diarrhea (rptref1, ref2 , ref3),Crimean-Congo hemorrhagic fever (rptref) and , in a study at the San Diego Zoo, hepadnavirus)
Rhinoceros Vaccination Programs At Zoos And Holding Facilities Around The World
In 2014-2015, many zoological facilities do not find the benefit-to-risk equation sufficiently compelling to vaccinate the rhinoceros in their collections. Those include Utah’s Hogle Zoo, San Diego Zoo, Salt Lake City Zoo, Copenhagen Zoo, La Palmyre Zoo, Budapest Zoo, Zoo Zürich, Zoo Basel, Johannesburg Zoo, New Zealand’s Hamilton Zoo, SANParks (Kruger Pk) , SanWild Wildlife Sanct. I do have an acquaintance in Capetown who maintains rhinos in fenced paddocks. He recently experienced sudden mortalities. His veterinarian told me she was considering vaccinating all the rhinos again the clostridial diseases.
Hippopotamus (ref)
I have not found the time to write this section yet based on my notes. AZA members might have access to more current data. The published source is still Murray Fowler’s 1986 publication. Here are some excerpts.
Elephants (ref)
The little rock hyrax on the right is the closest living relative of elephants.
I have not found the time to write this section yet based on my notes. AZA members might have access to more current data. The published source is still Murray Fowler’s 1986 publication. Here are some excerpts.
Giant Pandas (a bear, but a unique one)
The red panda and spectacled bear to the upper right are the giant panda’s closest, but far-distant, relatives. I have not found the time to write this section yet based on my notes. AZA members might have access to more current data. The published source is still Murray Fowler’s 1986 publication. Here are some excerpts.
Seals, Sea Lions And Walrus (pinnipeds)
I have not found the time to write this section yet based on my notes. AZA members might have access to more current data. The published source is still Murray Fowler’s 1986 publication. Here are some excerpts.
Marsupials (ref)
I have not found the time to write this section yet based on my notes. AZA members might have access to more current data. The published source is still Murray Fowler’s 1986 publication. Here are some excerpts.
Bats (chiroptera)
Bats have received vaccinations against rabies. (ref) But I have not found time to write about that yet.
Rodents And Rabbits (rodents and lagamorphs)
I had not found time to write this section yet.
Birds (avians)
# 9 goose can cross the Himalayas flying 3.4-4.5 miles high (ref). Birds with this ability can move avian influenza virus vast distances.
I have not found the time to write this section yet based on my notes. AZA members might have access to more current data. The published source is still Murray Fowler’s 1986 publication. Here are some excerpts.
Dolphins (cetaceans)
I have not found the time to write this section yet based on my notes. Although I did, for a time work for SeaWorld. AZA members might have access to more current data. The published source is still Murray Fowler’s 1986 publication. Here are some excerpts.