What To Know When Your Cat Has Diabetes
Care Of Your Diabetic Cat
Ron Hines DVM PhD
 See How Diabetes Affects My Body
See How Diabetes Affects My Body

Some Information About Your Cat’s Pancreas
Your cat’s pancreas is a small, pinkish organ that is nestled in the folds of its small intestine. You can see it if you enlarge the fanciful image I placed at the top of this webpage. Although it is a quite small organ, the pancreas has two critical functions. The first is to produce the enzymes that allow your cat to digest its food. The second is to produce insulin that regulates how your cat’s body regulates its blood sugar level. That sugar, glucose, is the primary fuel utilized by all animal cells. Most of it is manufactured in your cat’s liver from stored glycogen. The process by which the pancreas regulates your cat’s blood sugar level is actually much more complicated than my explanation. It is not yet fully understood.
There are two distinct portions in the pancreas of all mammals. The one that are important in understanding diabetes occur in small islands scattered throughout the pancreas (the islets of Langerhans). These particular insulin-secreting cells are called β-cells.
What Is Occurring In My Diabetic Cat?
There are several forms of diabetes. But the one affecting your cat is almost certainly the one known as diabetes mellitus which is also called Type 2 diabetes. Perhaps one in 230 cats will develop this type of diabetes. Hardly any will develop the other two types. In type 2 diabetes, cells throughout you cat’s body have lost some of their ability to respond to the insulin that your cat’s pancreas is still producing. In some cases less pancreatic insulin is also being produced. When either occurs, blood glucose sugar can no longer pass from your cat’s blood and into all of it’s other body cells that rely on the glucose in blood for their energy. Your cat’s body is then forced rely on other sources of energy to fuel its cells. It will begin to metabolizes fat and protein with a number of unhealthy consequences.
When that occurs a number of things happen. Your cat’s blood sugar level skyrockets up (hyperglycemia). When your cat’s blood sugar level reaches a very elevated level, some of the excess sugar will spills out through your cat’s kidneys and into its urine (glycosuria).
Veterinarians really do not know how much of this problem is due to decreased effectiveness of insulin in your cat’s body and how much is due to decreased production of insulin by its pancreas. It probably varies from cat to cat just as it does in people. But cat genetics plays a significant roll in their susceptibility to diabetes as well. As a species, felines produce less insulin and respond to it less dramatically than other species do. (read here) Many believe that the reason is that through eons, cats developed as true predators that in the wilds relied on a high protein/low carbohydrate-containing small prey animal diet as their sole food source. That required several basic alterations in their energy metabolism that omnivorous animals and humans do not require.
Why Was It My Cat That Developed Diabetes?
Curiously, as the frequency of Type 2 diabetes has risen in people, it has risen in cats as well. In 1970s, during visits to the veterinary teaching hospital of Purdue University, eight cases were diagnosed per 10,000 cat visits. But by 1999, that number had risen to 124 per 10,000 cat-visits. (read here) I people and cats, suspicion falls on life style. The primary two are increased obesity and decreased exercise. Commercial cat foods are high in carbohydrates. The only reason they are put there is to increase the profit margins those products produce for them. Cats in prior years were often in-and-out cats, rural or barn cats that got plenty of exercise in the pursuit of prey and policing their territory. In those years cats were rarely neutered. Neutering increases the tendency toward obesity. (read here) The risk of developing diabetes is several fold greater for male cats than for female cats – neutered and un-neutered alike. Veterinarians do not know why.
Indoor living decreases cat accidents and disease, but it also decreases exercise and increases the tendency to munch and gain weight.
Just as in humans families, some families (bloodlines) of cats are more prone to diabetes than others. We know that at least one breed of cat, the Burmese, develops more than its fair share of diabetes. (read here) In Australia, Burmese cats are 3.7 times more likely to develop diabetes than non-pedigree cats. In the case of Burmese cats, their post-dining blood triglyceride level remain higher than it should be. (read here)
Is My Cat Too Chubby?
Most cats that develop diabetes are or were overweight. These mellow Garfield cats develop a condition quite similar to the metabolic syndrome of humans, although cats are blessed in not developing the heart and vascular disease that accompanies MS in people.
Obese cats aren’t just rolly-poley and cute. They have much higher fatty compounds ( plasma triglycerides, non-esterified fatty acids and VLDL lipoproteins) in their blood than lean cats. (read here) More importantly, many cat owners do not realize that fat is not just blubber and padding; it is a living organ that secretes compounds called adipokines that directly affect your cat’s pancreas and the cat’s general health. Fat cats are lovable, cute indoor, inactive cats. Besides consuming more calories that they need many are consuming the wrong calories, in the form of carbohydrates – foods they were not designed to consume. (read here)
Adrenal Gland Disease, Steroid Injections And Diabetes In Cats
A few cats are prone to over-active adrenal glands (Cushing’s Disease). It is not nearly as common in cats as it is in dogs, but it does occasionally occur (read here & here) When these glands become over-active due to glandular tumors or over-stimulation by the cat’s pituitary gland, they begin to produce steroid hormones (cortisol) in excessive amounts. One function of this cortisol is to elevate blood sugar. Another is to increase appetite and body weight. That is probably the mechanism by which it encourages diabetes in cats. (read here)
A similar problem can happen when your cat is given a corticosteroid (eg prednisolone, prednisone, dexamethasone, methylprednisolone, etc.) over extended periods of time. These cortisol-like drugs are not produced naturally by your cat’s adrenal glands, but they have the same effect. It is possible that dexamethasone causes higher sugar elevations and insulin resistance than prednisolone – but further studies need to be done to verify that. (read here) Other hormone modulating drugs such as medroxyprogesterone/Depopovera® or megesterol/Megace® can have the same effect in elevating your cat’s risk of developing diabetes. In some cases discontinuing those drugs cures the problem. In some cases it does not.
Pancreatic Amyloidosis
Amyloids are proteins that form in the pancreas of cats as the result of chronic inflammation. Cats, as a species, seem to be particularly susceptible to oxidative damage to their body cells and to chronic, low grade inflammations of many types. You can read about chronic pancreatic inflammation in cats (pancreatitis) here. Triaditis here. IBD here. With time, the processes involved in amyloid formation can also destroy the ß beta cells of a cat’s pancreas. (read here)
Acromegaly – Too Much Growth Hormone
Acromegaly occurs when the adult body produces too much growth hormone (GH). One of the effects of this hormone in adulthood is to decrease the effectiveness of insulin. Cats can develop acromegaly when their pituitary gland develops a tumor. Almost all of the cats in this situation are male. Acromegaly is a condition to consider when your cat does not respond to insulin injections as dramatically as it should (=insulin resistance). (read here, here & here)
What Signs Might I See When My Cat Develops Diabetes?
Diabetes is a disease that usually develops slowly (insidiously) and symptoms do not become obvious until the disease has become quite advanced. So unless your cat gets periodic “wellness” screens, you are unlikely to know of an impending (future) diabetes problem. The most common reason diabetic cats are brought to animal hospitals is because of their owner’s concern that their cat has begun to urinate too frequently and drink too much water (polyuria & polydipsia). At that point, it is your veterinarians job to differentiate between the various common causes – kidney problems, urinary tract infection, or diabetes. There are other things that can cause polyuria and polydipsia. But those three are the most common reasons. In discussions the cat owner often tell me that their cat has recently lost considerable weight. Yet they may also tell me that their cat appears to always be hungry and eating well. These cats often have unkempt, disheveled hair coats. If the diabetes is quite advanced, the cats may be wobbly (ataxic). A few show cataracts in excess of what would be normal for their age.
Emergency Situations When Your Cat Has Had Unrecognized Diabetes For Some Time
If your cat has stopped eating its condition is usually much worse. Those cats are often ketotic due to ketosis (ketoacidosis). I have more to explain about that later in this article. These cat are also prone to have a liver problems called hepatic lipidosis Hepatic lipidosis occurs in cats that have stopped eating for any reason. These cats need to be hospitalized immediately and will likely need intravenous fluids to correct dehydration and adjust the acidity of their blood (pH) back to its normal value. They will probably receive a short-acting insulin as well and have their blood sugar level monitored many times throughout the day. A relatively new drug, Elura® might be helpful to some of these cats in enticing them to eat again on their own. Cats are often not cooperative patients when it comes to eating in unfamiliar environments. If at all possible, stay with your cat to reassure it. Inquire if the faculty offers 24-hour care – not all do. Be your cat’s advocate. Ask if you can periodically bring your cat home and offer its a bit of its familiar food. A number of these cats will be vomiting, retching or experiencing diarrhea that requires medications given by injection. Many have sub-normal body temperatures that require additional external heat. Those cats are not candidates for home treatment.
What Tests And Examinations Will My Vet Run?
In addition to your veterinarian’s physical examination of your cat and your description of the cat’s symptoms and history, your veterinarian will probably run a series of diagnostic tests:
A Blood Glucose Level Test
When your veterinarian suspects that your cat might be diabetic, his/her goal will be to document that your cat’s blood sugar level is persistently above normal. That can be difficult because hospital-related stresses of all kinds often cause cats to have temporarily high blood sugar levels and elevated blood pressure. (read here) The normal fasting blood sugar level in cats is about 70-170 mg/dL of blood. Cats can easily exceed that for a number of reasons other than diabetes.
A Test For the Presence of Sugar In Your Cat’s Urine
Once your cat’s blood sugar level exceeds about 240 mg/dL, its urine also becomes positive for sugar. A simple urine dip-stick, placed in a sample of your cat’s urine, will confirm or refute the presence of sugar. The same dip-stick tests for evidence of a urinary tract infections (nitrite + or -) that sometimes accompany diabetes. (read here)
A Blood Chemistry Profile And A CBC/ WBC Count
It is always wise to do a general health screen on cats that are suspected of having diabetes to judge how the rest of its body is being affected. That includes a series of blood chemistry tests, a red and white blood cell count and a differential blood cell count (aka WBC). It is not uncommon for diabetes to cause , or exist in tandem, with other body illnesses. It is also not uncommon for diseases other than diabetes to cause blood glucose elevation and other signs that could be confused with diabetes. So your veterinarians will want to send blood samples to a laboratory that screen for a large number of abnormalities and disease conditions or run those same test in his/her in house laboratory. You can see what the normal blood values are for your cat here.
A Fructosamine Test
Blood glucose levels are never a continuous flat line. They have many sudden peaks (spikes) and valleys related to your cat’s immediate metabolic needs and stress level. So a blood sugar reading only tell your veterinarian what the blood sugar level was at the instant the blood was withdrawn. However elevated fructosamine, a compound that slowly forms in the blood as blood sugar and certain blood proteins combine, is an much more accurate indicator of persistently high blood sugar levels in your cat. It is similar to the A1c test used to monitor diabetic humans. Fructosamine is quite stable . So the amount of fructosamine in your cat’s blood is a good indicator of its average blood glucose levels over a more extended period of time (1-2 weeks). This test is particularly valuable when your cat’s blood sugar levels are not exceedingly high but are still above where they should be. The fructosamine test has become a standard procedure in cats since 1996. (read here) This test is also quite helpful during your cat’s treatment. It determines if your insulin injection plan is successful in keeping your cat’s blood glucose level in its normal range (glycemic [blood sugar] control). It also tells your veterinarian when it is time to change your cat’s insulin dose or try a different insulin product.
Preparing Your Cat’s Treatment Plan
A diagnosis of diabetes in your cat requires that you and your veterinarian form a close working relationship. Pick one veterinarian that you trust and have good rapport with and request that all follow up appointments be with that same veterinarian. Diabetes is a lifelong challenge. For you to be successful in dealing with it, you need to find a veterinarian whom you trust and whose personal philosophy and practice style matches yours. I wrote an article on choosing the right veterinarian. You can read it here. Not all veterinarians are good communicators. When it comes to surgical skills that is not important. When it comes to diabetes management it is. Many corporate practices are too rushed and scripted. Others pass patients between multiple practitioners. If you don’t feel entirely comfortable with your veterinarian and his/her office staff, keep looking. Ask your friends and pet professions whom they would recommend. Join a support group. There are still plenty of wonderful, supportive veterinarians out there – but it is your job to find them.
Don’t assume that because your cat appears stable, that it does not need continuing checkups. Currently, the safest and most important test to monitor your diabetic cat’s health over time are periodic blood fructosamine assays I mentioned performed twice a year in cat that appear well regulated; more frequently if they don’t. (read here) If you cannot afford all these tests or your cat hates vet hospital visits, you will need to be very faithful, competent and frequent in the use of your cat’s glucometer.
Will Treating My Cat Take A Lot Of Time And Commitment On My Part?
Yes. Not every cat owner is capable or wants to take on this responsibility. Yet many cat owners derive great satisfaction and personal growth from the experience. Cat owners often find that caring for their diabetic pet produces an intense bond and a personal satisfaction that they had not, until then, experienced. Your cat’s basic personality is an important factor too. The decision needs to be a family-wide decision because it will affect all members of your family, your spouse, your children, your co-workers, your other pets. Not only will you have to decide if you will treat your cat. You will have to decide on the level of treatment. These are things that veterinarians were not taught in school to help you with. Some empathetic veterinarians intuitively understand your quandary, others are not equipped to do so.
One worrisome factors for you might to be a difficulty of finding pet-sitters or boarding facilities when you travel. Boarding or strange environments are always stressful to cats. You might loose some of control in your life due to the added responsibility. It might be more difficult interacting with family and friends. Perhaps more worry, less time for social life, added costs and interference with your work life. Probably the least important fact for you to worry about is your ability to perform the procedures that will be involved. None of these procedures are that difficult to master and there are plenty of cat owners and veterinary staff willing to instruct and encourage you. If you live in an isolated area, the Internet is full of instructional videos. Try not to be motivated by guilty feeling that you were in some way responsible for your cat’s diabetes.
People do not thrive in isolation, particularly when they are confronted by illness in those they love. So go find your support network – the people that care about you and your cat. The Web will lead you to many support sites, your veterinarian can tell you of other cat owners facing the same situation with their cat. There are no referees or policemen on the Web. As you educate yourself on the Internet, you will read many conflicting opinions as to what you should or should not do for your cat. You will see advertisements of miraculous diabetes cures and owners who swear that this or that cured their cat. You will even find veterinarians hyping mystical procedures and extracts of rare plants that only grow in isolated valleys of the Himalayas, etc. If it isn’t a proven scientific treatment for diabetes in humans, it is probably valueless for your cat as well. I know how much you love your cat and how much you want this problem to go away. But please, do not believe the claims of folks trying to sell you this stuff. Get your advice from people who do not have something on the shelf to sell to you. A group of veterinarians at the Royal Veterinary College of London wrote a good article on the challenges faced by the owners of diabetic cats. To read it in its entirety ask me for Niessen2010.
What Are My Cat’s Treatment Options?
Your cat will need medications to lower its blood sugar level, dietary modification, exercise encouragement and treatment for any secondary health problems that might arise. Your pet is unlikely to thrive unless all four of these things are attended to. Arranging a low-stress lifestyle with a minimum of changes and interruptions is also quite important for a diabetic cat.
Insulin Injections To Control Your Cat’s Blood Sugar Level
Insulin injection is the underpinning of almost all successful treatment of diabetes. A few cases can be controlled with oral products, but most will require insulin injections now, or later. Orally administered human glucose control medications are also more prone to produce unwanted side effects than correctly administered insulin injections.
Every species of animal produces an insulin that is slightly different in structure from all others. Over the years, veterinarians have been plagued by having to rely on insulins that were designed for use in humans – not cats. An additional major problem has been the withdrawal of insulin products from the market just when veterinarians and owners become comfortable in their use as well as frequent product recalls.
The veterinary insulin market has been chaotic for many years. For many years, veterinarians and cat owners relied on PZI insulin (protamine zinc insulin). It was extracted from freshly slaughtered pig or beef pancreas. It was an effective product for veterinarians to manage cats and dogs suffering from diabetes. However, a lack of sufficient raw material eventually caused that product to be only available intermittently. Another factor that made veterinary PZI insulin difficult to obtain was that human-grade insulin products were also obtained from livestock pancreases. When the major human-grade insulin supplier pharmaceutical companies found that it was more profitable for them to bio-engineer human insulin, plants willing to extract PZI livestock pancreas insulin became unprofitable to operate. The veterinary demand just wasn’t great enough to sustain them.
So, for a period of time, veterinarians had to rely on these bio-engineered products designed for humans with diabetes. They were all less than ideal for keeping your cat or your dog’s blood sugar level stable. However, Merck Animal Health eventually reintroduces a pig pancreas-derived product, Vetsulin®. So did BCP Pharmaceutical, a small Houston, TX manufacture. Their version of PZI comes from cattle pancreas. Idexx laboratories, for a time, also produced a similar insulin product.
Adequate control of your cat’s diabetes requires that one of these long-acting insulins be injected once or, more likely, twice a day. How frequently and in what amount can only be determined on an individual basis. Your veterinarian will begin this titration process at his/her animal hospital. But you will have to fine-tune it at home, based on your cat’s individual glucose curve chart.
Boehringer Ingelheim also produces an insulin marketed for use in cats and dogs. It is called ProZinc®. It is a bio-engineered recombinant human insulin product that mimics human insulin. Some cat owners have found that similar human Lantus/glargine-type products effectively controls blood sugar levels in their cat as well.
Of the two common options, Merck’s Vetsulin® and Boehringer Ingelheim’s ProZinc®, it appears that most cat owners prefer ProZinc® or a human Lantus product. (read here) Some veterinarians report even better success with that human-marketed product than with PZI insulins sold for dogs and cats. (read here & here)
A disadvantage of the Lantus/glargine insulin products marketed for humans is that they are sold in a quite concentrated solution, which should not be diluted. That means that you will be injecting a very small, difficult to measure, amount through your syringe. The advantages are its lower cost and easy availability. Glargine insulin is also available in more expensive pen injectors that minimize the measurement problem. Do not attempt to switch insulin products without your veterinarian being fully informed of what you are doing and be ultra-cautious in any changes you attempt. I do not want your cat to go into hypoglycemic shock. Read the product label and instructions thoroughly as to storage guidelines and do not use products past their expiration dates.
Determining Your Cat’s Correct Insulin Dose:
There are veterinarians and cat owners who feel that you can begin initial insulin injections at home (as an outpatient) if your cat is alert, well hydrated and it is eating and drinking normally. I am not one of them. Most cat owners are inexperienced in the techniques required. Insulin is a very powerful medication and your cat’s responses to it are always somewhat unpredictable. Perhaps I am just a nanny veterinarian who likes to hover over my patients, but I just do not feel comfortable sending inexperienced clients out with a bottle of insulin, a pack of syringes and advice. On the flip side, the advantages of beginning insulin injections in your own home are the lack of hospitalization costs, the fact that some cats really detest being hospitalized and the likelihood that a calm cat at home will give a truer indication of its insulin needs than a stressed cat in an animal hospital setting.
Insulin injections are generally started at twice-a-day intervals – often at 1-2 units per injection. Let your attending veterinarian make that decision. Changes in your cat’s insulin dose always need to be done very slowly and very cautiously. Don’t attempt it when you have multiple life issues to deal with. Always make your injections at the same time of day, at the same time after meals and under the same conditions. Do not make changes near weekends or periods when your veterinarian might not be available.
As Important As The Insulin You Give Is How You Give It
The biggest pitfall in administering insulin is inadvertently giving too much. That can be due to distractions, a new formula or bottle size, or incorrect syringe size. Your veterinarian or his/her technician will demonstrate how and where the injections should be given. Don’t attempt to use syringes designed for one insulin product with a different insulin product until you are absolutely certain the gradations (numbers) on the syringes are accurate for the insulin product you are giving. If you are in doubt, have your pharmacist (not a pharmacy technician) confirm that the syringe and the insulin product are compatible.
How Best To Give The Insulin Injection
As I mentioned, injections should be give shortly after your cat eats and at the same time every day. Giving insulin to fasting cats is more likely to cause dangerous drops in their blood sugar level. Have your vet demonstrate how and/or watch videos on the subject on YouTube. Before you start, feed your cat and give it a few minutes to groom itself. Meanwhile, let the insulin bottle warm up to room temperature. Swirl the bottle around to be sure it is well mixed. Don’t shake the bottle violently. Withdraw the insulin into the syringe to the proper gradation- being careful not to draw in air bubbles. If bubbles appear – gently force the product back into the bottle and try again or tap the syringe with your finger until the bubble rises high enough to be expelled.You may have been holding the bottle at the wrong level or the product may be foamy from excessive agitation. Place the syringe on a clean surface and get your cat. Be sure its claws are not sharp enough to scratch you. Lift up a fold of skin along the cat’s side. Insert the needle almost parallel to the surface of your cat’s skin but angular enough to be certain you are under the skin and not in it (subcutaneous/subdermal not intradermal). If you are in the skin (intradermal), rather than under it, there will be resistance in the syringe when you inject and your cat will tell you by its actions that the injection hurts. Part your cat’s fur to be sure the needle has actually penetrated into the cat and is not just in its fur. If you give the injection properly, your cat will probably not fuss or be aware that the injection was given. Reward your cat by petting and cooing to it. Give it a tiny food treat for its good behavior. Don’t reuse or boil insulin syringes. The needles become dulled, burred and painful and the plungers often leak. Alternate your injection sites. If you inject on the right in the morning, inject on the left side in the afternoon.
Cats can be uncooperative. You will need to tweak and customize these suggestions to fit your cat’s unique disposition. Sneaking up on cats, tricking them or seizing them suddenly in order to give them their injections, tends to be counter productive in the long run. It doesn’t take cats long to learn what you are up to. It is much more productive to use petting, praise and small pungent treats to gain your cat’s cooperation and trust.
What If Insulin Does Not Reliably Keep My Cat’s Blood Sugar In The Normal Range?
The blood sugar level of some cats is harder to control than others. The first thing to do is to be sure that you are really giving the amount of insulin that your veterinarian suggested. The biggest cause of unexpected or poor results is giving the insulin product incorrectly. Be sure your bottle of insulin has not expired and that it has been properly stored.
The next thing to do is to verify that your glucometer is accurate and that you are making your glucose level determinations correctly. The best way to do this is to check your cats blood sugar level on two different meters. Because your cat’s blood glucose level is in constant flux, you will need to do the two meter tests simultaneously or one right after the other. A few cat owners have found that alternative subcutaneous injection sites or having have another experienced person administer the injection, or changing the hour of the injections and feeding schedule solved their problem.
If neither of the above problems are keeping your cat’s blood glucose level elevated your veterinarian will probably increase your cat’s insulin dose. Less commonly, your cat’s blood glucose level will be too low when beginning the theoretically-correct dose of insulin. In that situation the dose size needs to be decreased. Generally, veterinarians begin cats on a low or moderate dose of insulin. That leaves room to adjust the dose upward if need be. If changing your cat’s insulin dose still does not solve the problem, your veterinarian will probably suggest that you try another brand or formulation of insulin.
Insulin Resistance
Calling a cat “insulin resistant” can mean several different things. Using the term in the traditional way means that one believes that the particular cat’s fat, liver and muscle cells no longer respond to circulating insulin as dramatically as they should. (read here). But as frequently, the term is used to mean that a particular cat just requires a larger dose of insulin than one might expect. As a species, cats tend to be insulin resistant in this second way – possibly because they were designed to live on a high protein diet of small prey. If a larger insulin dose or the other things I suggested do not solve the problem, your veterinarian will probably look for other health problems that might be contributing to the resistance. These include chronic inflammations, infections, intercat stress or malnutrition.
Occasionally, what appears to be insulin resistance is due to receiving too large a dose of insulin. This is called rebound hyperglycemia (Somogyi Overswing effect). When it occurs, the cats blood sugar level drops drastically and rapidly after receiving too large a dose of insulin. But the cat’s body quickly releases its own natural cortisone and adrenaline that cause its blood sugar to soon rise to abnormally high levels again. Careful examination of your cat’s blood glucose curve will detect this phenomenon. The treatment is smaller and possibly longer acting insulin doses. The corticosteroid and hormonal medications I mentioned earlier can also make cats resistant to the effects of insulin. Even topical anti-itch and anti-inflammatory spays and creams might have this effect.
Occasional cats just don’t absorb insulin well from their injection sites. A few cats appear to metabolize the insulin too rapidly. Some of these cats respond better to combinations of long and short acting insulin products (not all insulins are safe to combine in the same syringe). I can send you an article on the problem of insulin resistance in cats. Ask me for Scott-Moncrieff.pdf
Check Your Cat’s Blood Glucose Level At Home Regularly
Keeping a close watch on your cat’s blood sugar level at home is the key to keeping your diabetic cat healthy. The best way to do this is for you to purchase and learn to use a hand held glucometer. Most owners obtain their blood sample by nicking the marginal vein on one of their cat’s ears with a sharp lancet. After repeated testing, your cat may come to resent this. But there are other locations from which you can obtain the blood sample, often with less discomfort to your pet. Your cat’s front metacarpal foot pad – the one that doesn’t touch the ground – is a good alternative.
Not all cats will allow you to use the sharp lancets this apparatus requires – but most will. Those that don’t will have to rely on periodic fructosamine testing at their veterinarian’s office or the the services of a house-call veterinarian.
Testing your cat’s urine for sugar spillover is a much less accurate way to keep track of your cats condition because sugar does not enter its urine until its blood sugar level is quite high. But it is a better test than none at all. There are also a cat litter box dressings that will show a color change when sugar is present in your cat’s urine. (Purina ”Glucotest” Feline Urinary Glucose Detection System)
Your Glucometer
At one time most cat owners used glucometers designed for human testing to test their cat’s blood sugar levels. With time more now use meters specifically designed for cats and dogs. What should concern you more than the price of the unit is the price of the test strips. Over time, the strips represent most of your true cost. Cheap strips are also often short-dated.
The problem with using a glucometer designed for human on a cat or a dog is that blood glucose is distributed differently in the blood of humans versus the blood of cats and dogs. In humans, about 58% of the glucose is free in the blood plasma and 42% is tied up in the red blood cells. In cats about 93% of the glucose sugar is in plasma, 7% in the red blood cells (dogs ~ 87.5% of the glucose free in the plasma and only 12.5% in the red blood cells). The way human glucometers are calibrated at the factory, that means that they will likely read a lower blood sugar level than actually exists in your cat. I suggest you purchase a glucometer designed for cat use. However formulas and tables do exist that allow approximate conversion of human meter readings into cat and dog readings.
No matter what brand you buy, check your unit and your strips periodically against the one used by your veterinarian as well against your test solutions. Remember that blood serum and plasma glucose levels run at a lab are often 10-15% higher than results obtained on home meters. The most important attributes to look for in a meter are accuracy and repeatability of the results. A meter that only requires a very small amount of blood is also important. Another important meter feature is that its test strips be very absorbent in drawing up blood from your test prick site (“sipping”). Unless you are uploading your cat’s results to a graph on your computer, additional features that are added to many meters are really an unnecessary complication and expense. Glucometers marketed to the US give their glucose reading in milligrams/deciliter (mg/dL). In the rest of the World, the meters usually display in millimoles/liter (mmol/L). There are websites that will do automatic conversions.
Factors That Affect Your Meter Readings
Cats that are anemic may appear to have higher blood glucose levels than they really have. Cats that are not consuming enough water or are dehydrated will also test higher. Testing after your cat eats a fatty meal can also influence the meter reading as can vitamin C supplements. Other things that commonly cause inaccurate readings are low batteries, expired test strips, insufficient or too much blood on the strip, dirty meters and failure to regularly check your meter’s calibration against the test solutions.
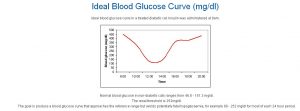
Preparing A Glucose Curve Chart For Your Cat
Enlarge the image above. Persistently high glucose levels take time to do their damage to cats. Occasional spikes are not that important. What is important is that your treatment plan keeps glucose at as close to normal as possible the majority of the time and to keep highs and lows as mild as possible. Use your graph to adjust your cats insulin dose, insulin type, injection interval, diet, exercise plan and lifestyle in a way that keeps your cat’s blood glucose level as stable and close to normal as possible and limit dramatic peaks and valleys (nadirs) as best you can. That was the job of your cat’s pancreas. It’s your job now. When contemplating your cat’s insulin curve, look for trends – not specific points.
Recommendations vary as to how to prepare a glucose curve chart. Curve charts are considerably more accurate when you prepare them at home where your cat is relaxed. I suggest that you obtain the first glucose reading one hour prior to your cat’s morning insulin injection, one hour after the injection and then every hour until the reading has reached its lowest point and begun to rise again. From then on, the sampling can be done every two hours. You should always allow your cat to become accustomed to a particular insulin dose and treatment plan for a few days before attempting to prepare a full glucose curve. You also should be aware that the test might still not be highly accurate. It is hard to get reproducible curves on consecutive days because there is considerable day-to-day, hour-to-hour variability in a cat’s blood sugar level. (read here) There is no one firm figure as to what a cat’s “normal” blood sugar level is because as I mentioned, it is constantly fluctuating. But a value that I often used is 70 – 170 mg/dL, with the average being around 80 mg/dL.
Sometimes the curve you obtain will not mesh with your cat’s clinical picture. Occasionally the curve will indicate that you cat’s glucose is under good control when it isn’t. If your cat continues to drink and urinate excessively or experiences periods of weakness or apathy, rely more on your cat’s fructosamine test results and your intuition rather than the curve.
It is unwise to attempt to maintain your cat’s sugar level near 80 mg/dL. That leaves too little down space between what is normal and what might lead to hypoglycemic shock. Instead, consider an 100 mg/dL – 185 mg/dL average or so as your goal. Some owners of easy-to-regulate cats succeed in keeping their cat’s average blood sugar level a bit lower. But it is not something you should attempt until you are thoroughly comfortable with how your cat is responding to its injections. Many cats can’t achieve that goal and must be satisfied with occasional spike levels of ~ 280 mg/dL. If your cat’s blood sugar reading reach peaks over 180 – 270 mg/dL, sugar will begin to appear in its urine. Cats with persistent readings over 300 mg/dL are at risk of developing health complications. Those cats often have ketone-positive urine. To check your cat’s urine for ketones, it only requires urine dipsticks (eg Ketostix®) available without a prescription. Check your cat’s first urine of the morning. Don’t panic if it is occasionally weakly positive. If it remains so for three or more days in a row, consult your vet.
BE CAUTIOUS WHEN YOU ATTEMPT TO CHANGE YOUR CAT’S INSULIN DOSE. ALWAYS DO SO IN CONSULTATION WITH YOUR VETERINARIAN. GIVE NON-HYPOGLYCEMIC CATS AT LEAST FOUR DAYS BEFORE DECIDING THE TRUE EFFECT OF THE CHANGE YOU MADE AND BEFORE ATTEMPTING ANOTHER CHANGE.
Many cat owners follow the ten percent rule – never changing their cat’s insulin dose by more than 10% in 4 days. Every cat is different. Some cats require more than the typical twice-a-day procedure.
What If My Cat Is Not Eating Normally?
Cats that are not eating adequately react differently to insulin injections than cats that are eating normally. If your cat’s food consumption or weight has fallen off recently, let your veterinarian know immediately. Cats do not have good mechanisms to survive fasting. Unlike you or your dog, they have very poorly developed mechanisms for shifting from regularly-ingested food calories to calories stored within their bodies (glycogen reserves). Cats are exceptionally bad at “shifting gears”. So two problems that develop rapidly in fasting cats are hepatic lipidosis and ketoacidosis – both very serious problems. Read about ketoacidosis here and here. In those situations, your cat eating anything is better than it eating nothing. These cats are usually not drinking enough water either – so soups and broths come in handy. Try to reversing any factors or changes that you may have made that might have led to the problem and contact your veterinarian immediately for advice. If soups, hand or syringe feedings does not rapidly get your cat back to eating normally or if significant weight loss occurs, your cat needs to be hospitalized. A recent addition to medication options, Elura® (The same ingredient that is in Entyce®) is often an effective appetite stimulant. If you have experience giving your diabetic cat Elura® please let me know. Another option is Mirtaz®.
Are There Oral Medicines That Might Substitute For Insulin Injections?
Some cats in the early stages of diabetes can be maintained without insulin injections if they are given oral diabetics medications (sulfonylureas) combined with special diets, weight loss and increased exercise. The most commonly used medication in this class is glipizide (Glucotrol®). Glipizide is not specifically intended for use in cats. It is a rather safe medication – although some cats will vomit or loose their appetite when taking it. Cats taking glipizide should also have their Liver enzymes monitored. If your cat’s blood glucose level has not returned to an acceptable range after taking the medication for four weeks, it will probably be of no benefit to your cat. Alternatives to Glipizide are glimepiride, glyburide and acarbose. (read here)
Both the EveryCat Health Foundation and the Morris Animal Foundation have funded studies to see if the human anti-diabetic drug, pioglitazone, might help control (or perhaps, even prevent) the progression of diabetes in cats as it apparently does in humans. This drug has the potential for very serious side effects. At this time, I would not experiment with it outside of a very controlled veterinary school research study.
Why Is Dietary Therapy In Addition To Insulin So Important?
Diet, exercise, weight control and insulin are the four pillars of successful diabetes treatment. (read here) Cats are creatures of habit. Whenever you make diet changes, do so cautiously and slowly. Make it slowly enough that it is barelynoticeable to your cat. Expect a greater chance for diarrhea and/or colic when transitions are made too fast. When you lower the amount of carbohydrate in your cat’s diet, its required insulin dose might even decrease. Never feed these pets dry cat foods of any kind. Consider preparing a lightly cooked, all-meat diet for your pet at home using a commercial vitamin-mineral supplement such as BalanceIT. 
I try to limit carbohydrates in my cat’s diet to ~ 15% of its energy needs. If you exclude grain, starchy vegetables and organ meats such as liver from a home-cooked feline diet, you will accomplish that. I also avoid pulses (legumes) as there is some thought that they block taurine absorption. Adequate dietary taurine is vital to cats. (read here) It is less clear how added fiber affects cats. Many cats will tolerate up to 8% fiber in their diets without developing loose stools. I avoid commercially available dry cat food formulas for diabetic cats when I can. When fed dry, those foods are too dehydrating. Their only benefit over home-cooked or canned commercial feline diabetic diets is convenience. I believe that these dry diets encourage kidney issues. I prefer chicken, turkey or beef-based diets over fish. The fish products most likely to be in cat food are likely to be the ones unfit for human consumption. Fish the process of spoiling and producing toxic peroxides. (read here) The fish that sat too long onboard or on the dock in the hot sun. I am not a fan of raw diets for your cat either. Cats can become ill from the bacteria that sometimes contaminate raw meat. (read here)
Exercise Contributes To Success
You are unlikely to lower your cat’s weight through exercise alone. For that you will need to control what your cat eats and how much it eats as well. But exercise will certainly help achieving your cat’s ideal weight and exercise has many health benefits beyond weight reduction. Toys, hanging strings, hand-held lasers, etc. are all good ways to encourage your cat to be active. Better yet is a fully-enclosed, outdoor play area (a cat run) or leashed walks with your cat that benefit both of you. It takes cats some time to enjoy walking on a leash. But when they eventually do they love it as much as dogs do. Simply reducing your cats food intake will cause it to be more active and explorative. Exercise also changes the way cells react to insulin. (read here) And studies have found that indoor confinement and inactivity are major risk factors in cats developing diabetes. (read here) Although outdoor, free-roaming cats rarely if ever develop diabetes, I don’t suggest that you allow your cat out-of-doors unattended. There are risks out there that are just as great or greater.
Hypoglycemia – Low Blood Sugar
If your cat’s blood sugar drops too low (less than 45 mg/dL [2.5 mmol/L] ) the cells of its body will be dangerously starved of the energy they need to function. That is what causes hypoglycemic shock. Diabetic cats become hypoglycemic when they receive a dose of insulin that is too large for their current needs (dose too large or, perhaps, did not eat as much as usual). The signs to expect are weakness, drunken motion, and, in severe cases, convulsions and coma. But the symptoms can begin as no more than restlessness, shivering, disorientation and meowing. Some cats react to mild hypoglycemia with ravenous hunger. In mild cases, it may progress no further than that. Hypoglycemia can progress to a life-threatening condition that advances very rapidly. The cure is to raise the cat’s blood sugar level rapidly. If time permits, check your cats blood glucose level with your glucometer. Cats facing this condition should eat if they are willing to or can be coaxed to. Contact your veterinarian, describe the situation and ask for advice. If the situation is already serious, just put the cat in the car and go there now. Your vet’s phone number and that of your nearest emergency clinic should always hang from your refrigerator.
It is wise for all owners of diabetic cats to have a liquid glucose source readily available in their home. You can ask your veterinarian for a 10 cc syringe of 50% Dextrose (5% dextrose (D5W) is too dilute). I make sure all my clients have some around – particularly when they are just beginning or changing insulin doses. You can also go to your pharmacy and purchase some glucose tablets (Dextrosol, B-D glucose tabs, etc.) and dissolve them in warm water (a 1-2-gram/dose should be sufficient). Wait 15 minutes and check the cat’s blood sugar level again. Repeat the dose if need be. Keep unused sugar solutions refrigerated. The best way to give glucose solution to your cat is by wetting the lining of its lips, mouth and tongue with it. Be careful not to get bitten or use a toothbrush to “paint” the syrup around the cat’s oral surfaces. The short period of time your cat’s blood sugar level might be high will have no effect on its long term health. Do not pour or squirt liquid into your cat’s mouth – it is libel to go down wrong. Never place food in the mouth of a cat that is not fully alert. Small, periodic amounts of glucose are better than one large amount. As soon as your cat is willing to eat, allow it to. Keep a close watch on your cat to be sure that the problem does not return. The glucose you gave will only have an effect for a short time and may need to be repeated. Rather than struggle with your cat when it is in a debilitated life threatening condition I would prefer that you just get it to your veterinarian as rapidly as possible. After the incident has passed, re-evaluate your insulin dose, interval and any other factors that might have caused the crisis and correct them if possible. Remember that the glucose curve graph you made for your cat may not have caught blood glucose at its lowest point between blood-draws. If the curve was headed in a downward slope it may have dipped even lower sometime before the next time you drew blood.
Increased Susceptibility To Infections
Urinary tract infections are more likely in diabetic cats – particularly overweight female cats. Diabetic cats are also more susceptible to other infections. It is probably not anything special about the diabetic condition that causes this – just the generalized debility that accompanies advanced or poorly-controlled diabetes. When diabetes is part of a generalized digestive tract inflammatory problem such as chronic pancreatitis or triaditis, an occasional fPL blood test would be prudent.
Do Eye Problems Occur In Cats With Diabetes?
Eye problems and cataracts associated with diabetes are common in dogs and in humans. They almost never occur in cats as the result of diabetes. (read here)
Nerve Problems Associated With Diabetes
Like eye problems, visible nerve problems associated with diabetes are rare in cats. Some vets have seen them; I have not. When this type of nerve damage occurs (diabetic neuropathy) the cats are described as walking on their hocks (plantigrade). But there are reports that even cats with no visible evidence of this type of gait have microscopic evidence of nerve damage. (read here)
Heart Problems Associated With Diabetes
There is no denying that diabetes takes it toll on the body. It is true that the better you control it, the longer your cat will live. But in one English study, veterinarians found that cats with diabetes had a ten-fold increase in developing heart failure over non-diabetic cats during the period that they were observed. One small, subjective study like this does not prove anything, but it suggests a trend.
Hepatic Lipidosis
Cats that feel poorly and refuse to eat have trouble drawing on their stored fat and protein reserves. I mentioned, hepatic lipidosis (aka an enlarged fatty liver = hepatomegaly) earlier in this article. It occurs in any condition that causes cats not to eat. You can read more about hepatic lipidosis and its many causes by following the preceding link.
How Long Is My Cat Likely To Live Now That We Know It Is Diabetic?
How long your cat is likely to live depends on how early the problem is discovered and how well you succeed in controlling your cats blood sugar level. It also depends on your cat’s temperament – some cats are better patients than others.