Liver And Gall Bladder Disease In Your Cat – Cholangiohepatitis – Triaditis – Aka Cholangitis –Triad Disease (CCHS)
Ron Hines DVM PhD
A recent study found that a little over half the mature cats brought to veterinarians because of chronic vomiting, weight loss, and diarrhea, had inflammatory bowel disease (IBD) – alone or as a part of triaditis. In a bit less than half, the problem had progressed to lymphoma. Only intestinal biopsies examined by a veterinary pathologist can tell the difference between the two.
What is Cholangiohepatitis?
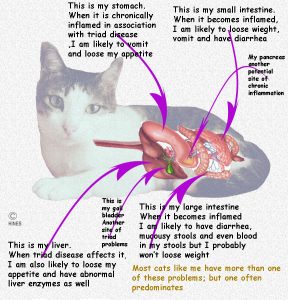
Cholangiohepatitis is a form of chronic liver disease that is common in pampered cats in North America and Europe. It is rare for only the liver to be involved. Next to hepatic lipidosis, it is the most common ailment that our middle-aged cats suffer. (ref) This form of hepatitis centers on structures that convey bile , produced in the liver, into your cat’s gall bladder and on out into its small intestine. That group of structures are the liver’s triad region, hence the names Triaditis or Triad disease. Words that begin with “chole” all relate to bile. When the normal flow of bile is blocked by inflammation of these structures, severe consequences ensue.
Is All Liver Disease In Cats Cholangiohepatitis?
No,
Feline infectious peritonitis (FIP), hepatic lipidosis (The fatty liver disease of fasting cats), liver damage due to medications and chemicals, lymphoma , toxoplasmosis, polycystic liver disease and gallstones all cause liver disease in cats. But cholangiohepatitis and hepatic lipidosis account for the majority of chronic liver and intestinal issues that indoor cats face.
Is There More Than One Form of Cholangiohepatitis in Cats?
Yes.
This disease occurs in three distinct forms and cases that combine the abnormal processes of all three.
The Sudden (acute) Form
The sudden form of cholangiohepatitis is not a common problem. When it does occur, it is often in younger male cats. These cats suddenly stop eating and become depressed. They vomit and often run fevers . Their tummies may be painful and, due to their disinterest in food and water, they quickly become dehydrated and unkempt. After the initial attack, it is common for these cats to develop a yellowish hue to their eyes and gums (jaundice). It is also referred to as the “suppurative” or “neutrophilic” form of cholangiohepatitis/Triaditis because blood
cells generally present to fight bacterial infection flock to the cat’s liver triads. Blood work performed on these cats usually shows elevated liver enzymes, especially bilirubin and high white blood cell count. There is no evidence, that I know of, that these sudden attacks cause the much more common chronic forms of cholangiohepatitis.
The Much More Common Chronic Debilitating Forms That Cats Suffer:
Cats with this form of cholangiohepatitis tend to be older than those with the acute form.
In these cats, the symptoms tend to wax and wane, with relatively good periods interspersed by periods of illness often associated with stress.
This form of cholangiohepatitis can have many names, all dependent on what cells and changes veterinary pathologists see in microscopic samples of your cat’s liver. If defense cells called lymphocytes predominate, they call it Lymphocytic Cholangiohepatitis. If neutrophils predominate, the term is Chronic Neutrophilic Cholangiohepatitis. When other defensive cell, macrophages and plasma cells, predominate, it is called Granulomatous Cholangiohepatitis. The terms used are limited only by the creativity of the pathologists that create them – most cases contain elements of them all. All forms of Cholangiohepatitis can eventually lead to a non-functional, scarred liver. That state is called cirrhosis. You can read a detailed description of the many forms of chronic cholangiohepatitis that occur in cats here.
Do Veterinarians Know Why These Liver Health Problems Occur So Commonly In Cats?
No, we really do not know.
The acute form that occurs suddenly and most commonly in younger cats is often attributed to an infection of bacterial that followed the ducts that link the liver and gall bladder to the cat’s intestines. But there is probably more to this problem than a simple quirk of nature. In humans, acute cholangiohepatitis is known to be related to diet – particularly one that is too high in carbohydrates and too low in proteins and fat. You can read a bit about that here. It is true that bacteria are occasionally found in the bile and livers of cats with cholangiohepatitis (read here) – but bacteria tend to grow in any previously-damaged or distended (enlarged) organ whose circulation has been impaired (damaged) or whose secretion-flow has been halted . In a carefully designed study, bacterial infections were not identified as a cause of chronic cholangiohepatitis in cats. Some veterinarians feel that the fact that the tubes (ducts) linking the cat’s pancreas (pancreatic duct) and the duct (common bile duct) linking the cats gall bladder to its small intestine are so intimately entwined that they predispose cats to these problems. Others find increased levels of antibody (gamma globulins) in many cats with chronic cholangiohepatitis and as well as a positive response to anti-inflammatory corticosteroids as evidence that the disease might be an autoimmune (immune-mediated) phenomenon. There is some evidence that situations like that might occasional occur in dogs (read here), monkeys (read here) mice (read here) and people (read here). But there is no solid evidence that this occurs in cats.
Could My Cat’s Diet Be A Factor?
Yes, it could.
Your cat’s liver is the first stop (portal circulation) for all compounds absorbed from its intestine. By virtue of its position astride the digestive system, it is more subject to injury from any undesirable things your cat eats. The cat food industry has traditionally used ingredients in their diets that were rejected as not fit for human consumption. You can read a bit about that here. These diets, when fed dry, also contain large amounts of preservative with unknown health affects on your cat. You can read about some of those preservatives here. A link between high-iodine in cat foods and hyperthyroidism was discovered. You can read about that here. The source of iodine in cat foods is often from products containing fish parts (but occasional other spoiled ingredients too). Not only are those parts often high in iodine – they are often high in histamine as well – particularly the head and entrails that end up in cat food along with the toxins concentrated in fish’s liver. As fish become stale, their histamine content increases. The first stop for all these compounds after your cat eats them is its liver. Canned fish-flavor cat foods are not immune to this problem. Histamine is not deactivated by the heat of the canning process. However, other potentially toxic compounds like ciguatoxins are not. (read here) These toxins are considerably higher in the entrails that are likely to wind up in cat food. (read here) There is absolutely nothing wrong with occasionally including cooked fish in your cat’s diet. But it should be supermarket fish fillets, not dock discards that you yourself would be unwilling to eat.
What Are The Signs I Might See If My Cat Had Cholangiohepatitis?
The acute, suppurative form of cholangiohepatitis is something you will not miss – a happy cat one day, a sick vomiting kitty the next. But the early signs of chronic cholangiohepatitis are easy to miss or brush off. It might be no more than more picky eating – a cat that has periods where it just sniffs it food, takes a few tentative bites and walks away. Perhaps less tidy grooming. Perhaps days of lethargy and a disinterest in interacting with you. Those signs and weight loss come on very gradually and are easily missed or written off to aging. They can come and go. An occasional cat with this problem actually eats more. That is because they no longer absorb sufficient nutrients from their food and compensate through additional eating. But that extra eating does not result in weight gain.
There is usually no fever in the chronic forms of cholangiohepatitis. Since cholangiohepatitis often coexists with pancreatitis and inflammatory bowel disease, signs of those conditions may be what initially cause you to set an appointment with your veterinarian. Those organs work in tandem – one depending on the others – so problems in one of them lead to problems in the others. In longstanding cases, cats may actually become yellow (jaundiced = icteric); but that is not a common occurrence. Fragile skin has also been reported. (read here)
What Are The Tests My Veterinarian Might Perform To See If Triad Disease Is the Underlying Cause Of My Cat’s Digestive Tract Problems?
A Physical Exam
Your veterinarian will want to perform a thorough physical examination of your cat. Your vet might notice a steady or sporadic drop in your pet’s weight over its previous office visits. In advanced cases , your vet might discover abnormal yellowish skin pigmentation (icterus) or a swollen or painful tummy. But in most cases of cholangiohepatitis; on your initial visit to your veterinarian’s office, your vet’s physical examination of the cat will be normal. That in itself, will help your veterinarian work his or her way to a final diagnosis.
A CBC and Blood Chemistry
Complete blood cell counts (CBC/WBC) and your cat’s blood chemistry values determination are generally a vet’s next step in diagnosing illnesses when vague signs prevail. They are often combined with a laboratory examination of your pet’s urine for abnormalities. (read here) I prefer that samples be sent to a national laboratory. Their equipment tends to be the most accurate and reliable and running tests is all they do. A laboratory-trained staff, more sophisticated apparatus, no distractions like answering phones, surgical responsibilities, and unexpected events to deal with as occur in animal hospital settings. Read about that here and view normal values for many of the tests here.
Your cat’s test results that might indicate a cholangiohepatitis problem or the chronic pancreatic and intestinal inflammatory conditions often linked to it. They include high GGT activity , elevated ALT and alkaline phosphatase (AP) in the presence of normal thyroid hormone levels (T4). Increased bilirubin level increased fTLI test, increased globulin levels, reduced cobalamin and folate levels and abnormal bile acids tolerance studies. No blood value elevations in themselves, are diagnostic for cholangiohepatitis – but they can be quite suggestive of the disease.
Serological Testing
These are the rule-out tests your veterinarian might run for such things as FeLV, FIV, FIP and toxoplasmosis, since they can also account for liver-related symptoms.
Abdominal X-rays
Standard x-rays can give your veterinarian an indication of the size and shape of your cat’s liver, the presence of liver tumors, etc. They cannot rule out or rule in cholangiohepatitis.
An Abdominal Ultrasound Examination
An ultrasound examination, when performed by an expert in its interpretation, can be of considerable help in diagnosing cholangiohepatitis or bile duct obstruction. It is also one of the least traumatic ways to guide a needle through the pet’s abdominal wall and into its liver to obtain a biopsy specimen for pathological examination when they are required.
A Liver Biopsy
The best way to diagnose cholangiohepatitis with certainty is for a veterinary pathologist to microscopically examine small snippets of your pet’s liver. There are two ways to obtain those samples. The cat’s abdomen can be opened surgically (exploratory laparotomy) or samples can be obtained using a long biopsy punch or needle aspirate that is guided through use of a real-time ultrasound image as I mentioned before. The surgical method has the advantage of allowing your veterinarian to visually inspect the entire contents of the pet’s abdomen for abnormalities. The ultrasound-guided method has the advantage of being considerably less traumatic. A second advantage of the surgical approach is that it allows the veterinarian to take full-thickness biopsy samples of your pet’s intestines when concurrent IBD/lymphoma is suspected. As I mentioned, early (small cell/low grade ) intestinal lymphoma cancer and IBD in cats can be quite difficult to tell apart. (read here) Both procedures are not without risk and must be done with the utmost care in cats that are seriously ill because inflamed organs are more likely to leak when manipulated and ill kitties pose a much greater anesthesia risk.
Bacterial Culture of Your Cat’s Liver And Bile
If liver or bile samples are to be obtained for a pathologist’s review, they should probably also be checked for the presence of bacteria. Bacteria are rarely if ever the primary cause of chronic cholangiohepatitis. But if bacteria are present, they need to be addressed with antibiotics.
What Treatments Might Help My Cat?
Stabilization In Life-Threatening Emergencies
If your cat’s cholangiohepatitis has progressed to life-threatening liver failure, your pet will require hospitalization. These seriously ill cats need customized intravenous fluid therapy and monitoring since they are often dehydrated with electrolyte imbalances . They need customized nutritional support – things like feeding tubes, liquid diets and, perhaps, parenteral nutrition. Your cat may need medications to control vomiting. It will also need the good nursing care and attentiveness that the veterinary technicians are trained to provide.
Antibiotics
Veterinarians place many cats with both sudden and chronic cholangiohepatitis on antibiotics. I know I told you that bacteria are seldom if ever the underlying cause of this form of liver disease. But the down side of administering antibiotics is minimal – at least when they are provided for a limited time. Antibiotics also reduce the general bacterial population of your cat’s digestive system which might lessen the workload on your pet’s liver. Some antibiotics, like metronidazole often decrease diarrhea through an – as yet – unknown mechanism. (read here) However although antibiotics may help by reducing the overgrowth of unwanted bacteria in your cat’s digestive tract or specific bacteria in its liver and bile, antibiotics also kill off helpful intestinal flora (“good bacteria”) that your cat requires to maintain good health. In humans fecal transplants are sometimes used to replace these “good” bacteria. (read here & here) It is generally understood these days that a great variety of intestinal organisms are critical for the good health of you and your cat (read here).
Probiotics
Most Probiotic pastes that you see advertised contain, perhaps, four of the 40+ helpful organisms that naturally dwell in your cat’s intestines. They are a very meager “good flora” substitute. Besides, most of the organisms they do contain are destroyed in their passage through the hostile environment of your pet’s stomach. I have little faith in them but they are harmless. The best source of a healthy bacterial is another healthy cat. Co-habitation is all that is required. (read here)
S-adenosylmethionine SAMe (eg Denosyl™)
S-adenosylmethionine is a product officially defined as a “nutraceutical” or food supplement – not a medication. The company that markets it, Nutramax, reports in glowing terms that it is an aid in the repair and protection of damaged canine and feline livers. Articles and testimonials to that are generally provided by the Company’s employees themselves or at Company-sponsored events. (read here) However, independent research on the benefits of SAMe in treating liver damage are less definitive. Some found it no better than a placebo, some found it possibly helpful and a few swore by it. Those that produced the questionable results on its effectiveness were what we call “double blinded” studies in which neither the researchers nor the recipients knew which received SAMe and which received a placebo (sugar pill) and the ones not sponsored by the manufacturers. I do not know if S-adenosylmethionine will be helpful to your cat or not. I hope it will. There are few proven option in slowing the progression of liver disease and I see no harm whatsoever in giving it to cats with cholangiohepatitis.
Choleretics
Choleretics and hydrocholeretics are compounds that facilitate (aid) the passage of bile from its points of production in your cat’s liver to the point of its action as an aid in food digestion within your cat’s intestines. Since bile stasis (lack of movement) appears to be a major part of cholangiohepatitis in cats, anything that encourages bile movement should be helpful. Frequent small meals stimulating the muscles of bile-containing system (biliary system) are one way, but certain compounds are thought aid in bile transport as well. One is ursodiol (ursodeoxycholic acid) , a medication developed to help dissolve human gall stones. It makes bile less viscous (so it flows easier). It is a form of natural bile acid produced in the liver. Your veterinarian might decide that your cat would benefit from this medication indefinitely.
Silymarin (milk thistle)
Like Denosyl® , this is another Nutramax supplement marketed for liver disease in pets. In the Asian market, the Company suggests pet owners take the product as well as their pet. (see here). An NIH study found Silymarin to be of no values in in human chronic liver disease. (read here) as did a second study (read here). Another study found beneficial affects. (read here) I wish I could give you better information than that to make your decisions, but I really can’t tell you more. Like the other products marketed by this company and others reputable sources, there should be no harm in giving it.
Medications that interrupt the inflammatory process
Chronic inflammation is the root of the liver damage seen in long-term cholangiohepatitis in cats. There are medications, steroids and immune-modulators, that act to decrease all forms of chronic inflammation. A side effect of all these medications is a lessening of the animal’s ability to fight infection or destroy tumors in their early stages. Some cats with cholangiohepatitis, inflammatory bowel disease and pancreatitis improve when given these medication. When they are given, they are best given only intermittently and for relatively short periods of time during which the cat’s blood work and general condition are closely monitored by your veterinarian for unwanted side effects. These medications include corticosteroids like prednisolone and drugs developed to fight cancer such as chlorambucil, cyclosporin. and methotrexate. Because the effects of these medications is non-selective in which portions of your cat’s immune response they suppress, none can be given without risk. (read here) But then, no truly effective medication can be given without some risk of side effects. Being watchful for them in your cat is one of the most important jobs for you and your veterinarian.
Vitamin And Nutrient Support
Cat that aren’t eating aren’t receiving important vitamins and nutrients. So supplying them independent of a quality diet is a good idea. The nutrient-absorbing ability of cats with cholangiohepatitis is reduced. The diseases cripples a cat’s ability to absorb vitamins and other important nutrients through its intestines even when those compounds are present in recommended amounts. So, at least initially, some of these compounds are best given by injection – if that is an option. They include, vitamin K, E and B-12. Some veterinarians also suggest taurine, folate and L-carnitine supplements. (Your veterinarian might just administer a vitamin supplement – there is no harm in doing that. Or he/she might confirm a B-12 deficiency exists by ordering a serum cobalamin assay. Deficient cats often perk up when that vitamin is supplied.
What About Giving My Cat Stuff I See Marketed On The Internet?
Be very cautious about giving you cat these products. Glowing testimonials are a good warning sign. Be even more cautious about expecting them to actually work or to be a substitute for a required visit to your veterinarian. If you are fortunate, they will not harm your cat. It is impossible to know what these preparations actually contain or how they will affect the medications your veterinarian may have already dispensed to your cat. (read here)
Might Modifying My Cat’s Diet Help?
Yes
A low carbohydrate high protein, highly digestible diet, given in many small amounts during the day, is known to be beneficial in liver disease treatment. Diets that contain sucrose or corn syrup fructose,or large amounts of carbohydrates are undesirable. It is also know that increased dietary protein levels reduce certain liver/bile related problems in humans. As important as what you feed is when you feed. Multiple, small feedings, given throughout the day, are more likely to encourage healthy bile flow than one or two larger ones.
The only caution in feeding a high protein diet is in cats with very advanced liver disease in which the liver has lost its ability to rid the body of ammonia. I mentioned this problem, hepatic encephalopathy, earlier in this article. In those situations, where a cat’s blood ammonia (hyperammonemia) levels are elevated above normal, your cat’s protein intake (the source of much of this ammonia) needs to be closely regulated.
Is There Anything I Can Do To Prevent This Problem?
Feed you cat a diet less likely to contribute to the problem is the only thing I know of. Cats are true carnivores – something pet food companies do not want you to accept. The higher profits generated encourage pet food companies to including cheaper ingredients of less-than-first-class quality. Over time, that is likely to have negative effects on your cat’s long-term health. So is adding ingredients that appeal to your taste and eye appeal (such as vegetables and peas) but that are not normally eaten by cats. Preparing your cat’s diet yourself from supermarket ingredients is what I suggest. (read here)
What Is The Long Term Outlook For My Cat?
The liver is an organ that repairs itself well when faced with a sudden crisis that still leaves a portion of its cells (hepatocytes) intact. The liver is not nearly as efficient in recovering from sustained, long-term, damage (scaring) – even when the initial cause is corrected. So cats with the acute suppurative form of cholangiohepatitis are usually cured rapidly or lost to this World. The majority of the people reading this article are the owners of cats with the more common chronic form of cholangiohepatitis. Making modifications to those cat’s life style and diet, along with periodic veterinary attention, should allow your cat to continue a happy life in spite of chronic cholangiohepatitis. Never expect it to be fully cured, but expect its condition to markedly improve with periodic flare ups associated with stress.
The outlook for cats is less bright when the problems is only discovered in its advanced stages, when multiple systems are affected by chronic inflammation, or when the problem has advanced to the early stages of leukemia (lymphoma). We know that chronic stimulation of your cat’s lymphocyte populations can be the first step on a road to lymphocytic cancer (lymphoma). Sometimes, your vet must actually have the properties of these lymphocytes analyzed to decide how far along in that process things might have progressed. Not all cases of lymphoma progress rapidly. (read here)
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.