Ron Hines DVM PhD
 For the newest mange treatment options go here
For the newest mange treatment options go here
What Causes Demodectic Mange In My Dog?
The two most common causes of mange in dogs are the demodectic mange and the sarcoptic mange mite parasites. Cats can develop mange too, but the most common mange in cats are due to the notoedric mange mite, sarcoptic mange or two more recently discovered feline species of demodectic mange that you can read about here and here. Any pet with a weakened immune system is more likely to develop a severe case of any of these parasites. Dog breeds with wrinkly skin are more susceptible to demodectic mange as well.
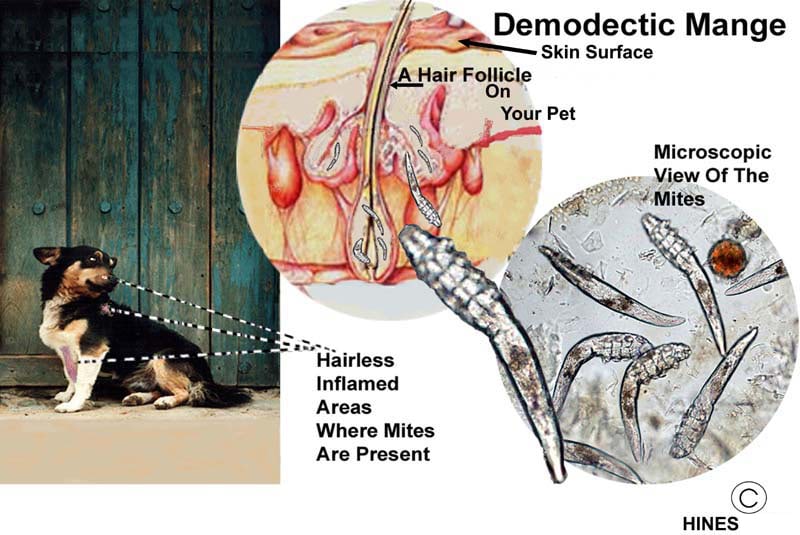
Demodectic mange is also called red mange or demodicosis. The parasite responsible for most cases is Demodex canis – the ones in the illustration on the top of this page. But Demodex injai and D. cornei can also cause similar skin problems in dogs. For reasons unknown, Demodex injai has been found most commonly in terriers. In those breeds, it causes an excessively oily, musty coat (seborrheic dermatitis) – particularly along the pet’s spine. Hair loss is minimal. This cousin of D. canis resides mostly in the oil glands (sebaceous glands) found in your dog’s skin. Demodex canis, the more common one, lives primarily in your dog’s hair follicles. Unlike fleas and ticks, all species of demodex spend their entire lifetime on your dog.
Can I Catch Demodectic Mange From My Dog?
Probably not. There has only been one case where that was suggested, and that Turkish case was not well verified. (read here) The Wikipedia entry states that people with weakened immune systems are at risk of contracting demodex canis and that human demodectic mites can be transferred to dogs that are immunosuppressed. However, the Wikipedia author(s) cite no references for that statement and I find none in Pubmed either – apart from the one Turkish case I mentioned. Your immune system is the watchman at the gate, and it sometimes malfunctions, so I would call it perhaps possible, but certainly not proven or likely.
For sarcoptic mange (itchy mange), it is an entirely different story. That mite will cause itching and redness when it gets on people. However, on people, sarcoptic mites obtained from dogs, cats, or wildlife are not believed to be able to survive long term or to reproduce. So, they usually “self cure” in 14–21 days. Much quicker with the same medications used for lice. The “Seven Year Itch” in people is caused by a different mite.
How Did My Dog Catch Demodectic Mange?
Most veterinarians believe that Demodex canis is found in the skin of all, or almost all, normal dogs. But the number of mites present in your dog’s skin is kept low by its natural immune defenses (its innate immune system). Too low a number to cause disease. We also believe that puppies become contaminated with these mites shortly after birth while they nurse and snuggle with their mother who already harbors a population of these mites in her skin. (read here) That might leave some of you wondering why some dogs develop demodectic mange hair loss and skin inflammation and some don’t. We know that the juvenile (puppy) form of demodectic mange often cures itself after a period of a month or so as the dog’s immune system learns to recognize the mites’ presence and destroy them. Age-related immunity is known to neutralize numerous other parasites as your pet’s immune system matures and becomes more sophisticated in its abilities. (read here)
As I mentioned, dogs differ genetically in their immune system’s ability to locate and destroy demodectic mites. The most susceptible are breeds that were intentionally bred to have abnormally wrinkly skin and skin folds. They include shar-pei, English bulldogs, some pit bulls, pugs, and Staffordshire terriers. Dogs with short hair coats also seem more susceptible to mange than breeds with longer hair coats. The few studies that attempt to explain the underlying reasons certain dog breeds have loose wrinkly skin were all focused on the shar-pei breed. Their wrinkles are attributed to a genetically driven excess of hyaluronic acid within their skin. HA is one of the glycosaminoglycans – the same compounds your veterinarian sells as a nutritional aid for arthritis and joint problems. (read here) On a practical note, when I administer vaccines to these mange-susceptible wrinkly breeds, the hypodermic needle penetrates their skin with no resistance – as if it were butter. That is because their skin is deficient in collagen. In its wisdom, the AKC has managed to create dogs with the equivalent of EDS. That same chromosome also contains genes that are essential to your pet’s T-cell function which normally destroys demodectic mange mites.
Is My Dog’s Age Important?
Yes
It is quite uncommon for demodectic mange to suddenly appear in a mature, otherwise healthy dog. When it does occur in a mature dog, an underlying health issue or medication has probably weakened your pet’s immune defenses. Systemic diseases, such as Cushing’s disease, have been the underlying cause of reduced immunity to demodectic mange through the elevated release of cortisol. Through the same mechanism, high prolonged doses of corticosteroids such as prednisone and prednisolone can be the cause as well. The generalized malaise and debility that accompany many serious health issues have also been known to be a factor. When a dog over 1.5 years of age suddenly develops demodectic mange, a series of tests are necessary to attempt to locate its underlying health issue(s). Similar human cases of the human demodectic mite occur in people with suppressed immune systems or those who are forced to take powerful immunosuppressive medications such as cyclosporin, methotrexate, or azathioprine. I also received an email from a dog owner whose 12-year-old pet developed demodectic mange shortly after beginning Apoquel® – another immunosuppressive medication.
If My Dog Has Demodectic Mange, What Signs Will I See?
Dogs commonly come to their veterinarians with two different forms of demodectic mange:
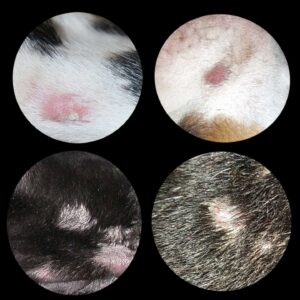
Localized Demodectic Mange
The first and most common form, localized demodectic mange, usually occurs in dogs that are less than 1.5 years old. Dog Owners, or their veterinarians, notice one or two coin-size patches of thin or missing hair on the pet’s face or, occasionally, on its neck, legs, or trunk. It is rare for these little patches to be inflamed or itchy. The patches are quite distinctive – similar to the one in my illustration above. Dog owners often mistake them for ringworm. About Ninety percent of these localized cases resolve on their own in a month or two with or without treatment. But in approximately ten percent of the cases, mite numbers are not kept under control and go on to colonize much of your pet’s skin in large numbers. Those pets have developed generalized demodectic mange. This unfortunate situation is more likely to occur in dogs whose parents or bloodline (close relatives) previously experienced this same form of mange. Even if cured by your veterinarian, it is never wise to breed these pets.
Generalized Demodectic Mange
The second group of dogs have generalized mange that involves many areas of their body. These dogs have sparse or patchy hair coats. Their skin is often overly pigmented and thickened. They have a musty, unhealthy odor. Many have waxy ear infections (ceruminous otitis) due to changes in the bacterial and yeast flora of their ear canals (be sure they are also checked for ear mites). Some dogs with generalized demodectic mange itch and scratch. When they do, it is usually due to a secondary bacterial staph and/or skin fungal infection that also needs treatment – or flea bite sensitivities. The superficial regional lymph nodes of those pets are often enlarged. They may also run a low fever and often appear listless, ill, and depressed. Occasionally, dogs develop demodectic mange that is confined to their feet and paws. When that occurs, the paws become puffy, malodorous and raw due to secondary bacterial infections. These cases can be very stubborn and resistant to treatment. Shar peis, bulldogs and other wrinkly breeds are over-represented in all forms of adult demodectic mange, including the paw form.
How Will My Veterinarian Confirm That Demodectic Mange Is My Pet’s Problem?
When your veterinarian is suspicious that your dog might have demodectic mange, he/she will place a drop or two of mineral oil on the area. The next step is to scrap the lesion(s) with a scalpel blade and then place the mixture onto a microscope slide to confirm that mites can be seen microscopically. Scotch Tape™, pressed firmly against your pet’s skin, and then examined under a microscope can sometimes detect these mites as well. I have also found demodectic (and sarcoptic) mange mites or their eggs in microscopically examined stool samples. Those pets ingested the mites while grooming. However, remember that normal dogs also carry lower numbers of mites that might be ingested during grooming.
If the lesions (hairless or crusty areas) are confined to sensitive areas of the face, microscopic examination of the roots of plucked hairs immersed in lens oil is often sufficient to find the parasites. Blades near the eyes of awake dogs are never a good idea. When your pet’s inner ear flaps are the only areas affected, Q-tip™ swabs can be the sample source. When secondary skin disease is severe, or when mange has been present for long periods, these mites can be hard to locate. In those cases, skin biopsies usually find them.
Are There Other Skin Problems That Might Be Confused With Demodectic Mange?
Yes
Other medical conditions that cause inflammation of your pet’s hair follicles and skin or itching can produce signs somewhat similar to those of demodectic mange. They include food allergies, atopic dermatitis, staphylococcal infections, skin fungus/yeast infections, various autoimmune diseases or long-standing cases of sarcoptic mange when only a few sarcoptic mange mites are still present. A skin scraping that is positive for an abnormally large quantity of demodectic mites, confirms the diagnosis of demodectic mange. If no mites are found, your veterinarian might tests for those other possible causes. A number of dogs suffer from more than one of these problems simultaneously – particularly ownerless, nutritionally deprived and parasitized dogs.
How Will My Veterinarian And I Know If We Are Making Progress?
Your veterinarian may do periodic skin scrapings (~every 2–4 weeks) during treatment to judge your dog’s speed of recovery. During those examinations, your vet will be looking for immature mites – a sign that the mites are still active and breeding. Large numbers of dead mites are a sign that the treatment is working (even immersed in mineral oil, living mites still slowly flex and wiggle). A decrease in total mite numbers is also a very good sign. Two consecutive examinations that find no dead or living mites is evidence that your pet is on its way to a cure. A third negative examination is prudent about a month after treatment ceases to be sure the cure was permanent.
What Medications Cure Demodectic Mange?
Veterinarians once used a number of medications attempting to cure demodectic mange. All of them had their drawbacks. However, with the availability of topical and oral Isoxazoline medications such as NexGard®, Bravecto®, Simparica®, Credelio®, or the application of Moxidectin containing dog topicals such as Advantage Multi®/Advocate®, those older treatments are rarely used today. (read here) Check with your veterinarian, read the label and read about breed sensitivities before attempting to apply these products to debilitated animals.
Bravecto® was not 100% effective in curing demodectic mange when given for a single month. (read here) Another study found afoxolaner/NexGard® about equal in its ability to destroy demodectic mange mites. (read here) That study claimed that NexGard® was superior to the topical moxidectin/imidacloprid product, Advantage Multi®, that I mentioned. Take all published studies that were paid for by specific manufacturers with a grain of salt – miraculously they always discover that their product is more effective than the competition’s.
Moxidectin is a compound similar to ivermectin. Its chief advantage is that it persists in the blood stream of most dogs for a full 30 days, while ivermectin/Heartgard® rarely persists in your dog’s body longer than 15 days. (read here & here) Although moxidectin is only approved for the treatment of sarcoptic mange in the United States, it is approved for use in treating demodectic mange in Canada and Europe.
As I mentioned, young dogs with no more than four isolated small patches of mites generally get better without treatment. However, when the number of patches continue to increase in number or size, it is wise to begin treatment.
 Here Are Products Commonly Used In The Past:
Here Are Products Commonly Used In The Past:

Rotenone (aka derris root), a constituent of Goodwinol™, is a natural product obtained from the roots of several tropical and semitropical plants. Its main use today is in organic farming. Rotenone-containing ointments, such as Goodwinol®, are usually effective when applied to isolated small demodectic mange areas. However, it is impossible to know if it was the medication or the simple passage of time that effected the cure.
Amitraz-containing formulas (e.g., Mitaban®) were once the only FDA-approved medications for both small patches and more extensive cases of demodectic mange in dogs. The drug was too powerful for use in cats. However, amitraz is smelly, messy, hard to apply and prone to side effects in some dogs. Wear gloves and a face shield if you are attempting to use this product yourself. It is hard to apply correctly without getting a considerable quantity of the milky smelly dip on your cloth and body in the process. Plan to take an immediate bath. Follow the directions on the bottle and remember, if the dip does not penetrate deep enough to reach each mite it will not kill them. Better yet, let your veterinarian’s experienced staff perform these dips. (read here) These dips are generally done at veterinary hospitals at 7-14-day intervals. Dips are continued until no living mites are found on skin scrapings. When Amitraz does not cure dogs at the manufacturer’s FDA-suggested dose, veterinarians sometimes resort to increasing the dip concentration or frequency. I no longer use these products because of the better and safer options I already mentioned. Although not a labeled use, and while wearing gloves, in the past I used this product on small isolated patches of demodectic mange as a “rub-in”— well massaged into the areas. The dogs all heal. But just like Goodwinol®, one cannot say that they wouldn’t have cured themselves with simple “tincture of time”.

Heartgard® and its generic equivalents contain, ivermectin. Although it can take a considerable period of time, ivermectin and other macrocyclic lactones usually eventually cure demodectic mange. However, to do so they must be used more frequently and/or at a larger dose than the products labeled for heartworm prevention suggest. Ivermectin works just as well when it is given orally as it does when given by injection. Because these are “off-label”, non-FDA-approved uses, they need to be administered on the advice and under the care of your veterinarian – not because some internet site or neighbor tells you there is nothing to worry about. I put an image of Heartgard just above. Most veterinarians would probably have purchased the cattle or swine injectable livestock formula of ivermectin to treat demodectic mange and used that product “off label” in your dog because of convenience and economy.
The chief drawback to giving ivermectin and other macrocyclic lactones like moxidectin/Advantage Multi® is that a few dogs are highly sensitive to macrocyclic lactones. Those are dogs that carry a mutant MDR1 gene. These are usually dogs that are all or partially herding breeds, such as Australian shepherds, healers, old English sheepdogs and collies. But other breeds sporadically (occasionally) carry this genetic mutation as well. Dogs with the blue merle coloration often carry some of this genetic background. If this is at all in question regarding your dog, it needs to be checked through a specific blood test :

Antibiotic And Anti-Fungal Medications
As I mentioned, dogs with generalized demodectic mange are predisposed to bacterial and yeast skin infections that make recovery more difficult. When your veterinarian suspects that bacteria or yeast like malassezia have taken advantage of your pet’s unhealthy skin, your vet might decide to put your dog on oral antibiotics or perhaps an antibacterial shampoo containing miconazole/chlorhexidine, in addition to the medications dispensed to kill the mites. (read here) Those skin care products do not kill demodectic or sarcoptic mange mites – but they make the chances of rapidly curing your dog of mange much better and give more immediate relief to suffering pets.
Whenever possible, treat your pet’s skin infections of all sorts with topical, non-antibiotic, non-corticosteroid containing products. You and your dog share many of the same beneficial bacteria. (read here) When a pet in your household receives more than a few days of antibiotics, with time, its skin and digestive tract will repopulate with bacteria that are resistant to those antibiotics. Staphylococcus is not very particular whether it grows on your pet or on you. If staphylococci later cause a problem in you or another family member, the antibiotics that these bacteria are already resistant to will no longer work. So wash well with antibacterial soaps when you handle pets receiving antibiotic medications. Do not share products or appliances with pets receiving antibiotics and do what you can to minimize cross-transfer. These are the same precautions that nurses take to minimize the transfer of resistant staphylococcus in hospital settings. (read here & here)
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.



 Here Are Products Commonly Used In The Past:
Here Are Products Commonly Used In The Past: