Why Is My Dog Or My Cat Anemic?
Ron Hines DVM PhD
If your cat or your dog is anemic, its intent, rapid breathing, general weakness and pale gums are what you will notice first. Your veterinarian, using a stethoscope, might also detect a faster than normal pulse and perhaps even a heart murmur if your pet’s anemia is severe. You can listen to what that might sound like here:
Anemia is the presence of too few red blood cells in your pet’s circulation. Its blood is composed of a liquid portion, the plasma, and a cellular portion. That cellular portion is composed primarily of red blood cells which are also called erythrocytes or RBCs. The RBC’s job is to carry oxygen throughout the body. Red blood cells have a relatively short life (~110-120 days in a dog and 65-76 days in a cat). The next most common cells in normal blood are platelets. They are also called thrombocytes. For every 20 red blood cells or so there is about one platelet. The other cellular types in normal blood are white blood cells (the leukocytes). Leukocytes are all associated with your pet’s immune system. Compared to erythrocytes and blood platelets, there are much fewer leukocytes in normal blood. When your pet’s RBC count, PCV or hemoglobin level is low, your dog or your cat is anemic. Normal packed cell volumes/PCV of dogs and cats differ. In dogs, 41-58% is considered a normal PCV. Cats naturally have lower RBC numbers. Their normal PCV is 31-48%. Cornell University one of the top 3 veterinary schools in America, considers dogs with a decrease to 30-40% or cats with a decrease to 25-30% as being mildly anemic. Dogs with a decrease to 20-30% and cats with a decrease to 15-25% they consider moderately anemic. Dogs below 20% and cats below 15% are severely anemic.
There Are Two Kinds Of Anemias – Regenerative Anemia and Non-Regenerative Anemia
Regenerative Anemia
In regenerative anemia, your dog or cat is still attempting to make new red blood cells in its bone marrow to take the place of the missing ones as well as RBCs that have reached the limits of their lifespan. In non-regenerative anemias, your pet is no longer attempting to replace those missing RBCs. When your cat or dog has a regenerative anemia, its body is loosing RBCs faster than it can generate new ones in its bone marrow. That manufacturing process is called erythropoiesis. In regenerative anemias, your pet still has the ability to producing new red blood cells in its marrow at a normal or increased rate. In an attempt to correct the problem, your pet might even begin manufacturing RBCs in other locations. (read here)
The most common causes of regenerative anemias in adult dogs and cats are traumas, such as car accidents or dogfights. In young dogs and cats the most common causes are large numbers of fleas, ticks or hookworms. Another common cause of a potentially regenerative anemia in cats is infection with bartonella. In that disease, the bartonella bacteria adhere to and invade RBCs and in the process of your cat’s immune system attacking these organisms, RBCs are destroyed. (read here)
A regenerative anemia has a much better outlook for your pet than a non-regenerative anemia. So, some of the the key markers that your veterinarian will be looking when he/she reviews its laboratory results are indications that your pet’s body is rushing in to correct the problem. One of those indicators are the presence of increased numbers of reticulocytes. Reticulocytes are young RBCs. Normally, most reticulocytes remain in your pet’s bone marrow until they become fully mature RBCs. But in regenerative anemias, the cat or dog’s body senses the urgency for replacement RBCs and releases them into the blood stream earlier than normal. If your pet’s lab report shows an increase in their blood numbers, that is a very good sign. If no increase in reticulocyte numbers occurred, or worse yet, fewer than normal reticulocytes are present, your pet probably has a non-regenerative anemia. These changes do not occur immediately after a blood loss. It takes 3-4 days for that to occur and up to 7 days for reticulocyte numbers to peak.
Red blood cells begin their lives with a nucleus present. By the time they normally leave the bone marrow, their nucleus is gone. However, in the rush to correct anemia, your pet’s body often releases young RBCs with some of that nuclear material still present (polychromasia) and a size slightly greater than normal (increased MCV). Those immature RBCs also tend to vary in size (anisocytosis).
Other Less Common Causes Of Regenerative Anemia
I mentioned trauma and parasites as common causes of regenerative anemias. But there are other less common causes. Onions are known to cause regenerative anemias in dogs. (read here) Swallowing metal toys and keychain fobs composed of metals containing zinc can also lead to anemia. In cats, acetaminophen/Tylenol™ will cause severe, sudden anemia, (read here) Eating mothballs have also been responsible.
NSAID medications that veterinarians dispense to treat arthritis occasionally cause stomach and intestinal bleeding that results in anemia.
A Vitamin B12 Deficiency
The B Vitamins are very important in red blood cell formation. Because they are all water-soluble, it is common for too little of these vitamins to be absorbed from food sources when food passes too quickly through the small intestine, as it often does in pets with IBD. That disease occurs in cats and in dogs. (read here). B vitamin deficiencies also occur in all the chronic disease that decrease your pet’s interest in eating. That includes feline leukemia in cats (read here & here), various chronic inflammations and cancer. (read here & here)
An Iron Deficiency And Malnutrition
Meat-based dog and cat diets should not be deficient in the iron essential to producing the hemoglobin in red blood cells. When an iron deficiency anemia occurs in dogs or cats, it is usually due to the chronic blood loss of a heavy parasite load or due to a very inadequate diets such as one might see in feral cats and stray dogs. Those diets might also be deficient in copper and B vitamins which are also essential to prevent anemia. Lead exposure has also resulted in anemia.
Anticoagulants And A Lack of Thrombocytes
Anything that increases your pet to bleed can cause a regenerative anemia. The most common ones are mouse and rat poisons that delay blood clotting. A common sign are nosebleeds. Your cat and dog also depend on an adequate number of thrombocytes for its blood to clot. When fewer than normal numbers of thrombocytes are present, anemias can be regenerative or non-regenerative. (read here)
Non-regenerative Anemia
In non-regenerative anemia, your dog or cat has lost its ability to manufacture sufficient new RBCs in its bone marrow to replace the ones that have lived out their lifetime. I mentioned that red blood cells have a short lifespan.
Probably the most common cause of a non-regenerative anemia in both cats and dogs is late-stage kidney disease. To stimulate bone marrow production of red blood cells, both dogs and cats rely on a hormone, erythropoetin, (aka EPO) produced primarily in their kidneys. In kidney failure, uremic toxins build up in the bloodstream. These toxic waste products of metabolism suppress the production of erythropoetin. They also decrease the lifespan of red blood cells. (read here)
Inflammatory Cytokines
The inflammatory cytokines present in many chronic diseases are also known to suppress RBC production in multiple ways. (read here)
Immune-mediated Hemolytic Anemia
Immune‐mediated hemolytic anemia (IMHA) is another cause of non-regenerative anemia. In this immune system mistake, your pet develops antibodies against its own RBCs causing them to burst (hemolyze). This disease can appear spontaneously, or it can be initiated by “triggers” such as an infection, medication or vaccination. Even bee stings have been the likely trigger. (read here) In dogs with this disease, spherocytes are commonly seen microscopically. Autoagglutination of a drop of your pet’s blood is another common finding. A positive Coombs’ test is another. Even an association with pregnancy was once suggested. (read here)
Long-acting Estrogen Injections
At one time, veterinarians commonly administered injections of long acting estrogens as “mismating shots” to dogs that were accidentally mated. In North America, that has been replaced by aglepristone (Alizin®) which is much safer. The older estrogen medications that veterinarians used commonly caused anemia. Certain tumors release estrogens as well. They have the same suppressive effect on red blood cell formation (read here)
How Will My Veterinarian Treat My Pet’s Anemia?
If a cat or dog arrives at its veterinarian’s hospital with PCVs below 20%, that vet would probably consider giving your pet a matched blood transfusion. If its breathing and oxygen saturation improves in a high-oxygen environment, that might be sufficient until the cause of the anemia can be determined. If it is an immature pet and intestinal parasites are determined to be the cause, medications such as pyrantel or fenbendazole might be sufficient. If spontaneous bleeding is suspected, injectable vitamin K1 is often given. If trauma was the cause, immediate surgery to stem the bleeding might be indicated. If immune medicated anemia is determined to be the cause, corticosteroids are often beneficial. If NSAID medications such as carprofen caused gastrointestinal ulceration and bleeding, those medications need to be stopped, and intestinal protectants dispensed until healing has occurred. If chronic kidney disease is suppressing RBC formation, darbepoetin might help stimulate RBC production. (read here & here)
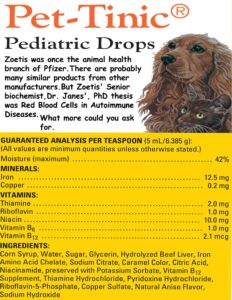
Mild to moderate cases of anemia can be treated with blood-building vitamins and minerals called hematinics. A common brand dispensed in North America, the UK and Europe is Zoetis’ Pet-Tinic™. It contains Corn syrup, water, sucrose, glycerin, beef liver paste, iron proteinate, sodium citrate, caramel color, citric acid, niacinamide, potassium sorbate, cyanocobalamin, thiamine hydrochloride, pyridoxine hydrochloride, riboflavin, cupric sulfate, natural anise flavor, sodium hydroxide. I would avoid niche products marketed by smaller companies that do not have a proven track record or full-time pharmacists and nutritionists on their staff. Always read and follow directions. If a little is good, exceeding the suggested dose is never good.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.