 Links To Other Articles On Liver Problems
Links To Other Articles On Liver Problems
I want to make it clear from the start that veterinarians do not have any medications that will cure chronic liver disease in your dog or your cat – yet. But I can tell you about recent progress in liver regeneration.
Today, at best, veterinarians try to stabilize your pet and slow its decline in liver function. That means slowing or reversing elevations in your pet’s Bilirubin, ALT, Alkaline Phosphatase, GGT, and PT numbers and increasing low blood albumin levels. You can judge progress as well by just looking at the color of your pet’s gums and sclera. Their yellowish tinge in liver failure is due to abnormally high bilirubin levels. It’s a healthy liver’s job to rid the body of bilirubin through its bile.
Why Is So Much Effort Being Devoted to New Liver Treatment Options?
It is the search for alternatives to liver transplants in people with liver failure that drives liver research around the world. That is particularly true in China, which accounts for over half of all human liver failure cases worldwide. The most common causes of liver failure in people are excessive alcohol consumption and acetaminophen (e.g. Tylenol) overdoses and the hepatitis B virus. Short of a rapid liver transplant, physicians have few successful treatment options proven to prolong life.
Your pet is unlikely to be exposed to the common human causes of liver failure. In dogs, the most common causes are probably the consumption of dog foods with excessive amounts of aflatoxins or leptospirosis. Certain toxic mushrooms can have similar destructive effects on the liver.
In cats, liver failure is most commonly due to hepatic lipidosis. However, the ingestion of pine oil or phenolic cleaning products, stagnant water algae and unpredictable reactions to drugs such as diazepam occasionally cause liver failure in cats as well.
Intestinal Bacteria Fortification – A Fecal Transplant
It has been found that the number and types of bacteria and other microscopic organisms that naturally inhabit the intestinal tract change when the liver begins to fail. What has not been satisfactory determined is if this change is part of the cause of liver failure or if it is the result of liver failure. In any case, transferring fecal bacteria from a healthy individual to an individual with liver problems (a fecal microbiota transplant) appears to be helpful. (read here, here, here and here)
Attempts At Liver Regeneration
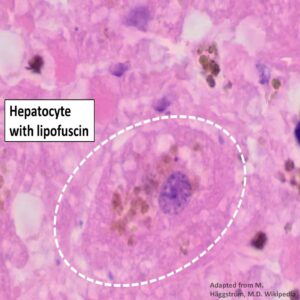
Liver cells are hard to keep alive in the laboratory. Each functional liver cell (hepatocyte) relies on its neighboring cells and its biochemical and hormonal environment to survive and perform its many tasks. Stem cells, fibroblasts, or umbilical cord mesenchymal cells, placed in the proper environment, can be induced to become hepatocytes. (read here, here, here and here) In the Netherlands, a country at the forefront of veterinary research, an attempt at liver regeneration in dogs that were genetically susceptible to liver failure has already been performed. (read here)
Hormones That Encourage Liver Regeneration
Your pet’s liver is a remarkable organ with a great potential to heal if its underlying scaffold structure and blood supply is still intact. (read here) One hormone that participates in liver repair is somatostatin. (read here) Others have ongoing projects attempting to encourage liver regeneration using granulocytic colony-stimulating factor, filgrastim or lenograstim. (read here)

I cannot tell you when any of these experimental techniques will enter the realm of veterinary medicine. But big leaps forward in regenerative treatments of all kinds are no more than a few years away. Just don’t expect your veterinarian to have access to them before your physician does.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.








