Ron Hines DVM PhD
You might find this list of other articles helpful:
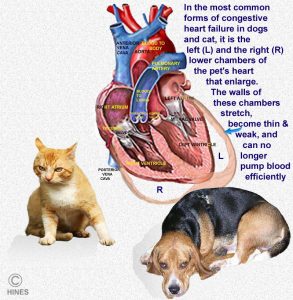
Like all mammals, dogs and cats have a four-chambered heart. It consists of a left and right upper chambered atrium and a left and right lower chambered ventricle. The left and right atria receive blood from the lungs and body respectively. The left ventricle is responsible for pumping oxygen-rich blood from the lungs out through the aorta into the body, while the right ventricle pumps the blood through the pulmonary artery to the lungs for oxygen.
The Heart’s Four Valves:
The heart has 4 one-way vales to keep blood flowing in the right direction. Because heart valves are fragile structures in constant motion, it is not uncommon for them to develop opening and closing issues as your dog or cat ages. The valve between the left atrium and ventricle is the mitral valve. The one between the right atrium and ventricle is the tricuspid valve. The one regulating blood passage into the aorta is the aortic valve and the one regulating blood going to your pet’s lungs is the pulmonary valve. The mitral valve is the most fragile of these four valves in your pet’s heart. In dogs, it is often the first one to wear out. In us humans, it is the aortic valve that causes the most problems.
What Signs Will I See If My Pet Has A Heart Problem?
The first sign that most owners notice is a cough. Coughs begin because enlarged, failing hearts allow fluid to pool in the lungs and also press on the wind pipe (trachea) – a structure just above the heart. Other signs you might notice in your cat or dog are earlier tiredness after activity, rapid breathing, poor appetite, an enlarged tummy (abdominal ascities), pale, “muddy” or bluish gums, and a rapid, weak pulse. Fainting is much less common.
What Might My Veterinarian Hear Through A Stethoscope?
Many of these pets have heart murmurs. Heart murmurs come about when a passage through the heart becomes too narrow or too wide or when a pet develops substantial anemia that changes its blood consistency. In middle-aged and older adult cats and dogs, heart murmurs usually mean that a valve is not working properly. In younger dogs and cats they can be a sign of an imperfectly constructed heart (a cardiac birth defect). The particular valve producing the sound may not be closing completely, or it may not be opening sufficiently for blood to pass through it without turbulence. Turbulence as blood rushes through an abnormal heart valve or channel is what produces all heart murmur sounds. The rhythm of a weakened heart also likely to changes. But unlike in us humans, frequent changes in the heart rhythm of relaxed dogs and cats is quite normal (sinus arrhythmia). Read about sinus arrhythmia here.
What Tests Might My Veterinarian Suggest?
If your veterinarian is suspicious that your dog or cat might have a heart problem, the first test we traditionally schedule are chest (thoracic) x-rays. We need two views to start with, one side to side (lateral) and the other bottom to top (DV/dorsoventral view). If your pet’s x-rays shows an enlarged heart, your veterinarian might be satisfied with that, begin therapy or offer you a consult with a formally trained veterinary cardiologist. If the radiographs are inconclusive or for backup evidence, your veterinarian might suggest a proBNP or similar blood test (Cardio-BNP Test, NT-proBNP, B-type natriuretic peptide yield similar information). These tests are especially useful in cats when your veterinarian is not sure if your cat has a heart problem or if it might be a lung problem or asthma. Another tests that a cardiac specialist might perform is echocardiography (doppler ultrasound) to see your dog or cat’s heart perform in real time, and an ECG/EKG to check if the electrical system of your pet’s heart is functioning normally.
What Are Some Of The Effects Of A Failing Heart?
As I mentioned, in dogs, the valves are often the first heart structures that are affected. Heart disease in cats more commonly involves the entire heart muscle – not just the valves.
Dogs let us know early on that there is a problem. Cat owners are often unaware that their cat has a heart problem until its heart is well on its way to failing. Often the only signs in your cat are weight loss, and difficulty breathing. Cats are more likely to make asthmatic and retching-like sounds than to have a persistent hacking cough. Unfortunately, even when given proper medications, cats with generalized heart disease rarely survive long periods. Signs of all forms of heart disease in cats are quite similar. So, your veterinarians will need to rely on sophisticated tests and the trained eye of a specialist to have the possibility of telling one potential cause from another.
Heart Problems That Are Common In Both Dogs And Cats :
In many ways, your pet’s heart is like a car’s motor. If one part goes out, it is not long before it causes another part to fail. So in reality, most actual cases of heart disease are a combination of several problems. The normal heart has a very precise shape. As its shape expands due to overwork and becomes more rounded, the heart is not able to perform any of its tasks well because of its distorted shape.
 Congestive Heart Failure (CHF):
Congestive Heart Failure (CHF):
Congestive heart failure is the result of an enlarged heart – one that allows blood to abnormally pool (congest), move sluggishly throughout the body and pool in areas where it does not belong. No mater what the underlying heart problem was, CHF is often the end result. You can read in more detail about how this problem affects dogs here. CHF is less common in cats. But when cats develop CHF, how it affects their bodies is quite similar.
CHF occurs when the heart is unable to meet the circulatory demands of the pet’s body. Many things can trigger it: a heart pumping against increased back pressure, decreased efficiency as a pump. valve defects, tumors, heartworms, heart beat abnormalities, or damaged to the muscle itself all cause the heart to enlarge and blood to pool in the pet’s organs and lungs. CHF can be the end result of any of those things. X-ray and/or cardiac ultrasound are the ways your veterinarian confirms CHF.
Because CHF is a common human problem too, new drugs are constantly being developing and refining to treat it. These human medications work quite well in dogs and cats too. So, your veterinarian might decide on a drug(s) I do not mention. This is particularly the case when you visit a veterinary cardiologist. They keep close watch on the methods used by human cardiologists. However, it is always uncertain if these newer human medications will extend the life of your pet any more than those that are more commonly used by your local veterinarian. It takes 5-10 years for even human meta studies to confirm the effectiveness or ineffectiveness of a new heart failure treatments, medications or supplements. (read here, here & here)
Veterinarians usually treat CHF with several medication groups at once:
Diuretics:
Veterinarians remove as much pooled fluids and blood as they can with drugs called diuretics. Once these excess fluids are removed from your pet’s lungs, its cough should improve or cease. The cow-like pot-belly associated with CHF should also go away. The most commonly used diuretics in dogs and cats is furosemide (Lasix®). When furosemide on its own is no longer effective enough in decreasing fluid retention in your dog or cat, veterinarians often add a second diuretic called spironolactone. Do not be surprised when your pet drinks and urinates more on these medications. One should never limit your dog or cat’s water consumption in an attempt to prevent pooled chest or abdominal fluids. That can cause severe dehydration which is bad or worse than the heart issue your pet faces.
ACE Inhibitors:
Veterinarians also attempt to increase the diameter of blood vessels throughout your pet’s body with vasodilator drugs so that your dog or cat’s heart does not have to work as hard. Most of the medicines of this group are called ACE inhibitors. The most common ones in this group that veterinarians dispense are enalapril (Enacard®) benazepril (Lotensin®) and lisinopril (Prinivil®). By making it easier for blood to flow through your pet’s blood vessels, ACE inhibitors help decrease your pet’s heart rate, and help preserve the heart’s remaining strength. The most common side effect of these drugs is lack of appetite and vomiting. If that occurs, your dog or cat’s dose needs to be adjusted.
Inodilators:
Inodilators, distant relatives of dopamine, are also called positive inotropes One compound in this group, Pimobendan (Vetmedin®) definitely seems to extend the lives of dogs and cats with CHF. Pimobendan increases the amount of blood that the weakened heart can pump by giving more strength to its individual muscle fibers. The drug also opens up (dilates) blood vessels throughout the body, so the heart doesn’t have to work as hard. One study found that dogs receiving pimobendan and furosemide lived 9 months longer than those receiving only enalapril and furosemide. It has been used in cats, although it is not licensed for that species. (read here) Its use in cats is still controversial.
Another drug in this group that was once quite popular is digoxin. Because of its many side effects and the limited length of time pets tend to survive while on it, I rarely prescribe it. It is at best a medication of last resort.
Antiarrhythmics:
The heart has a complex electrical wiring system to coordinate its contractions. When the heart is damaged, this system may fail. We call an abnormal heart beat rhythm a cardiac arrhythmia. Some of the drugs used to control arrhythmias are propranolol (Inderal®) procainamide (Pronestyl®), and tocainide (Tonocard®).
Less Proven Medication Options:
Effects are basically unproven, but there is certainly no harm in giving these a try:
A Lower Salt Diet
Many veterinarians suggest pets with heart disease consume a low sodium diet. This is probably a good idea if your pet also has elevated blood pressure or retained fluid. We really do not know if low sodium diets are as beneficial to pets as they might be to humans. (read here)
Coenzyme Q
Some veterinarians suggest coenzyme Q because of its possible beneficial effects in people with dilated cardiomyopathy and congestive heart failure. (read here)
Omega-3 Fatty Acids
Omega-3 fatty acids are high in fish oil. In people, there is some evidence that omega-3 supplements might reduce the risk of heart attacks and strokes. Based on this, some veterinarians suggest that dogs with heart problems also receive them. The makers of prescription dog and cat foods tend to increase the content of omega-3 fatty acids in the products they market for a variety of dog and cat health issues. (read here)
L-carnitine (carnitine):
L-carnitine is involved in the process by which the heart muscle converts fats into energy. There is some data that L-carnitine supplements help people who have heart disease. (read here) Whether or not it helps pets is something we do not yet know. (read here)
Taurine:
There is a small group of cats and an occasional dog that develop sudden heart disease due to a deficiency in the amino sulfonic acid, taurine. Once that link was discovered, pet food manufacturers added more taurine to their diets. Although we think more about cats that develop cardiomyopathy, a taurine deficiency has also been implicated as a possible cause of canine cardiomyopathy. One study discussed taurine’s possible role in that heart problem in golden retrievers. (read here) Since it is non-toxic, many veterinarians suggest a taurine supplement for all their cardiac patients.
Other Helpful Things You Can Do:
To keep your pet’s weight optimal, feed a name brand high quality commercial diet or prepare one you prepare at home.
When you exercise your pet, keep its activity at a level a bit less than what it would take to cause your pet to breathe heavily, pant or elevate its heart rate. Don’t give up short walks until you absolutely must. Dogs and cats benefit physically and mentally from physical activities and exploring new environments.
Heart Valve Disease Of Dogs And Cats:
I mentioned earlier that age-related scaring and distortion of the mitral valve is quite common in old dogs. The mitral valve divides the lower and upper left chambers of your pet’s heart. It’s constant hard work may cause it to fail to completely close and open. Sixty percent of dogs over 8 years old are said to have some degree of this problem. But less than half the dogs with this condition have any symptoms you would notice.
Many veterinarians have noticed that small breeds of dogs that eat soft food and table scraps eventually develop chronic mouth infections or periodontal disease. It is very common for these pets to also have a heart murmur related to their mitral valve. Dentists and many veterinarians believe that bacteria break loose from oral tissue, move through the blood stream and attach to the heart valves to cause a condition called endocarditis that eventually scar the heart valves. When a mitral valve wears out, its two flaps become blunted, shriveled and scarred so that they do not open or close properly. When this happens, blood does not flow in the normal pattern, but leaks back in to the left atrium and/or fails to fill the left ventricle fully before the heart beats. With time, increased back pressure causes one or more chambers of the heart to enlarge. As the chambers of the heart enlarge they press on the windpipe resulting in a dry, hacking cough. The enlarged heart also stretches the nerve fibers that control heart rhythm. That can resulting in abnormal heart beats or arrhythmias. As blood backs up, it pools in the lungs as edema that makes the cough even worse. Particularly, when the pet is lying down or at rest.
Right Side Heart Failure And Hypertension
Less frequently than left side heart failure, it is the right side of the heart that fails to move blood adequately. When that occurs, blood backs up between the heart and the lungs. You can read more about that problem through the previous link.
Puppies and kittens are sometimes born with abnormal hearts. This is congenital heart diseases – errors in heart construction.

Errors In Heart Development:
Subaortic Stenosis (SAS):
This problem is most common in big dogs (Rottweilers, Boxers, Newfoundlands, Golden retrievers, Great Danes etc.). Stenosis means narrowing. In cases of subaortic stenosis the puppy is born with an abnormally narrow passageway leading from its heart to its aorta. The problem comes in all degrees of severity – from very mild case, requiring no treatment to life-endangering seriousness.
When you take your puppy or kitten to your veterinarian for its first vaccinations, your veterinarian should listen to the pet’s heart. In a puppy with SAS, there will usually be a heart murmur over its chest near the left base of its heart. When a puppy is not severely anemic from hookworms, SAS and/or a patent (=open) foramen ovale are probably the most common anatomical reasons for these pediatric murmurs. (read here) This murmur is how most cases of SAS are first diagnosed. When discovered later in life the complaint is likely to be tiring after mild to moderate exertion. Not every puppy with a heart murmur has SAS or anything that serious. Puppies often outgrow heart murmurs without veterinarians really knowing what caused them in the first place. Only complicated tests can tell which murmur is important and which is not (benign or innocent heart murmurs). But if your pet still has the murmur when it is ~6 months old, the problem need veterinary attention.
When a puppy has a significant degree of SAS passageway narrowing, its heart has to work harder to force the blood through the narrow area just below the aortic valve. With time, the heart muscles will get thicker due to this extra effort. As the heart walls thicken, the full heart holds less and less blood and needs more and more oxygen. Eventually, the heart can begin to fail. Unlike older dogs with congestive heart failure, puppies with seriously narrowing SAS often die suddenly when clots form in the heart muscle or the heart’s electrical system fails. Neither the parent of an SAS puppy (nor the puppy itself) should ever be bred again.
What Signs Of SAS Might I See In My Puppy?
Most often, you will see no signs at all in your puppy. But as time goes by and the puppy’s heart muscles thicken, problems in the electrical system of the heart might cause fainting or even unexpected sudden death.
What Tests Might My Veterinarian Perform?
To decide how serious a heart murmur really is, your pet needs to have an echocardiography (doppler ultrasound) performed by a veterinarian experienced in interpreting the results. An x-ray and an EKG will also be required to see how much damage has already occurred.
What Are The SAS Treatment Choices I Have?
Medications:
The most popular drugs used to treat SAS are known as beta blockers (ß-blockers). The most commonly used ones are propranolol (Inderal®) and atenolol (Tenormin®). Beta blockers reduce heart rate, help control abnormal heart rhythm and reduce blood pressure. They are proven in their ability to extend the lives of dogs with SAS.
Surgery:
Open-heart surgery to correct a SAS problem in dogs has not been as successful as one might hope. Dogs that have had the surgery, live about as long as dogs that just receive medicine.
Balloon Valvuloplasty:
This technique is similar to the balloon angioplasties that are done to dilate blocked coronary arteries in humans. A catheter is threaded into the dog’s heart and a balloon is expanded in the narrowed area of the heart. So far, to the best of my knowledge, this technique has not been shown to lead to a longer life.
How Long Will A Puppy With SAS Heart Problems Live?
This is very difficult to predict. They younger a puppy is when a change in its energy level is first noticed and the louder the heart murmur, the bleaker its outlook. Most dogs with typical signs of SAS do not live over 3 years – even with medication. A cardiac work-up at a regional veterinary center that includes all the diagnostic tests, might give you more insight; but all pets with this condition can die with little or no warning.
Kissing Bugs And Chagas Disease
There is a group of blood sucking bugs that feed on the blood of sleeping dogs. They are called kissing bugs. These true bugs are found in hot humid climates all over the world. Where I live in South Texas, the Chagas disease parasite is transferred to dogs through the bite of our local kissing bugs. In the poorer areas in my region, 19.6 – 31.6% of the dogs have been exposed. (read here) One of the primary signs of Chagas disease in dogs are cardiac arrhythmias and heart failure. (read here) Veterinarians here are particularly suspicious that Chagas disease might be involved when a young dog that is negative for heartworms suddenly shows signs of heart failure. Besides keeping brush and leaf litter out of our dog’s outdoor environment I keep a 4% deltamethrin-impregnated flea/tick collar on our Labrador retriever, Maxx, (Scalibor®/Salvo®) because that particular long-acting insecticide is thought to repel kissing bugs. (read here) If the new isoxazoline flea and tick collars might be an alternative is unknown. Read about those newer prescription flea and tick collars here. In humans, benznidazole is the only FDA-approved treatment for Chagas disease. But it is unlikely to be effective in dogs (or humans) once Chagas-related heart issues have begun.
CATS:
Hypertrophic Cardiomyopathy Of Cats
I mentioned earlier that this problem was at one time more common due to a deficiency in the sulfamino-acid, taurine in commercial cat foods – offal, slaughterhouse waste, grains or substitute carbohydrates are considerably cheaper than high-quality meat. Mass pet food manufacturers tend to go with the cheapest ingredients. What goes into the product you buy is never what you see in the beautiful photos on the can or bag. Once veterinary nutritionists employed by the manufacturers knew that cats needed more taurine in their diet, all major brands of cat food have adequate taurine levels. Instead of better quality, they added cheaper synthesized taurine instead. (read here) Taurine deficiency in cats often caused their heart muscle to lose strength. Cats with hypertrophic cardiomyopathy usually lose weight and eventually have difficulty breathing. Blood clots often formed in the hearts of these cats and then move to other parts of their body. These clots often lodge in the cat’s lumbar area where the aorta divides to service each hind leg. In this disease the walls of the heart thicken, leading to inefficient pumping of blood. Blood pressure rises and fluid accumulates in the lungs. Eventually, the chambers of the heart enlarge and abnormal heart rhythms occur. Signs of this disease are labored breathing, rapid heart rate, heart murmurs, weakness, collapse and death. Rare heart valvular disease, hyperthyroidism and asthma can mimic hypertrophic cardiomyopathy. Veterinarians diagnose this disease with x-rays, electrocardiograms (EKG = ECG) and cardiac ultrasound. It is possible that cats with liver issues might require more taurine to compensate for their liver’s reduced abilities to process taurine. (read here)
Veterinarians treat hypertrophic cardiomyopathy in cats with lower salt diets, diuretics, blood thinners, and medications such as diltiazem and atenolol to stabilize your cat’s blood pressure and heart rate. Do not give aspirin to your cat without veterinary supervision – cats do not handle aspirin well. NEVER give them Tylenol. There might be a breakthrough in treating this problem. Read about that here.
Feline Dilated Cardiomyopathy
A second, genetic form of cardiomyopathy occurs in Siamese, Burmese and Abyssinian cats. Veterinarians treat this condition with the same medications that increase heart efficiency and decrease pooled fluid within the lungs. We also give them drugs to reestablish their normal heart rhythm. Many veterinarians suggest a taurine supplement for any heart condition in cats. Taurine might be beneficial and there is certainly no harm in giving it in reasonable amounts. A similar heart disease can also occur secondary to an over-active thyroid gland (hyperthyroidism). Cats with this and the previous problem generally do not live very long despite therapy.
Restrictive Cardiomyopathy Of Cats:
In this condition localized scarring of the cat’s heart muscle prevents normal heart beat. This eventually leads to an enlarged, weak heart and congestive heart failure with signs in some ways similar to what veterinarians see in dogs. Signs of the disease are poor appetite, weight loss and difficult respiration. Sometimes blood clots that cause paralysis of the limbs occur as well. X-rays, EKG and ultrasound all show atrial enlargement. Veterinarians treat these cats with calcium channel blockers such as diltiziam, diuretics such as furosemide and perhaps low doses of aspirin or another more modern medication that prevents blood clots. Aspirin must be used with extreme caution in cats – if at all. Do so only under the supervision of your veterinarian. Lower sodium diets might also help – if your cat will eat them. If cat owners are fortunate, a cat with this disease might live an additional year.
Corticosteroid-related Congestive Heart Failure in Cats
The University of Minnesota Veterinary Center noticed an occasional link between heart failure in cats and a recently given dose of a number of corticosteroid medications. Particularly, when the product was the injectable form of methyl prednisolone acetate = Depo-Medrol® aka “Depo”). Of the 160 cats with heart failure that passed through their clinic in a ten-year period, at least 8% that developed congestive heart failure had received that or similar medications within the 1-3 weeks preceding their heart problem symptoms. This unique form of heart disease often resolved itself with time. (read here) Corticosteroids are often given to cats with respiratory problems that are believed to be due to asthma. In other cases, they are given for allergic skin conditions or as appetite stimulants.
Dogs:
Dilated Cardiomyopathy Of Dogs:
Read more about this heart problem here. In this condition, as in cats, the heart chambers enlarge to the point where they can no longer pump blood efficiently. It is most common in large breeds of dogs and rare in small breeds. Doberman Pinschers, Great Danes, German Shepherds and Labrador Retrievers are particularly at risk. The disease is most common in middle-aged dogs, especially males. Usually, the cause is unknown, however taurine deficiencies, parvovirus infection and the use of adriamycin® (doxorubicin) have all been suspected causes.
The overly stretched heart muscle that occurs in this disease is a very inefficient pump. Signs of the disease are those of congestive heart failure: difficult breathing, weakness, coughing and fluid enlargement of the abdomen. These dogs may need oxygen until their medications have time to to work. Lower salt diets as well as supplements that contain taurine, L-carnitine (carnitine) and coenzyme Q might also be helpful. In my experience, dogs do not survive long with this condition.
Hypertrophic Cardiomyopathy Of Dogs:
This disease is quite rare. As in cats, the muscles of the heart thicken and become inefficient at pumping blood. The signs of the disease are the signs of congestive heart failure e.g. difficulty breathing, coughing, heart murmurs and exercise intolerance. There might be a breakthrough in treating this problem. Read about that problem here.
How Will I Know If My Dog Or Cat’s Heart Medications Are Working?
The most common reason pets with heart problems come to see veterinarians is because of coughing and breathing problems. They tend to breathe faster than they should, they tend to be congested, and they are emotionally distressed. One can have complicated, and frequent tests performed to evaluate if the medications you are giving are doing their job. But monitoring your pet’s breathing rate, freedom from congestion and relaxed attitude at home is just as accurate – perhaps even more so. If the medications are working, your pet will breathe slower and easier. When it is at rest, and it will show more interaction with you and its environment. If you want to confirm your opinion as to its situation, have your vet run an occasional proBNP test (or Cardio-BNP™) to confirm the test levels are dropping or at least holding steady. (read here)
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.