All About Lyme Disease In Your Dog – What To Do When Your Dog Tests Positive
Ron Hines DVM PhD







What Is Lyme Disease?
Lime disease is caused by a bacteria, Borrelia burgdorferi. Lyme disease organisms can attack many parts of your pet’s body. For that reason, the signs of it you see (if any) in your dog vary greatly.
This bacteria is transmitted by certain ticks. Borrelia belong to a family of bacteria called spirochetes. They are not very particular as to the species of animals they attack.
Borrelia burgdorferi, the spirochete, has always been around – we just didn’t pay much attention to it until recently. Its illness has been called Lyme disease ever since 1975, when an astute doctor recognized it in a cluster of children near the town of Lyme, Connecticut.
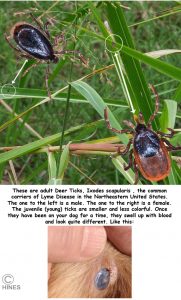
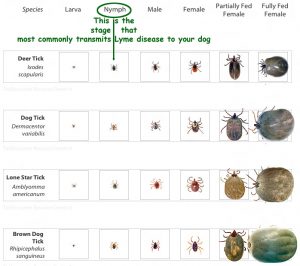
As I mentioned, the Lyme disease bacteria is transferred by ticks. In the Northeastern US, that tick is usually the deer tick, Ixodes scapularis – the ones in the photo at the top of this page. On the upper West Coast, it is I. pacificus that is thought to be responsible for most Lyme disease transmission. Lyme disease is less prevalent in areas where less rain falls – but why the number of cases in dogs and people go up and go down is still unclear.
Much of the information you read on the internet concerns the signs of Lyme disease you might see in people. Many pet owners reading that online information suppose the same signs would occur in their dog. However, Lyme disease will not affect your dog in the same way it affects you. People often develop a rash at the point where the tick attached as well as flu-like symptoms. In dogs the most common symptoms are joint pain and fever. Both do not usually start until 2-5 months after the pet was bitten. A few dogs develop swollen lymph nodes. Very, very few ever develop the heart and neurological problems seen in Lyme disease in humans. When a Lyme-positive dog develops kidney problems that are related to the disease, it is most often late in the disease process.
Lyme disease is a perplexing, frustrating condition because signs can present themselves in so many different ways – or no signs other than a positive blood test. No two cases are quite alike and the wide variety of symptoms that Lyme can produce can be confused with many other dog disease and health issues. Because of this, Lyme is sometimes called the Great Pretender. The fact that Borrelia usually produce no immediate symptoms in dogs make the choice of treatment and evaluating treatment success just as confusing.
In the United States, more than 90% of the Lyme cases occur in the Northeast and North Central states. Northwestern California and Mississippi also see quite a few positive dogs.
How Did My Dog Catch Lyme Disease?
Your dog was almost certainly bitten some time ago by a tick that carried the Lyme organism. Being around another infected dog does not spread the disease. It takes what we often call a “deer tick”. Some call them black leg ticks, others call them black legged ticks. Most of the time, a deer was not involved. These ticks feed on many other types of animals. In the northeast, a woodland deer mouse
What Are Symptoms Of Lyme Disease That I Might See In My Dog?
The majority of dogs that are infected with Lyme disease show no symptoms at all. Most of these dogs are identified through routine yearly testing at veterinary hospitals. We do not know why some dogs are affected with symptoms and others are not. In some animal species, the age at which they are infected has a lot to do with the development of symptoms – younger animals were affected more severely than more mature ones. Perhaps something like that occurs in younger dogs as well. Some studies suggest it does.
However, a small portion of infected dogs do develop sore, painful joints weeks or months after infection. Some of these dogs run low-grade fevers as well. But the signs you read about in humans with Lyme almost never occur in pets.
Ordinary arthritis, not due to Lyme disease, is usually constant in the joints it affects. But lameness due to Lyme disease often shifts from leg to leg. These swollen joints are usually hot and painful and occasionally the lymph nodes at the top of the leg may be slightly enlarged as well.
The front legs are most commonly affected. When they are, it is the lymph node on the shoulder of that leg that may be enlarged. Many of these ill dogs are also depressed. They may yelp when their joints are pressed, and they may be quite reluctant to walk. When they do walk, they might walk with a stiff shuffling gait and an arched back because of their discomfort.
Ticks might still be present or recalled as having been present on your pet to bring Lyme Disease to mind. Perhaps off-leash romps in an oak-wooded areas with lots of leaf litter on the ground.
In longstanding cases, destructive chronic inflammation can occur in your pet’s heart, kidneys and nervous system.
Your Pet’s Kidneys At Risk In Lyme Disease
Although it appears that most dogs live in relative tranquility with the Lyme organism, the kidneys of some Lyme-positive dogs do appear to suffer. Lyme organisms contain proteins that cause your pet’s immune system to produce antibody molecules in large number. Although these antibodies are not very effective in killing off the Borrelia, they are large enough to become trapped in the filtering mechanism of your pet’s kidneys. There they can stimulate destructive changes called immune complex glomerulonephritis. This disease slowly destroys the blood-cleansing ability of the kidneys.
Because this occasionally occurs in dogs that are chronic carriers of Lyme, many veterinarians suggest that Lyme positive pets have yearly tests that detect early signs of kidney disease. The tests most commonly performed to detect early kidney damage are the urine P:C ratio or the microalbuminuria test. You can read about chronic kidney disease and its treatment in your dog in another of my articles here.
Is This An Autoimmune Disease?
When the symptoms of Lyme disease occur, they are often similar to autoimmune diseases. Some of the pathological changes associated with Lyme disease are quite similar to those found in autoimmune diseases. In those diseases, an invading bacteria is sometimes the trigger that begins the disease – but the damage is caused by the body’s own immune system turning on itself. Injury by “friendly fire”.
What we know about this regarding Lyme we know from studies designed to help humans. Those studies indicate that once the immune system is alerted to the presence of Lyme organisms, it produces cells and antibodies that attack normal tissues of the body as well as the Borrelia. That might explain the cause of joint inflammation often seen in dogs with long-standing cases of Lyme disease.
But there are other scientists who believe that your pet’s immune system may not be chasing phantom “invaders” as it does in autoimmune disease. That is because other studies have shown that Lyme organisms are extremely clever at “hanging around” in the body and avoiding test detection after the acute phase of Lyme disease is over.
Is Lyme Disease Becoming More Common?
Probably so.
Lifestyle and ecology changes have brought Lyme disease-carrying ticks closer to your home, your pets and you. Suburban wooded subdivisions are more common than they once were. Folks living there are more likely to feed wildlife – consciously or inadvertently – than they once were. Those raccoons, deer and other urban wildlife bring Lyme disease-carrying ticks close to your home. But the biggest culprit is probably the cute little field mouse in the image above. It can be covered with Lyme disease-carrying ticks. Many small rodents transmit Lyme but are themselves immune to the disease. Read about that here and here. Family farms used to surround our large cities. In those days, hungry barn cats kept the mouse population under control. The pampered, well-fed felines of today are considerably less motivated to catch mice. What forests still surround cities are fragmented now. Roads and urban construction crisscross them. In those fragmented forests, mice thrive and crank out babies because their old predators, fox, bobcats, snakes, owls and hawks do not survive for long when they must cross roadways. Mice, on the other hand, thrive on 1/3 of an acre.
But the increased availability of rapid tests that your veterinarian can perform in the office are certainly responsible for some of the increase in Lyme disease diagnoses. Without a doubt, we veterinarians missed many cases before these tests became available to us. Heightened public and veterinary awareness of Lyme disease also accounts for some of the increase in cases that are reported.
Lyme disease is not a problem in all parts of the United States. Dog, with tick exposure, in the Northeast are at the highest risk. Those in the Pacific Northwest are also at moderate risk – depending on the dog’s lifestyle and tick exposure. A belt of cases also meanders down the Mississippi River drainage. Since the prevalence of Lyme disease in dogs mirrors the disease’s prevalence in humans, you can follow the risk of Lyme disease to your dog at the CDC human site. In Canada, Nova Scotia has the highest infection rate (~15.7%).
The CDC might be slow in recognizing the presence of Lyme in some areas of the United States. For example, looking at their 2016 map, one might think that the risk of exposure to the Lyme organism in Texas, my home, is quite low. However, a quarter of Texas deer ticks collected in a recent study were found to carry the Lyme bacteria. The data I have access to is quite preliminary and needs to be confirmed. Perhaps other factors here in the Southwestern United States influence infection rates in humans and dogs besides the simple presence of infected ticks. Perhaps, veterinarians and physicians here just aren’t looking out for it as much. Perhaps another tick-transmitted the Borrelia, disease we have in dogs down here in Texas, TBRF, was confused with Lyme.
How Will My Veterinarian Check My Dog For Lyme Disease?
The most commonly used test to check for Lyme disease in your pet is the Idexx SNAP® tests that your veterinarian runs in the office on a drop of your pet’s blood. The test kit looks similar to the image above. Many of these test kits not only detect for exposure to Lyme, they also check for the presence of heartworms and other tick-borne blood diseases. This test is for exposure only. It checks for antibodies that indicate Lyme is or was present in your dog. A positive test result does not tell you if the organism is still present, how many organisms are present, or if the organism is currently causing health problems in your dog.
There has been some recent criticism of the accuracy of the current tests available to your veterinarian – in certain instances, the tests apparently miss positive dogs and report uninfected dogs as positive.
Do not panic if your veterinarian says your dog is positive for Lyme disease. In 2007, almost two dogs in ten in the Connecticut area had positive test results. In addition, previous Lyme disease vaccinations your pet may have received or exposure to other, similar organisms appear to sometimes cause false positive test results for Lyme disease.
If your pet tests positive for Lyme on the 3Dx test – particularly if it has health issues – you need to have a second test performed to confirm the first. This second test looks for the number of antibodies your pet produces against a particular component protein on the surface of the Borrelia bacteria. At the time of the writing of this article, this test was only available through Idexx Laboratories. It has largely replaced an older test called the western blot. The second test is called their Quantitative C6 assay, and it looks for the level of antibodies your dog has produced against this specific surface protein on the Borrelia (the C-terminus of Osp C). Read about that here.
Your veterinarian will send out a blood sample from your dog for this test. The beauty of this test is that it measures the level of a specific antibody that is only present when the Borrelia is still present. So dogs that have cured themselves or received prior vaccinations are not confused with pets that have an active Lyme infection. It is hoped that this test will also allow your veterinarian to monitor the success of antibiotic treatment of your pet.
My only concern with the value of the Idexx Quantitative C6 test is that the only information available is distributed by the Marketing Department of Idexx themselves, or through marketing seminars and articles that Idexx paid for. Independent confirmation would be comforting.
If your dog is positive on either test, your vet may suggest urine tests to be sure no kidney damage has occurred (the urine P:C ratio & microalbuminuria test I mentioned earlier). Your vet may also suggest blood work analysis to gauge your pet’s general health.
What Lyme Disease Treatments Might Help My Dog?
Treatment of early Lyme disease is straightforward. The American College Of Veterinary Internal Medicine recommends a 30-day treatment with doxycycline. If kidney function tests were abnormal they suggest the pet stay on the medication longer and that it receive a diet formulated to minimize kidney problems. Read about that here. There are other antibiotics that are effective in treating early Lyme disease. But they are not as effective in treating the other disease organisms that ticks often carry and which might be in your pet’ system as well.
If your pet is experiencing joint pain, an anti-inflammatory NSAID medication such as Rimadyl® might be prescribed (don’t give your dog any of that group of drugs that are not approved by the FDA or EMA for use in dogs).
Dogs given antibiotics early in Lyme disease improve. But there is some doubt that the organisms are ever entirely eliminated from their bodies. Many veterinarians feel that it goes into remission but continues to lurk in the dog’s body in some “sleeping”, inactive form. Read about that here and here. Others believe that only bits and fragments of the dead organisms persist.
Your veterinarian may want to run additional follow-up blood and kidney tests subsequent to the antibiotic treatment. We are hopeful that repeat tests will show that your pet’s C6 antibody level is dropping and that that is evidence that the antibiotics and your pet’s immune system are eliminating a large number of the Borrelia from its body.
Why Are Lyme Treatment Decisions So Difficult?
It appears that many more dogs have positive Lyme tests than will ever show symptoms of the disease. The common tests only confirm the presence or recent exposure of your dog to the Lyme organism. They do not tell us how successfully your dog will be in dealing with that exposure. Recent studies at Harvard University tell us that there are several strains of the Lyme bacteria circulating in the United States. Some appear more likely to cause symptoms than others (e.g. RST1 strain). Some strains disseminate throughout the body faster than others. Read about that here. A single tick is even capable of transmitting more than one strain at a time. Read about that here. Compounding that in humans (and mice here) are differences in individual genetics that make the results of exposure to Lyme organisms highly unpredictable. A similar situation might easily occur in dogs – veterinarians just don’t know.
What Should I Do If My Dog Had A Positive Lyme Test But It Looks Healthy?
This is where veterinarians are in much disagreement. The 2005 position paper of the American College of Veterinary Internal Medicine (the ACVIM) stated: “Although it is unknown whether treatment of seropositive healthy dogs is beneficial, the consensus is that seropositive dogs should be evaluated for proteinuria and other coinfections and tick control prescribed.” In effect, what these experts were saying was that if kidney tests, physical examination and blood work were normal, it was unclear whether the dog should be treated with antibiotics or not. By 2018, the opinions of four out of the six ACVIM Lyme disease experts had changed. The four no longer routinely recommended treatment for such dogs. The reasons given were concerns about the general over-use of antibiotics, no proof that giving antibiotics lessened the dog’s chances of later developing kidney or arthritis issues, that antibiotics might not cure them and the fact that unless the dog owner moved, their dog would probably get infected again.
That may be true, but doxycycline is an inexpensive drug that has been used safely for many years in pets and humans. If the dog that received the positive test was the pet I loved, I would put it on doxycycline – if only for my peace of mind. The downside of not treating is just too great to worry about the very small chance of side effects or a treatment that was, perhaps, unnecessary. I would probably also extend the medication for my dog for an additional month if the pet tolerated it well.
There is also some evidence that just because your dog remains outwardly healthy is no guarantee that undesirable tissue changes are not occurring due to the presence of Borrelia. It might be many years before those changes became evident. Read about that here.
What About Dogs That Have Had Lyme Disease For Long Periods Of Time – Chronic Lyme?
When the Lyme organism has been in the body for extended periods of time, it does not respond to antibiotics as well as initially. Read more about that here. That is why dogs with chronic Lyme disease are much more difficult to cure. I believe that they should receive antibiotics, just like acute or recent case, but I believe that those antibiotics need to be given for longer periods. I would not give antibiotics for long periods of time just because a dog has health issues and is Lyme-test positive unless there was some concrete evidence the the two problems were actually related. Physicians struggle and argue about that all the time. Read more about that here.
In some cases, ceftriaxone (Rocephin®) antibiotic is added to the treatment as is done in humans with chronic Lyme disease. Most of these dogs are suffering from joint or organ damage – problems that are treatable but not curable. If your pet has painful joints and arthritis that are thought to be due to chronic Lyme disease, it needs to be managed in the same ways suggested for other arthritic joint problems. Read more about how to deal with that here.
If your veterinarian detected kidney damage in your dog, it needs to be treated and managed in the same ways suggested for pets with damaged kidneys. Read about that here.
Can I Catch Lyme Disease From My Dog?
The generally accepted belief, which I share, is that you are not going to catch Lyme Disease from your infected dog. However, if your dog has Lyme disease and if a tick bites your pet and then bites you, you can become infected. That is why eliminating ticks from your dog and your home environment is so important. There is a contrarian view – not widely accepted in the scientific community or by veterinarians – that Lyme can transfer through other means than a tick bite.
Are There Things I Can Do To Prevent My Dog From Catching Lyme Disease?
Yes
Eliminate ticks from your dog and its environment. Lime disease requires infected ticks to infect your dog. If you get rid of the ticks or keep your dog away from areas that are tick-infested, it will not catch Lyme Disease.
Here are some things that will help in doing that:







Vaccination
There are several vaccines approved to prevent Lyme disease in dogs. I personally prefer taking steps to reduce your dog’s exposure to ticks rather than vaccinating against Lyme disease. Their effectiveness is controversial. But if you elect to give your pet Lyme vaccine, my personal preference is for Recombitek Lyme® vaccine manufactured by Boehringer Ingelheim/Merial. That is because it uses recombinant subunit technology to minimize vaccine side effects. The manufacturers state that this vaccine will reduce – but not prevent Lyme disease infection. I suppose they mean that it will reduce disease signs in dogs that become infected. The Manufacturers suggest these vaccines be given every year.
I only suggest that your dog be vaccinated for Lyme disease when the infection is prevalent in your community and your dog’s lifestyle continues to put it at high risk. That means you should consider vaccinating your dog if you continue to see ticks on it, or it roams in meadows, woods and parks that are tick-infested. The society of veterinary internists, the ACVIM, initially stated: “The use of Lyme vaccines still is controversial and most [veterinarians] do not administer them.” There is still disagreement – the six member panel was evenly split between veterinarians who thought the vaccine was beneficial and those that did not.
There is another fact that brings the effectiveness of these vaccines into question. The safer subunit vaccines were developed to protect against a particular antigen protein of the Lyme organism called OSP-A. After these vaccines were already in production, it was found that other antigen proteins (OSP B & C) were also important in developing immunity to Lyme disease.
Should My Lime-Positive Dog Be Vaccinated For Lyme Disease?
I see no benefit in that.
What If I Discover that My Pregnant Dog Is Positive For Lyme Disease?
If your pregnant dog shows no symptoms of Lyme disease and its C6 titer is not elevated, wait until it has delivered its puppies and then have it placed on an extended course of amoxicillin. If the dog is ill and your veterinarian feels the symptoms are associated with an active case of Lyme disease (elevated C6 test, fever, etc.), I would begin the amoxicillin immediately. There are veterinarians who disagree. They mention a rare condition known to occur in humans suffering from similar diseases in which symptoms temporarily get worse when antibiotics are given. It is called a herxheimer reaction. We do not even know if a similar situation occurs in dogs. In any case, to me, the health of the mother is a more important concern.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.