When Your Dog Faces Hip Dysplasia
Ron Hines DVM PhD
 Arthritis, Joint & Back Pain in Your Older Dog
Arthritis, Joint & Back Pain in Your Older Dog
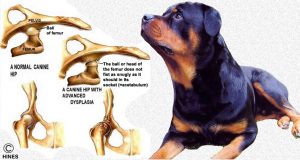
Hip dysplasia and the arthritis that accompany old age are the two most common skeletal issues that face our canine friends. Hip joint wear is inevitable. But when your younger dog develops hip dysplasia, it is usually the result of an inherited (genetic) tendency for its hip joints to be too lax or loose (laxity/subluxation). (read here) This abnormal looseness exists between the articulating ball of your dog’s hip joint (its femoral head) and the pelvic socket of the hip joint (its acetabulum). Loose unstable joints eventually lead to inflammation, remodeling of the joint’s configuration and pain. I tried to show those changes in my first drawing. The second image is an x-ray of a younger dysplastic dog. The arthritic remodeling and bone contour changes in that dog’s hips are not as evident yet.
Male and female dogs develop hip dysplasia in equal frequency. Veterinarians see it most often in the larger and the giant breeds. German shepherds, Rottweilers, and St. Bernards are high on the list. When it occurs in a specific individual of a high-frequency breed, it is often in the “larger than life”, eye-catching dog on the top end of its breed’s size scale. Those are the dogs that often win “Best Of Show” – hence their genes for largeness are likely to get spread around. Other breeds that suffer from dysplasia are actually intentionally bred to be dysplastic to give them that funny, waddling gait. Eighty-three percent of English bulldogs were once reported to be dysplastic. (read here)
Dog breeds that are resistant to hip dysplasia tend to be about the size of ancestral dogs – the ones that first threw their lot in with humans. They have refined features, a long snout and a multi-talented body structure designed to be swift and to survive the hardships of semi-feral life. Wild canids like wolves, foxes and jackals are free of hip dysplasia issues. Of course, their lives in the wild are much shorter than dogs, so we don’t know how extended old age might affect them. That is not to say that our smaller, lighter weight breeds are entirely immune to hip dysplasia. When hip dysplasia does affect them, smaller breeds are less likely to show as many signs of pain, stiffness and restricted mobility. That is probably due to the lesser weight their hip joints must carry.
Because CHD has a strong genetic element, it tends to occur when one or both of your dog’s parents were also somewhat dysplastic – or at least carried some of the genes that predispose dogs to the problem. And because many genes are involved, we call it a polygenic or polygenetic tendency, characteristic or trait. Polygenetic traits are particularly difficult to breed out of a group of dogs. (read here)
Even if your dog inherits an unfortunate combination of genes, hip dysplasia is not inevitable. That is because your dog’s individual growth rate and diet (read here), environment, neuter status and age at neutering (read here) exert substantial effects as well. Canine hip dysplasia can skip generations. It can affect some puppies in a litter while sparing others. All that, plus the fact that multiple gene are involved, is what makes the problem so difficult for breeders to stamp out.
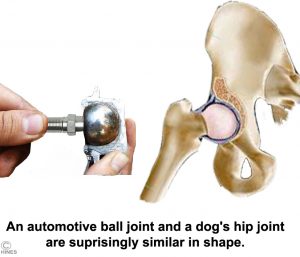
Your dog’s hip joint is constructed similarly to the ball joint of your automobile – similar to the image I drew above. This type of arrangement forms a very strong weight-bearing structure that allows great range of motion. But for this joint to work properly, the ball must be held deeply and snugly within its socket. Your dog has a series of very strong ligaments as well as fibrous layers (the joint capsule) that accomplish that when they are working properly. When they are lax, as in dysplasia, shearing forces are applied in ways that are destructive to the living tissues that comprise the hip joint.
Because a joint is a living structure, individual bone cells response to this irritation in predictable ways. The pet’s hip bones slowly change their shape (remodel). They recede in the areas of increased pressure, and they proliferate in the areas surrounding the pressure and irritation. The process (actually the result) is called osteoarthritis or degenerative joint disease. Some degree of osteoarthritis, including the hips, occurs in all of us and our pets as we get older. But loose joints, joints in improper alignment and joints carrying too much weight will usually develop the problem sooner.
There are all degrees of canine hip dysplasia. They range from very minor changes, which cause no lameness or limping, to severe cases in which the entire architecture of the joint is lost to arthritis. In these more severe cases the round ligament as well as the ligaments of the joint capsule are stretched, allowing the ball to wobble (subluxate) or even for the ball of the femur to slip entirely out of the acetabulum (a full luxation). Although inherited hip dysplasia always affects both legs, whichever side bothers your dog the most on a particular day is the side that will exhibit lameness, limping and pain the most.
The bone surfaces within the hip joint that touch each other are coated with a slick hyaline cartilage coating. In a normal joint, they are as smooth as glass, lubricated and slick with intra-articular fluid and cushioned with a shock absorbing under-layer of more fibrous cartilage. In dysplastic joints, these layers have eroded off, allowing painful bone-to-bone contact. When unprotected bone rubs on bone, the bone surfaces under pressure dissolve while new bone cells (osteophytes) form adjacent to it (on the periphery). It is a vicious, self-perpetuating cycle. The femoral head that once looked as round and smooth as a billiard ball now becomes flattened and mushroomed, with cauliflower-like new bone on its periphery (edge). The socket or acetabulum loses its normal depth and becomes shallow.
What Signs Might I See If My Dog Has Hip Dysplasia?
In puppies, young or adolescent dogs, walking abnormalities are due to hip joint looseness itself. In mature dogs, they are more likely to be due to the pain of hip arthritis. It is quite rare for pain to be a major factor in their abnormal gait before they are six months of age. Dysplastic puppies are born with hip joints that appear normal on ordinary x-rays. That is because the final shape of their hip joint is molded by forces associated with joint movement and walking. At 12 days of age there is no discernible radiographic difference between the hips of a dysplastic and a normal puppy. But you might notice a gait often referred to as “bunny hopping”, a rocking (“waddling”) motion as they walk, and perhaps some rear leg muscle weakness due to inactivity. The puppy might sit more on its haunches with its legs splayed outward (but all young puppies are poorly coordinated). As time goes by, the pup might have trouble climbing stairs or navigating up slopes, and it might be reluctant to jump up or over low obstacles. When pain finally does become a significant factor, the pup will often keep its rear legs placed farther forward than normal in order to shift more of its weight to its front legs.
When you examine these dogs with advancing symptoms of hip dysplasia, their upper thighs and hips are often bony and lack muscle mass. They are often “cow-hocked”, standing with their hocks almost touching. Some of these adolescent dogs actually improve for a time as their hips reach full calcium content (ossification) and before the pain of hip arthritis becomes a major issue. In hip x-rays taken of these younger dogs, the degree of joint changes may not correlate well with the pain your dog is experiencing. Some dogs that show significant joint changes show little pain, and vice versa.
Older dogs share many of the same signs I described for puppies. With time, those signs tend to intensify. In significant cases, stiffness on rising becomes your dog’s problem. Decreased activity levels compared to their peers are common as well. As in younger dogs, disuse will cause the muscles or their hips and thighs to be smaller than their non-dysplastic peers. They often also show hesitance getting in and out of cars. To pass inactive time, they often also spend more time grooming and worrying areas on their body that annoy them. Those and other low-motility endeavors are preferred. This can lead to problems such as lick granulomas, elbow and other pressure calluses, as well as skin sores and regional hair loss. Since all grades of hip dysplasia occur, many dogs with mild to moderate hip dysplasia don’t begin to hobble until they are about 4 or 5 years old. Working dog breeds can be particularly stoic and show little sign of lameness until the arthritis in their hips is well advanced. Pain in these dogs is often worse after exercise or first thing in the morning. That morning stiffness usually works out as the day progresses. Many of these dogs would rather sit on their haunches than stand. They might not be able to keep up with you on your walks like they once did. Your dog’s problems might be worse in cold weather – particularly when it has been spending time on a cold cement or tile floor. As I mentioned earlier, x-rays can be misleading in these dogs since their degree of joint destruction may not correlate well with the degree of pain and lameness they are experiencing. When your veterinarian has rules other possible causes of hip pain out, a trial month on one of the many canine NSAIDs such as carprofen (Rimadyl®, Novox®, etc.), deracoxib (Deramaxx®), firocoxib (Previcox®), meloxicam (Metacam®) etc.) is often the best way to confirm or rule out an arthritis problem.
How Will My Veterinarian Confirm That This Is A Hip Dysplasia Problem?
As I mentioned, only x-rays can positively diagnose hip dysplasia in your dog or rule it out. But there are other signs your veterinarian will notice that bring dysplasia to mind:
![]() Your dog’s breed age and size and family history are clues.
Your dog’s breed age and size and family history are clues.
![]() Your veterinarian will probably ask you to walk your dog around the office or exercise area to observe its gait. A problem here is that dogs in unfamiliar environments often hide minor to moderate lamenesses they exhibit at home.
Your veterinarian will probably ask you to walk your dog around the office or exercise area to observe its gait. A problem here is that dogs in unfamiliar environments often hide minor to moderate lamenesses they exhibit at home.
![]() Your vet will closely examine the whole of your dog’s rear legs looking for alternative explanations for your dog’s discomfort. Things like broken toenails, interdigital cysts, thorns, knee issues and the like. Fresh skin abrasions that might indicate recent hip, leg or back trauma are important to check for too.
Your vet will closely examine the whole of your dog’s rear legs looking for alternative explanations for your dog’s discomfort. Things like broken toenails, interdigital cysts, thorns, knee issues and the like. Fresh skin abrasions that might indicate recent hip, leg or back trauma are important to check for too.
![]() When your vet guides your dog’s hips through a full range of motion, evidence of pain at the extremes of motion is another major clue. Sometimes, thumb pressure over the joint will elicit (cause) pain. When dysplasia is quite severe, downward traction might cause a popping as the head of the femur separates from the shallow acetabulum (subluxates). The popping sound is call the Ortolani sign. I never perform this test and manipulation without sufficient prior pain-relieving medications.
When your vet guides your dog’s hips through a full range of motion, evidence of pain at the extremes of motion is another major clue. Sometimes, thumb pressure over the joint will elicit (cause) pain. When dysplasia is quite severe, downward traction might cause a popping as the head of the femur separates from the shallow acetabulum (subluxates). The popping sound is call the Ortolani sign. I never perform this test and manipulation without sufficient prior pain-relieving medications.
![]() Properly positioned x-rays of your dog’s hips should tell your veterinarian if your dog has hip dysplasia or will be prone to develop it in the future. Meaningful hip x-rays for dysplasia in dogs always require anesthesia/sedation. In early hip dysplasia small radiographic changes can easily be missed. So, it should be a trained radiologist who reviews your dog’s films. To be of much value, your dog must be positioned just right (exactly) in the x-ray beam. If the dog is even slightly off axis (crooked), it can appear from the x-ray that a hip is abnormal when it is not or vice versa. The diagnostic position for an in-office or OFA hip dysplasia evaluation is the dog with its back on the table, rear legs extended back fully and parallel, knees rotated toward the center line (and the attending personnel shielded from radiation and outside the exposure beam of course). Done right, this should yield an image similar to this one:
Properly positioned x-rays of your dog’s hips should tell your veterinarian if your dog has hip dysplasia or will be prone to develop it in the future. Meaningful hip x-rays for dysplasia in dogs always require anesthesia/sedation. In early hip dysplasia small radiographic changes can easily be missed. So, it should be a trained radiologist who reviews your dog’s films. To be of much value, your dog must be positioned just right (exactly) in the x-ray beam. If the dog is even slightly off axis (crooked), it can appear from the x-ray that a hip is abnormal when it is not or vice versa. The diagnostic position for an in-office or OFA hip dysplasia evaluation is the dog with its back on the table, rear legs extended back fully and parallel, knees rotated toward the center line (and the attending personnel shielded from radiation and outside the exposure beam of course). Done right, this should yield an image similar to this one:
This second image is of a dog with a considerable degree of hip dysplasia. Notice that the ball of each femur is no longer as round as it should be. It is a young dog, so advanced arthritis changes like joint lip proliferation have not yet begun.
With time, inflammation causes the osteophytes, the bone spurs I mentioned earlier, to form new bone at the periphery (edge) of the joint causing pain. The blue arrow points to that advancing process going on:
Hip Certification
High-quality x-rays of young adult dogs can be submitted to OFA where experts will make a judgment as to your dogs’ hip quality. The service was developed in an attempt to lessen the incidence of hip dysplasia in the breeds most prone to it. The service began in 1966. OFA will review x-rays taken by your veterinarian. If your dog is over 4 months old but less than 2 years old, their decisions will be “preliminary”. (read here) When the x-rays submitted are from a dog over 2 years old, the results are a final grade as to your dog’s “hip health” in relation to what they believe to be ideal hip joint conformation.
The University of Pennsylvania School of Veterinary Medicine began an alternative program, PennHIP (the Pennsylvania Hip Improvement Program) in 1993. It is now administered by Antech Imaging Services. The motivation for the PennHIP program was the slow rate with which the prevalence of hip dysplasia was being reduced using the OFA method. (read here) The PennHIP procedure can be employed as early as 16 weeks of age for predicting the likelihood of future degenerative joint changes in your dog’s hips. That might give dog owners time to make diet and lifestyle changes in the hope of delaying the onset of pain and debility in their pet. It might also be a wise procedure to perform when selecting a future service dog. Conscientious dog breeders also have the procedure performed before choosing which dogs to breed as well as to provide reassurance to those that purchase puppies from them.
Unlike the OFA, the PennHIP procedure utilizes three x-ray views of your dog’s hips. Penn requires an x-ray image of the dog’s hip in extended view, a compression view and a distraction view. The three are used to obtain a numerical measurement of hip joint laxity. You can see the three views here. Your dog must be anesthetized, and the procedure must be performed by a veterinarian trained and certified by the program before a hip score (distraction index) can be assigned. Your dog’s distraction score is based on measurements, not the subjective opinion of veterinarians as the OFA method is. See a PennHIP report here. Most veterinarians today believe the PennHIP approach yields more accurate predictions of your dog’s future hip health. The drawbacks are a higher cost and the requirement that veterinarians taking the radiographs be within the PennHIP network. Dog owners who fear anesthesia for their pets might be able shop around and find a vet willing to take OFA x-rays without the use of an anesthetic; that is not the case with PennHIP. Unfortunately, the AKC has no requirement that dogs have good hips. Canine health, a pain-free life and longevity are not among their top priorities. When I must present bad hips or other bad genetic news to my clients, it is common for them to reply, “that can’t be, he/she came with papers !! “.
What Can I Do To Avoid Or Minimize A Potential Hip Dysplasia Problem?
Later Neutering Of Female Dogs And Leaving Your Male Dog Intact
Pediatric spaying of female dogs and castration of male dogs is partially responsible for many of the long-term health problems that plague our dogs. (read here) Hip dysplasia is one of them. (read here) Early-age neutering has profound negative effects on your dog’s bone development and the function of its other organs. Early age neutering also increases the chances of obesity when your dog is fed to its heart’s content (free choice). Every year, more canine health issues related to early-age neutering are added to the list. (read here & here)
Growth Rate And Nutrition
Don’t over feed your puppy or growing dog. Growing dogs are capable of consuming more food than they require for optimum bone structure and health. Too rapid a growth rate and excessively fast weight gain make genetic tendencies toward hip dysplasia worse. When puppies grow too quickly, the structural strength of their bones, joints and ligaments can’t keep up with their rapid increase in body weight, increased muscle mass and strength. Discouraging rapid weight gain will not change your dog’s genetic predisposition to hip dysplasia. But slower progress to adult body weight might delaying the onset of hip dysplasia or its severity. Dietary calcium & calcium/vitamin D supplements have not proven unhelpful. (read here)
Thoughtful, Age-Appropriate Exercise
Your dog needs exercise to keep its hip and leg muscles strong. But do not push your young dog to over-perform. Your dog will do anything to please you, and it cannot tell you when it is pushing the limits of its endurance. You have to look out for its best interests. Dogs that are still growing have developed strong muscles, but their bone and joint structure has not reached its maximum strength. Hip dysplasia is thought to begin with microfractures. (read here) Pups at high risk of developing hip dysplasia need a low-impact lifestyle until the bones of their hips have fully ossified, and their joint conformation is less plastic to deformation. Ligaments and supporting structures of their hip joints (and cruciate knee ligaments) also take at least a year to reach their full potential strength.
For adult dysplastic dogs, walking them on a leash, swimming, or a slow treadmill are all fine. Just don’t overdo it. Your dog should not appear worse the following day. If it does, cut back. When you take your pet for walks, stay on unpaved grassy areas that cushion their steps avoiding hard packed, paved or uneven surfaces. You need to pay close attention to your dog’s toenail length. Toenails of dysplastic dogs tend to overgrow and become a danger in themselves as they twist and distort toe structure. There might come a time when a mobility harness will be helpful as well.
Avoid Obesity
Most large breed dogs love to eat. My Labrador retriever Maxx sure does. When a dog becomes overweight and does not have thyroid issues, it is not a canine problem, it is a human problem. It is always a struggle for me not to equate providing extra food with providing extra love. Resist that temptation as best you can. Carrying extra weight around puts extra stress on the skeletal support of your dog’s whole body. Even if you later decide your dog needs hip surgery, the results are likely to be considerably better if your dog is not overweight. Read more about overweight dogs here.
Padded Bedding And Soft Relaxing/Sleeping Areas
I believe that the worst thing for a dog with hip dysplasia is sleeping on a hard floor. Warm wood floors and carpets often improve matters, but your dog will be most comfortable on an over-stuffed dog bed or something similar. My Labrador Retriever Maxx is now 15 years old. His favorite resting and sleeping areas are two black rubber mats – one large commercial entrance mat placed on top of a similar size ergonomic/anti-fatigue mat (bonded together with Loctite®PLS30 adhesive). (see here) I prefer this to porous cloth or open foam products, for large dogs. They are easy to washed and sanitized and harder for dogs to destroy.
Soothing Warmth
Just as with human arthritis, your dog might experience its most discomfort in cold weather. A warm room, free from drafts with an additional heat source will help. I prefer heating pads that were designed specifically for dogs. A pet sweater when out and about might also be appreciated.
Physical Therapy
Physical therapy and hydrotherapy can go a long way in reducing your pet’s pain and debility when dealing with hip dysplasia. Hire a professional or begin by kneading the muscles around the hips with your fingertips in gentle, circular motions. Gradually work your way around the surrounding muscles. There is an entire science of pet physical therapy, which you can explore online. Begin on YouTube. If there comes a time when it becomes too painful for your dog to climb stairs or go outside to relieve itself there are ways to overcome those issues too. Building or purchasing a handicap ramp can be helpful. When even that is not sufficient, your dog can be paper-trained.
Medications
There are no known medications that will reverse dysplasia-associated hip arthritis in your dog. But hip dysplasia pain and debility can be managed successfully for quite some time with medications. The disease is a form of arthritis; so the same NSAID group of medications that are helpful for us humans suffering from arthritis and joint pain are helpful to dogs too. These are medications that decrease inflammation. But don’t be tempted to reach into your medicine cabinet for medications prescribed for you and give them to your dog. Giving them to your dog could be quite dangerous. At the least, the dose or frequency might be wrong for a dog. At the worst, it might be a particular NSAID drug that dogs do not handle well (such as aspirin, indomethacin (Inodcin®), naproxen/(Aleve®) or ibuprofen/Advil®). It could also be a dangerous medication (contraindicated) for your dog due to other concurrent medical issues that your pet faces. Liquid human medicines can also contain xylitol sweetener. The only NSAID I know of that is sold in the United States for both human and dog use is meloxicam (Metacam® /Mobic®). I am told that the active ingredient in canine Rimadyl®, carprofen, is sold for human use in Europe. Others, like deracoxib/Deramaxx®, firocoxib/Previcox® and grapiprant/Galliprant® are marketed specifically for dogs. Most dogs handle these medications well. When issues do arise, they are usually related to stomach and intestinal tract inflammation that NSAIDs are prone to cause more frequently in dogs than in humans. Always keep that issues in mind. The first sign of a bad reaction to an NSAID in dogs is often a lack of interest in food. Just because a medication works safely in most dogs doesn’t mean it will work safely in your dog. Always read the warnings on the product insert that comes with your dog’s medications. Periodic blood tests when your pet is taking these medications regularly is always a wise thing to do.
Corticosteroids
Corticosteroids, like prednisone and prednisolone, are strongly anti-inflammatory medications. They will relieve arthritis pain. However, given long term, they all have profound undesirable side effects. Those include weight gain due to increased appetite and fluid retention, liver enlargement and dysfunction, elevated blood sugar level, decreased ability to fight infections, slowed healing and a host of other undesirable metabolic effects. I reserve them for end of life situations where dog owners want to be with their pets just a little bit longer.
Tramadol
Tramadol (Ultram®) is a narcotic medication that relieves pain. There are dogs that develop intestinal troubles when given NSAIDs or don’t receive enough relief from them. In those dogs, tramadol might be helpful. It is reasonably priced in its generic form and usually has minimal side effects when given in at the proper dose and interval. Unlike NSAIDs, tramadol can be given in combination with corticosteroids. Its two chief drawback are its lack of effectiveness in some dogs, and the fact the the DEA makes it a challenge for pet owners to obtain.
Gabapentin
Gabapentin (Neurontin®) is another medication that sometimes helps relieve chronic pain. It was originally used in the treatment of epilepsy in humans, where it was noticed that it seemed to also provide some pain relief. In humans, it appeared to be more effective in pain relief due to nerve irritation than to pain due to arthritis or dysplasia. But recent studies seemed to indicate that the drug decreased the pain of arthritis in experimental animals as well. (read here & here) Nociception = the feeling of pain. Gabapentin is inexpensive and has few side effects when given properly. It does not help all dysplastic dogs and when it does, it often takes several weeks before you can expect to see a positive effect.
Nutraceuticals
These are products that are not evaluated by the American Food and Drug Administration (FDA) because they are all considered “foods” rather than “medicines”. It is extremely difficult to find hard scientific data that prove that any of them work or don’t work. Because dogs with hip dysplasia have “good days and bad days” and because dogs can’t talk, it is very hard for anyone to get a handle on their actual effectiveness – if any. Nevertheless, very large amounts of these products are sold. Published reports on their effectiveness when they appear and testimonials tend to be “advertorials” by the companies intent on selling you their wares. Anything that is prefixed by the words “complementary” “amazing” “alternative” “all natural” “miracle”, “breakthrough”, “dramatic” or “veterinarians don’t want you to know” fall into this classification. Anything that claims it helps all dogs with joint-related mobility issues belongs in that bag too. Among those products are antioxidants, fish and krill oils, zinc supplements, polysulfated glycosaminoglycan (e.g. Adequan®), glucosamine and chondroitin (e.g. Cosequin®), hyaluronic acid, omega-3 fatty acids, topical DMSO and Boswellia serrata. Since most of them are probably harmless, I see no problem at all with you giving them to your arthritic or non-arthritic dog in reasonable amounts when other treatment options fail. It is so so hard for you and I to just stand by when we see the dog we love so much in pain. I take vitamins myself.
Platelet rich plasma injections, low-level laser therapy, acupuncture and massage therapy receive at best mixed reviews as to their benefits – although most dogs love a massage and the added attention. (read here & here)
Does My Dog Have Surgical Options?
Yes, some dogs do.
Several types of surgery can sometimes help dysplastic dogs. In adult dogs, these surgeries are designed to eliminate pain and improve mobility. My preference in heavier weight breeds is for a total hip replacement with the surgery put off as long as non-surgical options maintain your dog’s quality of life. In lighter weight dogs, my preference is still a femoral head ostectomy.
In puppies the aim of surgery is to reassemble the joint structure in ways that make hip dysplasia less likely to occur later on. Unfortunately, none of those reconstructive techniques have had adequate long-term studies for us veterinarians to accurately tell you their success rates in relation to other, less drastic measures.
Read more about these procedures below:
Femoral Head Osteotomy (FHO)
Many speak of femoral head removal or osteotomy as a salvage procedure. It is true that your dog’s gait will not likely return to normal. But your dog will usually be pain-free and happy, which is my primary concern. It is a less successful procedure in large and giant breeds of dogs (not as successful in dogs over 45 lbs/20.4 Kg adult weight). To read more about femoral head excision (FHO) go here. FHO serves no purpose when your dog’s hip joint(s) are fully luxated and your pet is already pain-free. It is a great joy to me to see these dogs running pain-free and happy again.
A Hip Replacement
Artificial hip joints (prostheses) perform well in dogs when performed by experienced surgeons. Your dog’s gait often returns to near normal, and they remain pain-free. Some veterinary orthopedic surgeons prefer devices that are bonded to the bone with special cements, others prefer cement-free techniques. One big drawback is expense. The cost, once given to me a number of years ago by Ohio State Veterinary School for the procedure, was $5,600 – $6,000 per hip + $200-$300 per follow-up visit. However, they stated that “Four out of five dogs or 80% of their patients with arthritis in both hips only required that one side be operated upon to return them to a satisfactory and comfortable life”. Veterinary surgeons rarely suggest hip replacements before your dog is fully grown. The hip bones of your dog need to have reached their maximum size, surrounding tissues fully developed and bones fully calcified in order for the prosthetic joint to hold fast and function optimally. Dogs generally stay 3-5 days at the facility after their surgery. After their surgery, activity is generally limited for 2-3 months. This gives time for complete healing. But procedures and techniques differ depending on the individual proclivities (inclinations) and learning experiences of your dog’s surgeon.
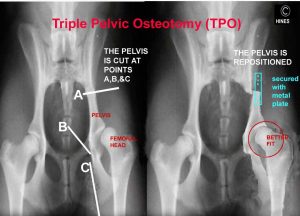
Surgically Changing The Alignment of Your Dog’s Hip Sockets – Triple Or Double Pelvic Osteotomy Or Symphysiodesis (TPO, DPO, JPS)
If a puppy or adolescent dog still has some growing to do, procedures exist that attempt to reassemble your dog’s acetabulum (hip socket) in positions that might promote joint stability. The two most common techniques, TPO and DPO, cut the bone that forms your dog’s hip socket into three or two portions and reassembles them in a new alignment designed to hold the head of your pet’s femur more snugly in the joint socket.
There has not been enough long-term tracking of dogs after TPO, DPO or JPS surgery for veterinarians to be confident in predicting the results of any of the three procedures. The only attempts I know of were done in 2007 and 2010. The first study noted that the procedures had not eliminate hip joint laxity or the progression of hip joint arthritis when examined 2 years after the surgery. (read here) The second study found improvement was still present two years after JPS surgery. Surgical procedures are rarely questioned until something better comes along. In the case of canine hip dysplasia, nothing has. Many university veterinary orthopedic centers and veterinary orthopedists offer the TPO or DPO procedures.
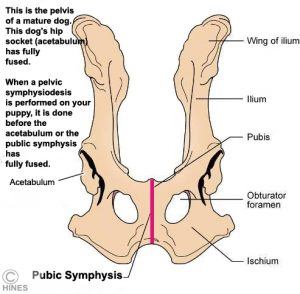
The University of Wisconsin Veterinary School pioneered the symphysiodesis (JPS) technique. In that procedure, one growth plate of your pup’s pelvis (the pubic symphysis) is prematurely prevented from growing – as it normally would until your dog reached its full size. Click on the image above. The red line outlines the pubic symphysis area. Since the other centers for pelvic growth continue to grow, the shape of your dog’s pelvis changes and so do the forces that press the head (ball) of your dog’s femur into the acetabulum (socket). Of the three procedures, this is the least traumatic and least expensive – but I noted that the University of Wisconsin Veterinary School no longer mentions the JPS technique on their website. Instead, they promote only total hip replacements.
Fifteen to 20 weeks of age would probably be the ideal time to perform the JPS procedure. That is a very small window of opportunity. At that tender age, the only reliable method to determine if your puppy needed the procedure would be the PennHIP test that I previously mentioned. TPOs and DPOs are generally suggested between 6 and 12 months of age. If performed on your dog much younger, the pet’s bone structure might not be strong enough to hold the required anchoring screws and plates. When performed much beyond a year of age, self-perpetuating arthritic joint changes and remolding that this surgery cannot correct have already begun. So again, the time window for hoped-for success is quite short.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.