What Diseases Do Ticks Expose My Dog To?
Babesia, Ehrlichia, Anaplasma
Ron Hines DVM PhD
What Diseases Do Ticks Expose My Dog To?
The three I want to tell you about are babesia (babesiosis), ehrlichia (ehrlichiosis) and (anaplasmosis). They are the most common ones that your dog or even your cat could be exposed to in North America. But there are many many others, ticks give a free ride to so many diseases. Veterinarians call all of them tick-borne diseases. All of this group of organisms are spread by blood sucking parasites – usually a tick, but fleas probably have that potential too. (read here) Lyme disease is another one of them. Another is Rocky Mountain Spotted Fever (RMSF). Many are in a group called Rickettsial bacteria. None of these organisms are particular about whom they infect. (read here) It could be your dog, it could be your cat, or it could be you. (read here) In one study, 13% of a group of stray dogs in Louisiana had been exposed to Rocky Mountain Spotted Fever. RMSF is also present in dogs in Canada and in Europe – always spread by ticks.
Ticks spread more than blood parasites. They also transmit tularemia (rabbit fever). Dogs as well as people can catch that disease too. Although ticks transmit tularemia, your dog is more likely to have caught it by coming in contact with wild rodents or rabbits. Tick paralysis is the only tick-borne disease of dogs that is not caused by an infectious organism. Tick paralysis is caused by a neurotoxin that is produced by the ticks themselves. (read here) Another disease organism, hepatzoon, is spread when ticks are accidentally eaten by your dog while grooming. I am always disconcerted when I discover fleas on your dog. But I am mortified when I discover ticks.
I can’t discuss all of these diseases, there are just too many of them. But preventing all of them requires limiting your pet’s exposure to all blood sucking parasites.
How Likely Is It That My Dog Will Be Exposed To One Of These Diseases?
When blood samples were collected from 6,582 dogs and checked for exposure to borrelia, ehrlichia and anaplasma, 18.2% were positive for exposure to at least one of them. The authors looked for antibodies the dogs produce only after encountering these organisms. These were dogs from the USA, Canada and the Caribbean islands. This sort of study is not the most accurate way to decide the true number of dogs that encounter these blood parasites. Some dogs might not have produce sufficient antibodies to detect. But it is the best study we have. Read that article here. Other sources give much lower exposure numbers: 2.22% (of 2,366,999 dogs tested) positive for ehrlichia, 4.21% positive for anaplasma and 6.85% positive for borrelia (Lyme). (see here)
Babesia – Babesiosis
Babesia are microscopic blood parasites, protozoa that cause so many diseases in so many animal species. Over 100 different parasitic babesia species are said to exist – each perhaps preferring (but not confined to) a particular animal species. Parasitologists are always hot to discover a new organism. So, many of these babesia names are probably redundant. It is more likely that it is the tick that chooses who catches these blood organisms rather than the babesia organism themselves. The one that deer mice and their ticks carry (B. microti), occasionally infects humans as well as dogs and cats. (read here) No matter which babesia is involved, once your dog is infected by a tick bite, the parasites live within your dog’s red blood cells (RBCs). In the United States, babesia are primarily spread by the common brown dog tick (Rhipicephalus sanguineous). On very rare occasions, it is possible to spread the babesia through an infected blood transfusions. Once inside your dog’s red blood cells, these parasites reproduce. In the process, they destroy the RBC to liberate their immature parasite offspring (merozoites). The merozoites mature in new RBC that are also eventually destroyed. The result is often anemia. Although much of that anemia is due to the mechanical destruction of your dog’s RBCs some is probably due to your dog’s immune system attacking its own RBCs that it now regards as abnormal or tainted. In addition to anemia, many infected dogs experience abnormally low blood thrombocyte counts. Thrombocytes are an essential part of your dog’s blood clotting process. Babesia disease tends to be more severe in younger dogs and puppies. As I mentioned, there can be many species and sub-strains of babesia that infect dogs. Some are larger than others (e.g. Babesia canis = larger, Babesia gibsoni = smaller). They also appear to vary in the severity of the disease that they produce. But the severity of the disease caused by a single babesia strain is very dependent on your dog’s genetics and the current health of its immune system. Also coming into play is the fact that a tick can infect your dog with several different babesia strains all at the same time. A single tick can even infect your dog with several different tick-borne diseases at the same time. Chronically infected dogs that have been doing a good job in keeping babesia numbers under control can break or relapse with babesiosis when facing multiple new health issues or simple stress. Occasionally, severe babesia infections cause secondary liver and kidney damage.
If My Dog Catches Babesia, What Signs Might I See?
Other than pale gums, the most obvious sign of a severe babesia infection is jaundice – yellowish gums, eyes and skin. In the case of a babesia infection, that is due to the bilirubin released during RBC destruction. However, liver problems that are unrelated to babesia are a more common cause of jaundice. Some dogs with babesia bruise easily, other experience nose bleeds. Some pass rust-tinged urine. Many run fevers. Some have swollen superficial lymph nodes. But many pets just lack energy due to their anemia. However, there are also many dogs harboring babesia that do not show any symptoms at all. They might be dogs whose signs are subtle or progressing slowly or whose babesia numbers are being kept in check by their immune system. Some call those pets “carrier” dogs. They might do just fine until they encounter another health issue that decreases their general immunity. A few of those cases are not discovered until a dog is required to have a splenectomy. The spleen is the home of many of your pet’s immune system cells, constantly patrolling the blood passing through it for pathogens. (read here)
How Will My Veterinarian Know For Sure That It Is Babesiosis?
Most dogs that harbor babesia are brought to their veterinarian because they are in crisis with the severe form. Most have known tick exposures. Those dogs have that dark urine I mentioned earlier, pale gums, jaundice and weakness. Their heart rate is elevated. Your veterinarian can palpate an enlarge spleen in many of them. As I mentioned, often their superficial lymph nodes are enlarged as well (lymphadenopathy). They often run a fever – at least initially. Many have lost weight. Blood tests confirm their anemia. Their blood bilirubin level is elevated. They are often deficient in blood albumin as well. White blood cell counts often show that they lack sufficient thrombocytes (thrombocytopenia). However, none of those signs are specific to a babesia infection. Your veterinarian will have to rule out many other possible causes. Things like ingested toxic substances, kidney failure, autoimmune hemolytic anemia, liver disease and many more.
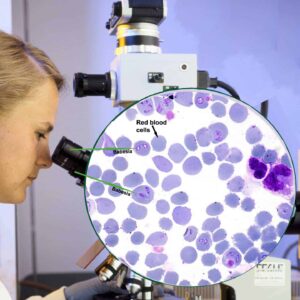
Traditionally, your veterinarian would have examined or send off a stained blood smear, similar to the one in the diagram I drew. If fortunate, with the aid of the microscope the babesia organisms would be visible. But the number of babesia organism in the RBCs of infected dogs cycle up and down in waves. In many cases they might be missed.
So, when organisms cannot be found, or just for the ease and convenience of rapid testing, today most veterinarians either send a blood sample from your dog to a commercial laboratory for a blood parasite PCR panel, or run the in-office Snap combo test you see in the picture above. PCR tests magnify and detect even modest amounts of the unique proteins of babesia and the in-office test detects the presence of several other tick borne diseases as well. None of the these tests are perfect. Manufacturers squabble as to whose test is the most accurate. Whichever company paid for the research always finds their test is the best on the market.
What Are My Veterinarian’s Treat Option?
If your pet is severely anemic (PCV ~15% or less), it will require hospitalization, possibly a blood transfusion, intravenous fluids, perhaps oxygen and 24 hr supportive care. Experienced veterinarians have learned over time to size up your dog’s degree of illness and its need for hospitalization quite well, just based on their visual observations. So, your vet might suggest hospitalization as the safest course of action, even if its anemia is not that severe. In the United States, imidocarb dipropionate (Imizol®, imidocarb) is the most commonly used drug to treat babesiosis. It is a powerful drug that must be given by deep intramuscular injection or subcutaneously and the dog closely observed thereafter. The most common side effects are pain during injection, drooling, vomiting and diarrhea (in that order of frequency). Some vets try to counter these effects with a pre-injection dose of atropine. Occasionally, the drug will negatively affect your pet’s liver as reflected by a rise in its liver enzymes. That usually subsides. A second injection dose is given two weeks after the first. Azithromycin and clindamycin antibiotics are thought by some to also be helpful in resolving clinical cases of babesiosis.
It is unclear if treatments are always effective in completely ridding your pet’s body of babesia. Your dog’s general health generally does improve rapidly (within a week or two). But the species of babesia involved, high-stress environments, nutritional deprivation, kennel stays and a variety of future health challenges that might occur all have been known to cause relapses. Since even a case of babesiosis does not leave your dog with lasting immunity to future infections, it is really impossible to tell the difference between relapse or a new infection from another tick bite. (read here)
How Can I help Prevent My Dog From Catching Babesia?






Are Vaccines Against Babesia Available?
Over the years attempts have been made to develop an effective canine babesiosis vaccine. None that were completely effective were ever found. One, Merck’s Nobivac Piro®, was available for a while in Europe. I believe that it has since been withdrawn from the market. When it was available, it only claimed to lower the severity of your dog’s babesia infection should one occur. Another, Merck’s EURICAN PIRO® is, I believe, still marketed in Spain for dogs. Another, Pirodog®, produced by Boehringer Ingelheim, is also available in some European countries. It is said to shorten the disease duration and reducing the severity of clinical signs. None of them prevent infection, but all appear to some extent to block the development of the symptom. (read here)
Ehrlichia – Ehrlichiosis
Another blood disease that ticks bring to dogs is Ehrlichiosis. There are many ehrlichia bacteria, but the most common one in dogs is Ehrlichia canis. Ehrlichia canis also infects cats and possibly humans as well. (read here) Several common species of ticks transmit ehrlichia. The disease goes by many names: canine monocytic ehrlichiosis (CME), canine rickettsiosis, canine typhus, tropical canine pancytopenia, idiopathic hemorrhagic syndrome, canine hemorrhagic fever and tracker dog disease. It is most common in hot, humid tropical and semi-tropical climates. Whereas babesia live in your dog’s red blood cells, ehrlichia live in its white blood cells. The white blood cells most likely to be invaded by this parasite are your dog’s monocytes.
If My Dog Becomes Infected With Ehrlichia, What Signs Might I See?
Many dogs that harbor ehrlichia subsequent to a tick bite show no signs of illness at all. Veterinarians do not know the factors that lead one dog to become ill while another dog lives in relative harmony with these parasite. Many suspect that it is coinfection with other tick-borne diseases like anaplasmosis, babesiosis or Lyme disease that allow ehrlichia to cause disease. Other, attribute the onset of symptoms to be due to lifestyle stresses, or concurrent other health issues. Still others point to perhaps a genetic susceptibility to ehrlichia disease, particularly in German shepherd dogs. (read here)
When ehrlichia does produce illness, signs are quite variable. Many dog owners just notice a sudden loss of appetite and energy in their pet. With time, that can progress to painful joints, lameness, pale gums, rapid respiration and fever. Like babesia, ehrlichia often causes your dog’s thrombocyte (blood platelets) numbers to drop, decreasing its blood’s ability to clot. So, nosebleeds or easy bruising occasionally occur as well.
How Will My Veterinarian Diagnose Ehrlichiosis In My Dog?
The physical signs of ehrlichiosis are not sufficiently different from babesiosis to tell one from the other. Fever, enlarged lymph nodes (lymphadenopathy), enlarged spleen and joint pain are commonly associated with this disease. As I mentioned, as with babesiosis, there is often a deficiency in thrombocytes – the cells involved in the blood clotting process. Veterinarians are unsure why this is a common symptom in several tick-borne diseases of dogs. As with all tick-borne diseases, it is not that unusual for a dog to be infected with several different species of these bacterial parasites at the same time. Standard canine “tick panels”, offered by a number of commercial laboratories and universities, will detect most dogs that are suffering from ehrlichiosis. Those tests look for antibody the dog produces against the organism. They occasionally give false negative results. When these tests detect ehrlichia antibody, it only denotes exposure – not active disease. So, a confirmatory PCR test for the organisms themselves is a wise choice in those situations.
Most vets in high disease prevalence areas perform the Idexx SNAP®4
What Treatment Are Available When My Dog Has Ehrlichiosis?
Most veterinarians treat this disease with doxycycline (often for about 4 weeks). Minocycline is an alternative when doxycycline is unavailable.
Ehrlichia Prevention
The same prevention suggestions I gave for babesia apply to ehrlichia. Many veterinarians suggest that your dog be tested at their office for tick-borne diseases, including ehrlichia, yearly. That decision needs to be made by you. It depends on the climate where you live and on how likely you feel it will be that your dog will be exposed to ticks.
Anaplasma – Anaplasmosis
Anaplasmosis of dogs is the most recent tick-borne disease to receive special attention from veterinarians. For most of the last 100 years, the focus was on this organism, Anaplasma phagocytophilum, when it affected cattle. (read here) As in cattle, ticks are the primary transmitter of anaplasmosis to dogs. Anaplasmas are a type of rickettsia, ehrlichia is as well. The classification and grouping of these organisms is confusing and ever-changing. A variety of biting insects such as fleas and mosquitoes are probably capable of spreading this organism too. Those routs of transmission have been confirmed for other rickettsial diseases of animals and humans. Anaplasma and ehrlichia are closely related. In fact, the common anaplasmas affecting dogs, Anaplasma phagocytophilum and Anaplasma platys, were once considered to be ehrlichia. (read here) And like ehrlichia, they have wild animal reservoirs other than dogs. Humans occasionally contract Anaplasma phagocytophilum too (HGE). But an infected household dog free of parasites is no threat to you. The disease only move from one host to another through insect bites or blood contamination of a wound. Cats are at risk as well.
Of these three diseases I mention, babesiosis, ehrlichiosis and anaplasmosis, anaplasmosis tends to be the mildest in dogs. It is often described as “self-limiting”, meaning most dogs overcome the infections without treatment. The few that continue to harbor the organisms usually become normal-appearing (asymptomatic) carriers. Much depends on your dog’s own unique immune system and the strength (virulence) of the particular anaplasma strain it encountered. (read here)
What Signs Might I See If My Dog Develops Anaplasmosis?
There have been no large studies in America. But in one small study in the Netherlands, only two out of 6 infected dogs showed any outward signs of illness. (read here) When dogs do show signs of illness, it is usually confined to a lack of energy and interest (general malaise & lethargy), decreased appetite and perhaps a transient fever that resolves over a week or two. But on occasion, signs of anaplasmosis can be considerably more severe. When they are, the signs mimic the signs of the more pathogenic ehrlichia. (read here) Those cases often involve infection with more than one tick-borne diseases at a time.
How Will My Veterinarian Diagnose Anaplasmosis In My Dog?
When the history you provide to your veterinarian and the typical symptoms I mentioned for the first two diseases are present in your dog, your veterinarian will run an in-office or send-out test that indicates exposure to all of them. That includes anaplasmosis. As I also mentioned earlier, it is not unusual for a dog to be infected with more than one of these diseases simultaneously. In severe cases, and often when the tick(s) transmitted more than one disease – the same laboratory blood test results of a low blood thrombocyte counts, a low lymphocyte counts and an elevated liver enzymes are likely to be present. An occasion dog with anaplasmosis will show symptoms of painful joints as well.
What Treatments For Canine Anaplasmosis Are Available For My Dog?
Antibiotics of the tetracycline class, such as doxycycline are usually quite effective in reliving the symptoms of anaplasmosis and other tick-borne diseases. As with ehrlichia, one cannot always be certain that every last anaplasma has been eliminated from your dog’s body. The most certain way to confirm your dog’s status with more confidence is to run a post-treatment PCR test. Dogs that do not improve rapidly on drugs like doxycycline need to be evaluated for other health issues that might be suppressing their immune system. (read here)
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.