Kidney Disease In Your Dog And Cat
Chronic Renal Problems Chronic Renal Failure (CRF), Chronic Renal Insufficiency (CRI)
Ron Hines DVM PhD
All of our bodies suffer the wear and tear of time. In dogs and cats, it is often their kidneys that wear out first. There is a slow but steady and natural loss of kidney function throughout their lives. It is significant enough to make chronic kidney disease the second leading health issue in older dogs and cats. The first is arthritis.
What Happens When My Pet’s Kidneys Begin To Fail?
First, you need to know something about how your pet’s kidneys work. Kidneys keep your pet’s body free from excessive amounts of the wastes that naturally accumulate during metabolism. Veterinarians measure two of those wastes, BUN and creatinine, in your dog and cat, but there are many more. Your pet’s body also continuously monitors your pet’s blood levels of salts (electrolytes) minerals and water. When some essential component of your pet’s body is in short supply, its kidneys are “informed” of that and do their best to prevent those elements from leaving in the urine. (read here) For example, your dog or cat’s urine is darker and more odorous when your pet is dehydrated because its kidneys are letting as little water escape from the body as they can. The opposite is also true, kidneys attempt to excrete more when compounds in the body are in excess.
The actual removal of waste occurs in tiny filtering units within the kidneys called nephrons. Some of the escaped elements are later reabsorbed farther down the tubular system. There are almost one million of these structures in a single human kidney. No one has ever counted them in dog or cat. Each of those many nephrons contains a small sieve-like filtering structure called a glomerulus. These glomeruli hold back normal blood proteins and blood cells while allowing excess fluid and wastes to pass through to end up in your pet’s urine. A complicated chemical exchange takes place as waste materials and water leave the blood and enter the urinary tract. Kidneys also regulate your pet’s body’s acidity. Through regulation of body salt content, they help control its blood pressure too. Cells associated with healthy kidneys also produce an important hormone called erythropoietin and an enzyme called renin. Erythropoietin is necessary for your pet’s body to produce and maintain red blood cells while renin activates another hormone (angiotensin) to helps control your cat or dog’s blood pressure. In addition, healthy kidneys are required to process vitamin D3 into its active form, calcitriol. Calcitriol is essential to preserve the proper balance of calcium to phosphorus in your pet’s bones and blood stream. In chronic kidney disease all these processes break down due to inflammation and scarring
But My Pet Is Still Producing Plenty Of Urine – More Than Before!
Your dog and cat’s body is marvelous in sensing when it has a chronic kidney issue. In an attempt to keep its body’s waste level down, your pet’s kidneys work overtime, using whatever remaining capacity they still have to remove as much waste as possible. That means that its remaining functional glomeruli must flush more body water through the system. That accounts for the excess thirst and urination you probably see in your pet. For a while, that compensates and keeps its body free enough from toxic wastes to function. But over time, too many glomeruli have been lost, and your pet can’t consume enough water to keep its waste levels in check. By that time, your dog or your cat probably experiences weight loss, anemia, and abnormal blood work results. When that occurs, over half of its kidney glomeruli have already been lost. Pet and people cannot replace them. Glomeruli never regenerate. At least not with the tools that veterinarians and physician have today.
What Are Some Common Signs Of Kidney Disease In Pets?
The first signs that there might be a kidney problem is usually excessive drinking and urination. It is normal for pet owners to ignore this at first. It might be that your dog began to whine at night asking to go outside. Or it might be that your cat’s litter box is damper and smellier than it used to be. Your cat or dog’s water bowl might have to be filled more often than it used to. But with time, your pet also begin to lose weight and become a more finicky eater. About this time, it is common for your pet’s energy level to decrease. It might sleep more and end its play sessions earlier. Most veterinarians associate those signs with metabolic toxins building up in your cat or dog’s body. Often your pet’s hair coat begins to lack the luster it once had. Unless you are into yearly “wellness” checkups, this is usually the point where concerned owners take their pets to see their veterinarian. In more advanced kidney disease, dogs and cats have little interest in eating. Coaxing them to eat with tuna or salmon juice might work for a while. You might even experiment with Entyce®. or Elura®. Pets in this stage of kidney disease often develop digestive tract disturbances such as nausea, retching and diarrhea. Their water intake then decreases, and they often become dehydrated. These pets might stand over their water or food bowl without attempting to eat or drink. These pets have all developed uremia – an intolerably high level of nitrogen-containing metabolic waste products in their blood. Because many of these toxic waste products contain the azo-molecular grouping of nitrogen, another name for uremia is azotemia.
Why Did This Happen?
Veterinarians know the things that make your dog or cat’s kidneys fail suddenly. We are much less certain why kidneys fail gradually. Many causes have been proposed that seem logical. But none of them have been scientifically proven to be true. There are probably a number of factors involved. But regardless of the cause(s), all cases of chronic kidney disease develop similar microscopic signs and pass through similar stages. However, how rapidly the problem progresses is highly variable. Usually, your veterinarian will just tell you that your pet has CRF (chronic renal failure). That is because in most cases, there is no way for your veterinarian to determine the cause.
The Wear And Tear Of Time
There was a time – not so long ago – when infectious diseases and dietary deficiencies ended the lives of dogs and cats early. But with advances in pet nutrition, vaccination, antibiotics and sophisticated surgery, our cats and dogs now live much longer. Nothing lasts forever, and I mentioned that every organism has its weakest link. Unfortunately, the critical cells of your pet’s kidneys (the podocytes) cannot replace or regenerate themselves the way essential cells do in your pet’s liver, blood, bone, skin or cornea. Once a glomerulus ceases to function, it is lost forever. New ones never take its place. The passage of time is probably the most common cause of kidney failure in dogs and cats. Cats in the wild and the wild ancestors of your dog did not live as long as our housepets do. Nature designed their kidneys to match their normal lifespans.
Polycystic Kidney Disease
Some cats and dogs were destined from birth to loose kidney function too early in life. These pets inherited genes that cause fluid-filled sacks (cysts) to form within their kidneys. As these cysts gradually grow in size, they crowd out and destroy the functional tissue (the glomeruli) within your pet’s kidneys. This is an inherited problem in certain purebred cats. (read here) It is much less common in dogs, but there are reports of the disease occasionally occur in dogs too. (read here)
Chronic interstitial Nephritis
Chronic interstitial nephritis is the most common form of kidney damage found in older dogs. It occurs less frequently in cats. Nephritis is a pathologist’s term for inflammation of the kidneys. The tissue that surrounds each nephron filtering unit is called the interstitial tissue. It is the matrix in which the nephrons are suspended – much like stars are suspended in space. Pathologists that examine kidney tissue from pets with failing kidneys have noticed that many have a higher than normal number of inflammatory cells present in these interstitial areas. This low-grade, chronic inflammation is thought to cause the scaring that eventually destroys most of the nephron filters.
An acute (sudden) nephritis with similar results can occur in dogs that have become infected with leptospirosis. Leptospirosis is diagnosed much less frequently in cats. Some veterinarians believe that after the acute phase of this disease, the organism responsible can lingers for long periods in a pet’s kidneys and, in some cases, causes chronic interstitial nephritis. However, most dogs with chronic interstitial nephritis show no evidence that they were ever infected with leptospirosis. Pets suffering from chronic interstitial nephritis have small, shrunken, hard kidneys due to the scarring. If your pet is not too chubby, it is easy for your veterinarian to palpate and identify these shrunken, lumpy, hard kidneys during a routine veterinary visit.
Over-stimulation Of Your Pet’s Immune System
Your pet’s kidney glomeruli act as a sieve, straining and filtering all the blood that passes through them. In a typical day, the entire blood content of your body passes through your kidneys about 60 times. I assume that is not much different in your dog or your cat. Large molecules present in the blood have a tendency to become lodged in kidney glomeruli (sieves). Some of these large molecules are antibodies that are combined with antigens (immune complexes). Many chronic infectious, allergic and autoimmune diseases of dogs and cats produce these immune complexes. They include Lyme disease, chronic skin infections, chronic intestinal disease, overactive adrenal glands (Cushing’s disease) and diabetes. The inflammation of periodontal disease is also associated with kidney disease – at least in humans. (read here) Perhaps a similar connection occurs in our dogs and in our cats. Veterinarians do not know.
The most common form of heart disease in dogs is mitral valve disease. We do not know for sure if heart valve disease is a risk factor for kidney disease in your dog or cat. But when bacteria are involved, they have the potential to break loose from the heart valves and lodge in the kidneys. (read here)
A type of destructive protein sometimes accumulates in the kidneys. It is called amyloid (amyloidosis). In some cats, it is a genetic disease. But it is also known to occur subsequent to over-stimulation of the immune system. Abyssinian and Siamese cats and shar-pei and akita dogs all have a higher than normal incidence of amyloidosis leading to kidney failure. A similar form of kidney damage in pets can occur in autoimmune diseases In these diseases, run-away antibodies are produced against the pet’s own body. In some cases, these autoantibodies are directed at the pet’s kidneys themselves, in others, they may only accumulate there causing physical damage. The most common form of autoimmune disease in dogs is the skin form of pemphigus it tends to occur as a depigmentation and inflammation around your dog’s nose, eyes and anus (mucocutaneous junction disease). Those run-away large antibodies also pass through your pet’s kidneys. What damage if any that they cause there is unknown. Dogs and cats with autoimmune issues often have elevated Coombs and ANA tests.
Hyperthyroidism In Cats
An overactive thyroid gland (hyperthyroidism) is a common problem in older cats. Veterinarians are uncertain why it appears to be occurring more frequently these days. But we know that hyperthyroidism often occurs in cats concurrently with kidney disease. Perhaps that is due to the high blood pressure hyperthyroidism is associated with. High blood pressure can lead to kidney failure. Hyperthyroidism often masks the early signs of kidney failure that I mentioned earlier because hyperthyroid cats generally drink a lot. It is only when your veterinarian resolves your cat’s thyroid problem that it becomes apparent that the cat’s kidneys are failing as well. So, your veterinarian is likely to do extensive kidney function tests on your hyperthyroid cat before deciding if it would be wise to treat the disease or leave things as they are.
Lower Urinary Tract Disease In Cats
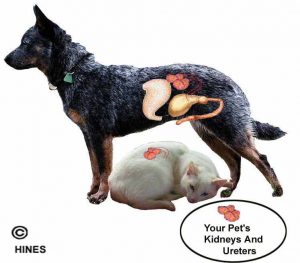
Feline Urological Syndrome (FUS) is another common disease of cats. In that problem, a pasty grit (struvite or oxalate crystals) irritates and sometimes plugs your cat’s urethra preventing normal urination. When the urethra is partially or completely plugged and your cat cannot pee, urine pressure builds up in its bladder, progresses up its ureters tubes to its kidneys, and then into the kidneys themselves. That abnormally high urine pressure, if not resolved, will slowly destroy the kidneys. Increased internal kidney pressure causes hydronephrosis.
How Will My Veterinarian Diagnose Kidney Disease In My Dog Or Cat?
The history you give your veterinarian, your pet’s age and its physical examination will likely prompt your vet to add a potential chronic kidney problem to your pet’s possible health issues. I mentioned that as kidneys scar, they become hardened, smaller and lumpy. In lean pets, they have a characteristic feel when felt through the abdominal wall. But even when those signs of kidney issues are present, your veterinarian will suggest blood tests because those signs are only present in very advanced kidney disease. Blood and urine tests that warn of kidney damage are included in all standard veterinary laboratory examinations. They are also included in what veterinarians call yearly “wellness tests”. For normal test results in dogs and cats, go here.
Your Dog And Cat’s Urine Specific Gravity
When your veterinarian asks you to bring in a urine specimen from your pet, its urine specific gravity will most likely be checked. Specific gravity (=SG, Usg, etc.) tells your veterinarian how concentrated the urine sample is. Pets that have kidney issues have difficulty producing concentrated urine, so the SG of their urine will be low. The lower the specific gravity of first-of-the-morning urine, the more serious the kidney problem is likely to be. However, anything that causes your pet to drink excessively will also lower its urine specific gravity. That is why it is wise to collect your pet’s urine specimen as soon as possible after it wakes up in the morning – before it has consumed water. For certain other urine analyses, it is much better if your veterinarian collects the sample because urine at room temperature for more than 30 minutes gives inaccurate results.
Urine Protein Content And Microscopic Urine Examination
Failing kidneys leak blood proteins into your pet’s urine. Most of that protein is albumin. However, the most accurate test for early kidney issues in not a urine protein test, it is a urine microalbuminuria test. A higher than normal microalbuminuria protein reading is often a very early sign of sudden or long-term kidney damage. The presence of white blood cells and bacteria in your pet’s urine sample can help your veterinarian tell the difference between a sudden (acute) kidney/urinary tract infection and chronic (long-term) kidney disease.
Blood Urea Nitrogen (BUN)
Blood urea nitrogen, is a waste product of metabolism. It rises in the blood of pets with failing kidneys. BUN level normally stays within a relatively narrow range in the blood of pets with healthy kidneys. BUN level in the blood of pets begins to rise when not enough healthy kidney tissue remains to excrete it into your pet’s urine. The higher its level in the blood – the more serious your dog or cat’s kidney problem is likely to be. Blood urea nitrogen and creatinine levels are the prime ways veterinarians decide if their treatment for kidney disease in your pet is working. You will probably have many of these tests run on your cat or dog during its therapy.
Blood Creatinine Level
Creatinine is a protein metabolite of muscle that tends to rise and fall in tandem with BUN. However, blood creatinine determination is a more accurate test for kidney disease than BUN determination because blood levels of creatinine do not fluctuate as much as BUN. BUN can rise in response to dehydration or consuming a high-protein meal. So, BUN and Creatinine tests are almost always run together. The results are often expressed as a BUN:Creatinine ratio.
Blood Phosphorus & Calcium Determination
Phosphorus is one of the mineral constituents of blood. The meat-based foods your pet consumes are very high in phosphorus. Failing kidneys have difficulty excreting sufficient excess phosphorus into the urine. An elevated blood phosphorus level is often another sign of advanced-stage kidney failure. As the ratio of phosphorus to calcium in your pet’s blood becomes abnormal, its bones will weaken. That is why pets in kidney failure need to be fed diets that are low in phosphorus. Pets with kidney damage may also lose their ability to produce calcitriol. When that occurs, they can no longer absorb sufficient calcium from the foods they eat.
Potassium
A proper body level of potassium is very important to your pet’s well-being. When your dog or cat’s kidneys fail, its body potassium level tends to rise. This problem, called hyperkalemia. It causes generalized fatigue, nausea and an irregular, slow heartbeat that can be life-threatening. However, when pets with advanced kidney disease lose their appetites, their blood potassium level can actually fall dangerously low. That is another reason your dog or cat in kidney therapy needs periodic blood tests.
Packed Cell Volume (hematocrits, Hct, PCV)
Your cat and dog’s packed red blood cell volume (PCV) is a measure of possible anemia. A low Hct also indicates that. When a pet with kidney failure has a PCV that is abnormally low, it is not manufacturing sufficient red blood cells. One of the hormones involved in red blood cell manufacture is produced in your pet’s kidneys. It is called erythropoetin. When your pet’s kidneys deteriorate, not enough of that hormone is being produced.
Blood Pressure
Your veterinarian will probably also measure your pet’s blood pressure. Obtaining an accurate reading in cats and apprehensive dogs is extremely difficult in a hospital setting. Read about that here. Many veterinarians believe that it is common for pets with chronic kidney disease to also have abnormally high blood pressure that needs to be managed with medication. However, it is unclear if the high blood pressure is part of the cause of kidney damage, or the result of kidney damage. High blood pressure is known to damage kidneys – but kidney disease is also known to elevate blood pressure. That is called secondary hypertension.
What Treatment Options Do I have For My Cat Or Dog?
In the future, we may be able to regenerate failing organs. But for now, there is no known way to mend damaged kidneys. What veterinarians can do is to try to slow the rate at which your pet’s kidney tissue is lost and deal with the side effects of the loss. Kidney failure is progressive – that means that with time it will get worse. The key to gaining time for your pet is to use its remaining kidney tissue as efficiently as possible. We try to do that through diet, medications and, when necessary, fluid injections (diuresis). Read some of the links at the beginning of this article for more detailed information about that.
A Special Diet
Prescription diets, designed for kidney failure in dogs today are not true low-protein diets. They are lower lower in protein (~2/3 the amount of protein) and sodium found in standard dog foods. It is even harder to safely lower the amount of protein in cat food. To thrive, cats require more protein than dogs. Manufacturers also add omega-3 and omega-6 fatty acids and compounds like potassium citrate to counteract body “over-acidity” and these diets are drastically lower in phosphorus. Your pet’s health on protein restricted diets needs to be monitored carefully. Blood tests need to be done periodically to be sure that the pet’s blood protein levels have not dropped too low and that the dog or cat’s body weight remains stable. When you do that, and your pet’s BUN and Creatinine levels drop or remain stable, protein restriction is probably a positive step. But there are periods in a pet’s ongoing fight with kidney disease when restricting protein might not be a good thing to do. For example, when 7/8th of a group of dog’s kidney was removed experimentally, dogs fed low protein diets actually died sooner. Cats do not tolerate true low-protein diets well at all. It is wiser to depend more on added fat and fiber for dilution of the cat’s protein consumption rather than a large amount of added plant carbohydrates. Ketoacids, as sold through body building outlets, can also act as a substitute for dietary protein in certain instances. But I know of no veterinarians who use those types of diets in dogs and cats.
Always make your pet’s dietary changes gradually.
No matter what you decide to feed, we always want to limit your pet’s consumption of phosphorus. The foods naturally highest in phosphorus are the common high-protein foods, meat, poultry, fish, dairy products, peas and beans. Limiting the amount of sodium your pets ingests is also wise when its kidneys are failing – so commercial-prepared kidney diets limit the amount of sodium-rich ingredients in their foods. They also add omega-3 and omega-6 fatty acids that are found in cold-water fish and fish oils combined with flax seed. In advanced kidney disease, when your pet’s BUN is over 60 mg/dl, most vets believe that moderately restricting protein in your pet’s diet does become important.
Vitamin Supplements
Pets with kidney problems often have poor appetites, weight loss and anemia. They might suffer digestive disturbances as well that could limit their absorption of vitamins. So B-vitamins are often given as appetite stimulant and to ward off any deficiency.
ACE Inhibitor Medications
An organ as basic as the kidney does not appear to vary much between mammals. Experiments in kidneys disease are most acceptable to animal welfare advocates these days when they are done in rats. The cells that researchers zero in on in declining kidney function are the podocytes, cells in the kidney’s filtering apparatus that underlie its blood-cleansing abilities. Once podocytes loss begins, like a tree, bent to a severe angle by a storm – it will continue to slowly fall even after the wind ceases even though the remaining filers “super nephrons” enlarge (hypertrophy) and work harder. There is considerable evidence that medications called ACE inhibitors can slow that loss. The ACE inhibitor most often chosen for pets are benazepril and enalapril. If your pet is placed on an ACE inhibitor, it is wise to be sure that its blood creatinine levels do not increase. In later kidney failure when the remaining kidney filters (glomeruli) are filtering way above their normal capacity, ACE inhibitors occasionally drop the kidney’s internal pressure so low that the pet’s uremia actually worsens. The best monitoring test in those situations is a 24-hour creatinine clearance test or another test that estimates your pet’s GFR.
Phosphorus binders
Certain compounds called phosphate binders can block the absorption of phosphorus from your cat’s foods while it is still within its digestive system. At one time, aluminum hydroxide was suggested. Dietitians now think that more modern products that are free of aluminum are safer. Some common ones are calcium acetate (PhosLo®), sevelamer (Renagel®) and Epakitin®. There are others. (read here)
Calcitriol
Since pets with advanced kidney disease may not produce adequate amounts of active vitamin D3 in their kidneys, the preformed compound, calcitriol, has been occasionally given to them. It is generally given when your pet’s blood calcium to its blood phosphorus ratio become significantly abnormal. Too much calcitriol or vitamin D supplementation can be toxic.
Potassium Supplements
Potassium supplements (Tumil K®, etc.) help when the pet’s blood potassium level drops too low. This sometimes helps combat the listlessness and weakness that accompanies advanced kidney failure.
Erythropoetin – Red Blood Cell Growth Factors
Sold as Epogen®, Betapoietin® or Eporel®, these compounds encourage your pet to produce red blood cells and so combat anemia. Because these compounds were bioengineered for humans, dogs and cats eventually cease responding to them. But they might raise your pet’s PVC for a short time. There is a danger in giving these product. When your pet’s immune system decides to attack human erythropoetin as a foreign protein, it may not only destroys the human erythropoetin that was given – it might also destroys the pet’s natural erythropoetin. That would make the anemia even worse. I would only consider giving erythropoetin in a last ditch effort to gain a bit more quality time with your cat or dog. I personally would be looking more closely at the quality of life than the extension of life.
Fermentable Fiber
Fermentable or soluble fiber, when added to a pet’s diet, also helps remove toxins from its body. Because of this, it is often an ingredient in prescription diets marketed to manage kidney failure in dogs and cats. In these diets, the source is sugar beet pulp. Beet pulp is sold in quantity to stables as a horse feed additive.
Fluid Administration
There comes a time with all pets when they no longer drink enough water on their own to fully utilize their remaining kidney capacity. Early in this period, you can give your pet additional fluids orally or add additional liquid to its food. When that is no longer sufficient, the fluids needs to be given periodically under the pet’s skin by injection. The effect is called diuresis. Its effect in flushing out lowering blood toxins from your pet can be dramatic. Many owners learn how to administer these subcutaneous fluids at home. In most cases, there is no benefit in giving them intravenously. Pets with failing kidneys do need emergency intravenous fluids when they are presented severely dehydrated to veterinarians.
How Much Longer Will My Cat Or My Dog Live?
That is completely dependent on the level of toxins in your pet’s blood. Pets with blood creatinine levels below 2.8 mg/dl usually do well for long periods. Pets with blood creatinine levels of up to about 4 mg/dl have also survived happily for many years with appropriate treatment. But when your pet’s creatinine levels exceed 5, the quality of its life has become quite poor. Creatinine levels of 5 and above mean that 80-90% of their kidneys have been destroyed. It is possible to keep these pets alive – but I question the kindness of doing this. Your pet loves you very much. But it is a two-way street – it is relying on you to end its life peacefully and humanely when that time comes.
Kidney Transplants
Kidney transplants are an option for cats if you are fortunate enough to be able to afford them. They are much more successful in cats than in dogs. Currently, a little more than half of the cats that have had a kidney transplant survive for an additional six months. Of those that do, a few have lived an additional three years. Transplantation surgery in cats is still in its infancy. Success rates generally go up as a specific veterinary center gain more experience with the procedure. Success rates vary from one veterinary center to another. It is not just the expertise of the surgeon that accounts for this. Some Centers are willing to attempt transplant surgery on cats that are already quite seriously ill. In those cases, their overall success rate will be lower than at Centers that confine their surgery to cats in earlier kidney failure.
Dogs do not fare as well with kidney transplants. The greatest obstacle to kidney transplantation in dogs is rejection of the new kidney. Powerful immunosuppressive drugs must be given to these dog for the rest of their lives. These drugs have serious side effects of their own. Centers that once performed the procedure on dogs have now ceased to do so. But others are always beginning programs that attempt to get around the hurdle of rejection in novel ways. I would not let my dog take part in these experiments.
Is Hemodialysis An Option For My Pet?
Hemodialysis, as performed on humans with failing kidneys, is not performed frequently in dogs or cats. The veterinary school at the University of Florida once released as press report of a successful hemodialysis procedure in a dog. I do not know if other veterinary centers that are attempting it, but there probably are a few. When veterinarians attempt hemodialysis, they are more inclined to do so for fixable events such as drug overdoses, toxin consumption or acute kidney trauma than to attempt long-term dialysis to prolong the life of a dog in kidney failure. Perhaps one might use hemodialysis as a temporary delay method until a kidney transplant could be performed on your cat, or perhaps to improve the likelihood of it surviving the transplant surgery when it did get performed. I have never tended to a client cat in that situation.
I Am Desperate – What About New Experimental Drugs, Homeopathic Remedies, Acupuncture And Other Unproven Treatments?
There will always be a few veterinarians offering those services. They are lucrative and people demand them. A few novel legitimate medications that are being administered by veterinarians to pets in kidney failure might some day be proven to be beneficial. The only way we make discoveries is through experimentation. However, the majority of these new treatments will be found to be ineffective. If traditional medications and procedures are no longer helping your dog or cat, there is no harm in trying an experimental therapy – as long as it does not prolong your pet’s suffering. Things that are sold over the Internet to desperate pet owners and and that make marvelous claims are always worthless. The ones that Google might choose to advertise on this webpage based on your browsing history are no better. I will block any you notice.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.